Advances in Diabetes & Endocrinology
Download PDF
Research Article
Microalbuminuria in Type 2 Diabetes and its Relationship with Glycosylated Hemoglobin
Ferdousi S1, Nasreen T2, Md. Islam S1, Md. Rahman Q1, Selim S3, Paul D1, Ahmed MU4* and Sultana T1
1Department of Laboratory Medicine, Bangabandhu Sheikh Mujib
Medical University, Bangladesh
2Transfusion Medicine and Clinical Haematology Department,
BIRDEM General Hospital, Bangladesh
3Department of Endocrinology, Bangabandhu Sheikh Mujib Medical
University, Bangladesh
4Masters in Microbiology, Bangladesh University of Professionals,
Bangladesh
*Address for Correspondence: Ahmed MU, Masters in Microbiology, Bangladesh University of Professionals, Dhaka, Bangladesh
Submission: 20 April, 2018
Accepted: 01 October, 2019
Published: 04 October, 2019
Copyright: © 2019 Ferdousi S, et al. This is an open access article
distributed under the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited.
Abstract
Background: Microalbuminuria is the most common aetiology
of chronic kidney disease. Optimum glycemic control reduces the
development and progression of diabetes-related complications and
there is evidence that improved glycemic control improves outcome
in diabetic subjects.
Objective: This study was designed to know the relationship
of glycosylated hemoglobin (HbA1c) level with microalbuminuria
and normoalbuminuria in type 2 diabetic patients and its relation
to diabetic nephropathy. Materials and methods: This study was
conducted at the Department of Laboratory Medicine (Clinical
Pathology) in collaboration with Endocrinology department (BSMMU),
Dhaka. In this study, HbA1c level and urine microalbumin level of 60
type 2 diabetic patients were measured. Both levels were measured
by biochemical auto analyzer (Siemens Dimension RL Max).
Results: Urinary microalbumin, HbA1c levels were significantly
higher in the cases. Microalbumin levels were linearly correlated to the
duration of diabetes and HbA1c.
Conclusion: Impaired glycemic control is associated with
significant elevations in urinary microalbumin levels. Furthermore, there
is an increased urinary microalbumin levels with increased duration
of diabetes, which suggests that the detection of increased urinary
microalbumin levels at the initial stage can avert, reduce the clinical
and economic burden of diabetic complications in future.
Introduction
Diabetes mellitus is a clinical condition characterized by
increased blood glucose level (hyperglycemia) due to insufficient
or inefficient (incompetent) insulin [1]. The incidence of diabetes
is rising. As a result, Diabetic nephropathy is more common now a
days and an important cause of morbidity and mortality in chronic
kidney disease and End-Stage Kidney Disease (ESKD) or failure [2].
Improved glycemic control has been demonstrated to reduce micro
and macro vascular complications in patients with diabetes. Glycated
hemoglobin (HbA1c) is the preferred and widely utilized biomarker of
glycemic control in subjects with diabetes with higher concentrations
of glucose [3]. Diabetic nephropathy is defined by increased Urinary
Albumin Excretion (UAE) in the absence of other renal diseases. It
is categorized into two stages: microalbuminuria (UAE ≥ 20 microg/
min and ≤ 199 microg/min) and macroalbuminuria (UAE ≥ 200
microg/min). Hyperglycemia, increased blood pressure levels and
genetic predisposition are the main risk factors for the development
of diabetic nephropathy [4]. HbA1c is currently accepted as the most
informative biomarker of glycemic control in subjects with diabetes
and is highly prognostic for long-term diabetes-related complications
such as Microalbuminuria [5].
Materials and Methods
This cross sectional study was conducted at the Department of
Laboratory Medicine (Clinical Pathology) in collaboration with Department of Endocrinology, BSMMU, Dhaka. Total 60 subjects
of type 2 diabetes mellitus were included. Urinary microalbumin
levels and HbA1c in all type 2 diabetic patients were measured.
Urinary microalbumin was measured by microalbumin (MALB)
method which had been based on a particle-enhanced turbidimetric
inhibition immunoassay (PETINIA) in biochemical auto analyzer
(Siemens Dimension RL Max). Other types of diabetes, patients with
UTI/ Pyelonephritis, patients who were on long term diuretics, with
malabsorption or chronic diarrhea, on dialysis were excluded.
Result
Total 60 subjects of type 2 diabetes mellitus were included.
HbA1c level and urine microalbumin level were measured. After
performing microalbumin in urine, patients were grouped into
normoalbuminuria and microalbuminuria. Finally correlation
coefficient of HbA1c and urinary microalbumin was calculated by
using Pearson’s correlation coefficient test.
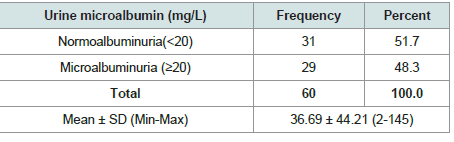
Table 1 shows urine microalbumin of the study patients, it
was observed that 29(48.3%) patients had microalbuminuria and
31(51.7%) normoalbuminuria. The mean microalbumin level was
found 36.69 ± 44.21 mg/L with range from 2-145 mg/L.
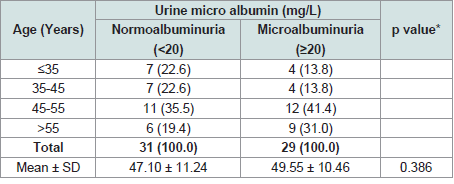
Table 2 shows the age distribution of study population. The mean age was found 49.55 ± 10.46 years in microalbuminuria group, 47.10
± 11.24 years in normoalbuminuria group and. The difference was
statistically not significant (p>0.05) between two group.
Figure within parentheses indicates in percentage.
Table 3 shows comparison between sexes with urine
microalbuminuria, it was observed that almost half of the male
patients 15 (51.7%) patients were male in microalbuminuria group
and 20 (64.5%) in normoalbuminuria group. The difference was
statistically not significant (p<0.005) between two group.
Figure within parentheses indicates in percentage.
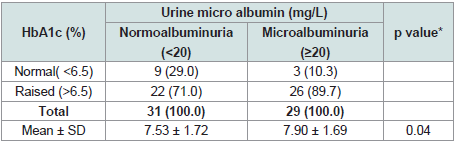
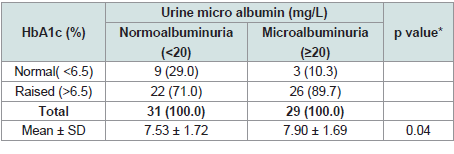
Table 4 shows distribution of the patients HbA1c by urine micro
albumin. 26(89.7%) had raised HbA1c in microalbuminuria group.
22(71.0%) had raised HbA1c in normoalbuminuria group. The
difference was statistically significant (p<0.05) between two groups.
Discussion
Microalbuminuria includes a range of urinary excretion of
albumin of 20 to 200 mg/L or 20 to 200 μg/min [6]. The causes of
microalbuminuria include short term hyperglycemia, exercise,
urinary tract infections, marked hypertension, heart failure, acute
febrile illness, dehydration. Some others condition that damage
glomerulouscauses microalbuminuria and then progress toward
microalbuminuria to proteinuria. Such conditions are hypertension,
diabetes, vasculitis etc [6,7]. The findings of this study is compared
with the results of some other published articles elsewhere in the world
to verify the results. In this study, urinary microalbumin level was measured in sixty subjects of type 2 diabetes mellitus. It was observed
that 29(48.3%) patients had microalbuminuria and 31(51.7%)
normoalbuminuria. The mean microalbumin level was found 36.69
± 44.21 mg/L with range from 2-145 mg/L. Xu B et al. (2013) had
shown that 11.37% of the study population had Microalbuminuria
[8]. In another study done by Varghese et al. (2016) found that
overall prevalence of microalbuminuria 36.3% [9]. So, the findings
of present study are within the range of previously published studies
but more than the study done by Xu B et al. (2013). This difference
in result might be due to demographical variation. It was observed
that in normoalbuminuria group, The mean age was found 49.55
± 10.46 years in microalbuminuria group, 47.10 ± 11.24 years in
normoalbuminuria group and the difference was statistically not
significant (p>0.05) between two group. In a study done by Anesh T
et al. (2016) found that the mean age of microalbuminuria group was
57.15 ± 10.17.This difference in result might be due to demographical
variation. In present study, it was observed that almost half of the
male patients 15 (51.7%) patients were male inmicroalbuminuria
group and 20 (64.5%) in normoalbuminuria group. The difference
was not statistically significant (p>0.005) between two group. In a
study done by Anesh T et al. 2016 found that 63.8% microalbuminic
patients were male [10]. In another study, Rao PP et al. (2015) shown
that about 66% were males and 34% were females in both group. This
difference in result might be due to demographical variation and
socioeconomic status. In present study, 26(89.7%) had raised HbA1c
in microalbuminuria group and 22(71.0%) had raised HbA1c in
normoalbuminuria group. The difference was statistically significant
(p<0.05) between two groups. Gupta M et al. 2017 also found a
significant correlation between HbA1c and Microalbuminuria [11].
So, the result of present study is consistent with other studies. Based
on observations of present study, level of glycemic control seems to be
the strongest factor determining conversion from normoalbuminuria
to microalbuminuria in patients with type 2 diabetes mellitus. As
such this study will fill the gap, open new forum of discussion and will
provide knowledge and information regarding the medical workup of
patients with type-2 diabetes mellitus.
Conclusion
This necessitates that all type 2 diabetes mellitus should be
screened forHbA1c and urine microalbumin level along with blood
glucose level. Any abnormal level should be treated meticulously to
revert or prevent microalbuminuria and thus delay complications.