Advances in Diabetes & Endocrinology
Download PDF
Review Article
Reimagining Empowerment: A Critical Review of Empowerment Theory in Diabetes Research
Walker HR1* and Litchman ML2
1Medical Group Analytics, University of Utah, Salt Lake City, USA
2College of Nursing, University of Utah, Salt Lake City, USA
*Address for Correspondence:
Walker HR, Medical Group Analytics, University of Utah, Salt Lake City, UT
84102, USA; Phone: 530-755-7673; E-mail: heather.walker@hsc.utah.edu
Submission: 08 June, 2022
Accepted: 06 July, 2022
Published: 07 July, 2022
Copyright: © 2022 Walker HR, et al. This is an open access article
distributed under the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited.
Abstract
Diabetes, well documented as a complicated condition, has
been the focus of self-management studies for over three decades.
Empowerment theory has co-developed within diabetes literature
at the same time. However, this literature lacks a core and standard
definition, which has led to incongruencies in theory and relative
terminology. In this critical review, the construct of empowerment in
diabetes literature is dissected and examined. Prominent measures
and methods are problematized to highlight their overreliance on
individual behavior rather than systemic social change. Current
interventions targeting empowerment focus almost exclusively on
individual behavior-change, inadvertently suggesting that the location
of the problem of poor management lies within the abilities, attitudes,
and beliefs of individuals. This paper argues that there has to be a
socially-based power-related shift from one group to another in the
process of empowerment for its construct to be complete, and that
the ultimate agent of change must shift from the patient to systemic
barriers in their way. Examples of online patient community-generated
definitions, resources, and practices of empowerment are highlighted,
leading to an argument that researchers and healthcare providers
ought to add nuance to the construct of empowerment by weaving
in community and systems levels change goals.
Keywords
Diabetes; Empowerment; Change; Critical review;
Community-based methods, Participatory design, Systems change
Introduction
Diabetes is a condition that seeps into life physically, mentally,
emotionally, and socially. As such, there is an impact on sense of
self among people with diabetes (PWD) as one must consider their
day-to-day activities, social positioning, environment and economic
factors. There are multifarious stigmas attached to diabetes that
color the ways in which one develops and adjusts their self-concepts.
Despite the deep impact diabetes is known to have on identity, the
psychosocial impact of diabetes has only been taken up as an area
of study since the early 1990s, after a major shift in the treatment of
diabetes occurred.
In 1993, a groundbreaking study, the Diabetes Control and
Complications Trial (DCCT), was published. For the first time, there
was significant evidence linking tight diabetes self-management
to decreased incidence of diabetes-related complications [1]. For
healthcare providers, this study redefined the goals of practice and
treatment. It called for increased diabetes patient education with a
focus on self-efficacy and activation. For patients, the DCCT drastically
transformed the obligation and responsibility of risk mitigation from
being provider-based to being patient-based, increasing the psycho
social burden of diabetes on the patient [2]. For example, having a
sense that one can cause or avoid their own complications has been
linked to higher rates of stress, guilt, and distress within diabetic
populations [3]. Today, the individualized challenges of diabetes
extend far beyond the practice of doing self-management, to the art
of coping with them.
Individuals with diabetes must engage in daily self-management
practices, such as physical activity, healthy diet, taking medications,
stress reduction, and sleep. For those on insulin, it is the gold standard
to calculate insulin doses based on insulin-to-carbohydrate ratios and
insulin sensitivity ratios with every meal and snack. Diabetes calls for
advanced and thorough planning with day-to-day activities, including
travel, driving, sleeping, eating, exercising, etc. Our previous research,
further, suggests that diabetes requires individuals to shape their sense
of self around the demands of the illness – requiring they incorporate
descriptors like planner and responsible into their self-concepts [4].
Additionally, accounting for the time PWD spend thinking about
diabetes [5], it is no surprise that studies of diabetes management
have moved toward the realm of distress, depression, empowerment,
activation, and self-efficacy.
This movement in the research and treatment of diabetes toward
the psychosocial most heavily relies on nurturing patients’ selfefficacy.
Self-efficacy, a concept developed by noted Psychologist
Albert Bandura, is a person’s belief in their own ability to control their
life circumstances and effect change through behavior modification
[6]. Self-efficacy relates to a person’s ability and willingness to enact
behavior modifications toward disease management betterment.
Self-efficacy is a hyper-individualized approach to diabetes care and
treatment because it implies that control is ultimately a matter of
willingness to perform a set of behaviors that will lead to change. This
approach however, fails to capture or critically reflect on the social,
political, and economical considerations people with diabetes face.
Self-efficacy as a construct closely parallels empowerment as it is most
generally applied to diabetes in research and healthcare. This paper
critically reviews the construct of empowerment in diabetes literature
and argues for a more sociopolitical approach.
Empowerment in Diabetes Research
Empowerment blossomed in the diabetes space prior to the
DCCT, however, the DCCT amplified its construct. In 1991, diabetes
researchers introduced the need for a shift toward empowerment
within diabetes care arguing that the traditional medical model relied
too heavily on health care providers as decision-makers [7]. Originally,
the construct of empowerment was described as a form of accepting responsibility for oneself and one’s own health [7]. However, over
time, the common constructs of empowerment in the literature have
shifted and now represent several factors related to who is responsible
for empowerment, what is required for empowerment to take place
(e.g. a process, a treatment, etc.) and how empowerment might
occur. This article explores these areas and calls for a reimagining
of empowerment in the diabetes space. As an entry point into these
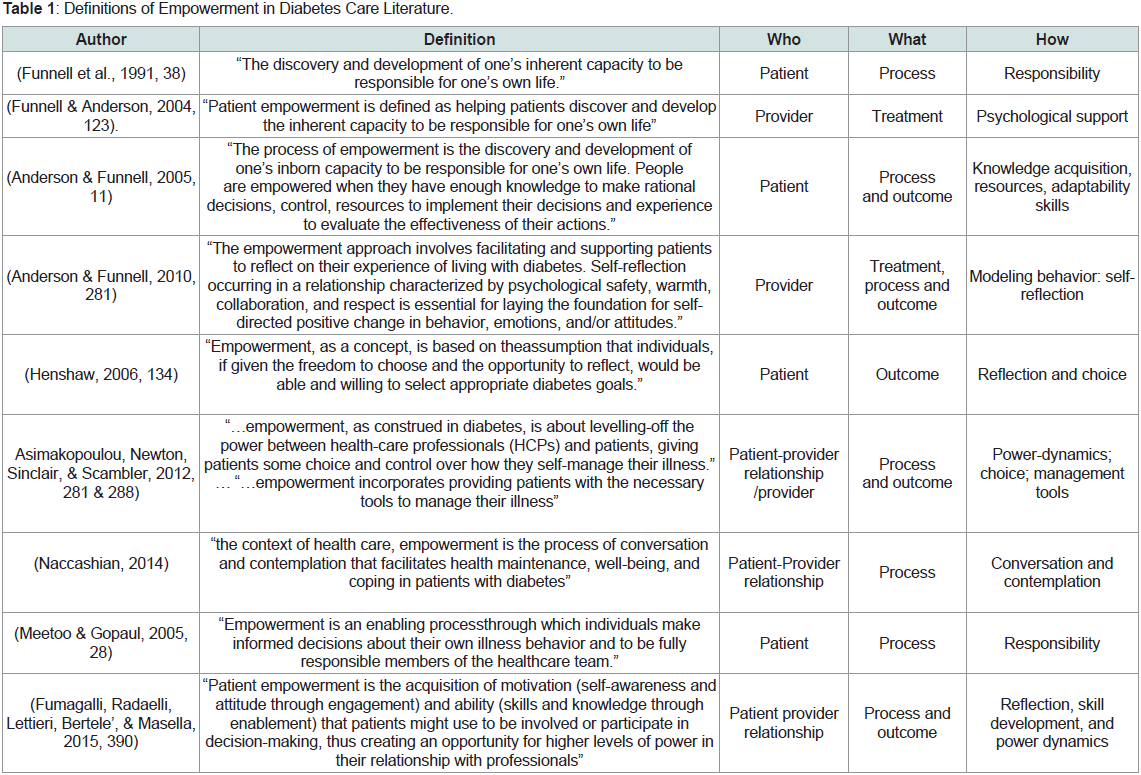
ideas, Table 1 provides definitions from leading and top cited works
on diabetes empowerment (Table 1).
The construct of “who” in empowerment:
Historically, health researchers have viewed the person
responsible for empowerment to be focused on the patient, provider,
or the patient-provider relationship (Table 1). This posits that in order
for patients to be empowered, they are to become knowledgeable
[13], reflective about their willingness to engage in diabetes selfcare
[Table 10], and choose to be responsible by engaging in diabetes self care
activities [7,11]. Providers, on the other hand, are to empower
patients by providing psychological support [8], facilitating patient
self-reflection [9], and providing diabetes self-management tools [15].
Within a patient-provider relationship, empowerment can take place
if power hierarchies are reduced [12,15], and knowledge is effectively
transferred [12].While the literature varies in stating who is responsible for
enacting empowerment, the onenessonus is always ultimately on the patient. For example, the provider can give patient tools, but the patient
has to choose to use them beyond the walls of the clinic or research
site. Providers can hand over decision-making power to the patient,
but the patient still has to use that power to weigh self-management
options and actively choose the path best suited for them. The illusory
variance in the construct of ‘who ‘in the diabetes empowerment
literature may be representative of a social phenomenon contributing
to worse health outcomes in diabetic populations.
In one community-based study, diabetes incidence was found
to be constructed as a failure of the individual. Staff persons in at
the Community Health Center of study believe that diabetes is a
signal of a defective individual who is ignorant of self-care strategies
necessary to manage diabetes effectively [16]. Perhaps more telling,
patients expressed a tendency to internalize the attributions made
by staff persons. Patients themselves believed that if they were better
educated had more education and made “better” choices, their health
would be better. This form of internalized ableism, which can be
theoretically linked to the treatment philosophies and practices used
in diabetes care today, is particular particularly insidious within
diabetes populations because of the way diabetes is associated with
poor choices [17]. When prompted during interviews with questions
related to structural inequalities, participants in the Chaufan study
reverted back to individual attributions and solutions. This implies
that both patients and community-service staff function under a
belief that the “proper locus of intervention” ought to occur at the
individual rather than the social level [16]. When only individualized approaches to diabetes empowerment are taken, social and structural
inequalities and possibilities for social change are ignored. The
problem remains then within the individual seen as responsible for
any potential change: the patient [16].
The construct of “what” in empowerment:
The mechanism through which empowerment may occur varies
throughout the literature. Some studies describe empowerment as
an outcome which can be measured and treated clinically [10,13,18].
The most common research tool used to measure empowerment as
an outcome is the Diabetes Empowerment Scale (DES). Researchers
who developed the DES describe the purpose of the empowerment
approach to treatment “as helping patients make informed choices
about their diabetes self-management” [19]. The scale is designed to
measure a patient’s behavior change and thus has been used primarily
as a pre-and post- intervention measurement. Topics covered in the
scale relate to three categories: 1) managing the psychosocial aspects
of diabetes; 2) assessing dissatisfaction and readiness to change; and 3)
setting and achieving diabetes goals [6]. The Diabetes Empowerment
Scale has been translated into several languages and into short form
as recently as 2021, suggesting it is still being used on a global scale
[19-22].Though the tool is called an empowerment scale, the journal
article introducing it describes it as a measure of self-efficacy,
indicating a conflation in terminology [6]. The questions used in the
scale focus on the patient’s belief in their ability to identify and act on
diabetes-related issues as well as their attitude toward living with the
daily requirements and demands of diabetes. Though the validity and
reliability of the scale have been confirmed, classifying the DES as a
psychometric survey, the researchers do not measure or comment on
the social validity of the scale.
Social validity can be defined as “the extent to which potential
adopters of research results and products judge them as useful and
actually use them” [22]. Though the tool is called an empowerment
scale, the journal article introducing it describes it as a measure of
self-efficacy, indicating a conflation in terminology [6,19]. The
questions used in the scale focus on the patient’s belief in their ability
to identify and act on diabetes-related issues as well as their attitude
toward living with the daily requirements and demands of diabetes.
Though the validity and reliability of the scale have been confirmed,
classifying the DES as a psychometric survey, the researchers do not
measure or comment on the social validity of the scale.
Social validity can be defined as “the extent to which potential
adopters of research results and products judge them as useful and
actually use them” [23]. In this way, potential adopters can mean
fellow researchers, members of the population of study, healthcare
providers, and so on. Though the DES has been used in many
studies since its publication in 2000, the social validity to the patient
population remains unexplored. Methodologically, this means we
have yet to develop a meaningful understanding of the relevance and
significance of the results of this scale to diabetic populations and
service organizations serving them. Furthermore, we do not know
yet of its usability by and for community members, which has been
taken into consideration by some health researchers [23,25]. It may
be the case that members of diabetes communities would want an
empowerment scale such as this one to also capture aspects of social and community empowerment. However, if they are not brought
into the research process beyond piloting the survey for validity and
reliability purposes, researchers will remain ignorant of this gap.
Empowerment has also been described in the literature as a process
of becoming empowered. Studies that take this approach either argue
that empowerment happens within the effort made to reach diabetes related
goals, but is not necessarily an end goal in itself [11,24,25],
or that empowerment is an unfolding internal process leading to a
state of being [26]. Studies that describe empowerment as a process
require healthcare provider input through education, therapy, or skill
and knowledge transference. Though the construct of empowerment
as a process revolves around individual patient growth, it suggests
that said growth cannot occur without provider involvement. This
philosophical incongruency defies the underlying aim of current
empowerment constructs arguing for self-directed patient change
studies that take this approach argue that empowerment happens
within the effort made to reach diabetes-related goals, but is not
necessarily an end goal in itself [11,24,25], or that empowerment is an
unfolding internal process leading to a state of being [28].Studies that
describe empowerment as a process require healthcare provider input
through education, therapy, or skill and knowledge transference.
Though the construct of empowerment as a process revolves around
individual patient growth, it suggests that said growth cannot occur
without provider involvement. This philosophical incongruency
defies the underlying aim of current empowerment constructs,
another problematic aspect of the way diabetes empowerment is
constructed in clinical research.
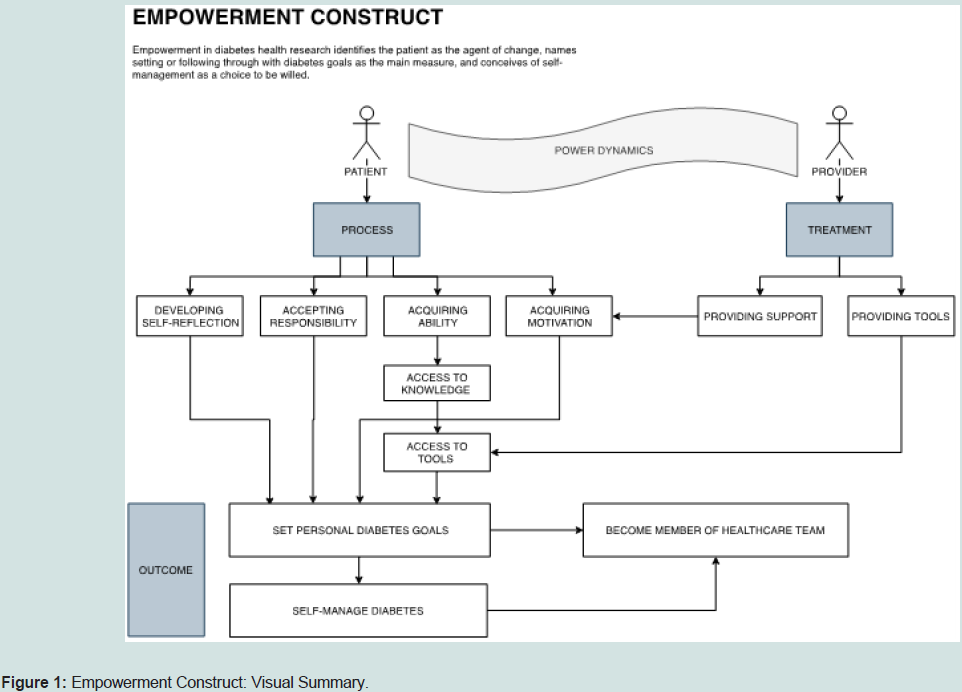
To better link the way aforementioned definitions and uses of
empowerment within diabetes literature, we developed a flowchart
of responsibility and outcome. The flowchart in Figure 1 visually
summarizes our critical review of the construct of empowerment and
its definitional components within diabetes literature.
To drive this point home, of the masse of literature covering
empowerment within the context of diabetes, few studies offer
definitions of the concept. These studies seem to take the position
that the concept of empowerment is a given, and does not need to
be thoroughly defined [27-30]. As further evidenced by our critical
review here, the construct of empowerment is not a given. There
is no universal or standard understanding or conception of what
empowerment is how to harness it, or what it looks like when it is
intervened on.
When considering what empowerment is, the literature is
evermore wrought with incongruencies and discrepancies. There
are also gaping holes which are made deeper upon reflection of the
construct of how in diabetes empowerment literature.
The construct of “how” in empowerment:
Thematically, when the definition of empowerment implicates
the patient as the agent of change, the mechanisms revolve around
individual internalization processes like self-reflection and accepting
responsibility [7,10,11,13,,24]. To drive this point home, despite
ample research articles covering empowerment within the context
of diabetes, few studies offer definitions of the concept. These studies
seem to take the position that the concept of empowerment is a given,
and does not need to be thoroughly defined [29-32]. As further evidenced by our critical review here, the construct of empowerment
is not a given. There is no universal or standard understanding or
conception of what empowerment is, how to harness it, or what it
looks like when it is intervened on.When considering what empowerment is, the literature is
evermore wrought with incongruencies and discrepancies. There
are also gaping holes which are made deeper upon reflection of the
construct of how in diabetes empowerment literature.
The construct of “how” in empowerment:
Thematically, when the definition of empowerment implicates
the patient as the agent of change, the mechanisms revolve around
individual internalization processes like self-reflection and accepting
responsibility [7,10,11,13,26]. When the definition of empowerment
implicates the provider as the agent of change, the mechanisms
revolve around modeling behaviors, psychological support, and
providing management tools [8,9]. And lastly, when the definition
of empowerment implicates the patient-provider relationship as the
agent of change, the mechanisms revolve around power dynamics,
self-reflection, and skill development [12,18,25,27]. The way in
which empowerment occurs, then, is described as dependent upon
the identified agent of change, a facet of the construct which we’ve
problematized hit her to here.Problematizing the Construct of Empowerment:
Empowerment has been problematized on the basis that use of
the term is confounded within the literature with patient activation,
patient engagement, patient participation and patient enablement [12].
Fumagalli et al. further argues that empowerment is defined across
studies as an active patient behavior, as an achievable state of being,
and as a process of transformation, much of which our critical review
discusses. This inconsistency in the literature leaves the construct
wrought with apertures, both theoretical and practical. The study
concludes with a provocative proposal: could empowerment be an
illusion of power that ultimately maintains top-down power dynamics
present within the parlance of clinical interactonsinteractions? [12].
Considering that, across definitions, empowerment is ultimately the
responsibility of the patient, this provocation merits further critical
consideration.When it comes to active participation in one’s own care, this
literature is saturated. However, there is a dearth of literature related
to social and political empowerment. What would sociocultural and
sociopolitical research on diabetes an empowerment look like? How
could methods and measures be modified to capture a more nuanced
construct of empowerment which takes into account considers
social conditions and positioning, stigma, economic, and capital
resources? Where could researchers go for guidance on incorporating
sociocultural and sociopolitical facing elements to their diabetes
empowerment research?
Empowerment as a Social Process:
As previously mentioned, community-oriented conceptualizations
of empowerment are blatantly missing from the literature on diabetes
and empowerment. Empowerment, when conceptualized as a social
process rather than an individualized one, takes on a more critical and
nuanced meaning.Disability activist and scholar, Jim Charlton’s book, Nothing About
Us Without Us: Disability Oppression and Empowerment, presents
some of the theory behind the concept of empowerment as a social
processs [31,33]. To introduce and contextualize the book, Charlton
describes a paradigm shift which occurred that critically opened
up the study of disability. He calls this shift “a historical break with
traditional perception of disability as a sick, abnormal, and pathetic
condition” [10,33]. This historical shift, in part, resulted in disabled
activists starting the Disability Rights Movement. To Charlton and the
international disability rights advocates he interviewed in the writing
of his book, “empowerment must translate into a process of creating
or acquiring power” for the collective [33]. That is, there has to be a
socially-based power-related shift from one group to another in the
process of empowerment. In this way, empowerment is not about an
individual, but about the social positioning of the group as a whole.
In diabetes, there is no shortage of stigma and prejudice creating
and maintaining the social positioning of people with diabetes as an
inferior class [17]. The attribution of both diagnosis and poor self-management
to laziness is but one example [16,32]. That is, when a
person is diagnosed with diabetes, they are categorized as one who
does not take care of themselves. In a recent study, it was found
that those who report having “poor diabetes control” experience
disproportionately more social stigma from family, friends, and the
public [33]. Similarly, in one Hong Kong-based study, participants
reported that due to perceived social stigma, they felt obligated to
only perform diabetes-related tasks in private, which then led to the
omission of blood glucose testing and insulin administration before
group meals [16,34]. That is, when a person is diagnosed with diabetes,
they are categorized as one who does not take care of themselves.
In a recent study, it was found that those who report having “poor
diabetes control” experience disproportionately more social stigma
from family, friends, and the public [35]. Similarly, in one Hong
Kong-based study, participants reported that due to perceived social
stigma, they felt obligated to only perform diabetes-related tasks
in private, which then led to the omission of blood glucose testing
and insulin administration before group meals [36]. Together, these
studies demonstrate a bi-directional relationship between perceived
social stigma and self-management.
Socially, the interventions for improving self-management
through empowerment principles, like action-planning, goals setting,
and problem solving [35,36], identifying and addressing personal
challenges [37], and integrating coping strategies [38], actually work
to authenticate the stigmatization faced by people with diabetes. That
is, it suggests that the location of the problem of poor management
lies within the abilities, attitudes, and beliefs of individuals. When our
empowerment research fails to account for the social and community
aspects of power, they also fail to challenge dominant discourses
and inequities actively reproducing power differentials. This stigmareproducing
dynamic has been shown to negatively impact research
recruitment in minority populations, as well [39].
Calling for More Participatory Methods:
In part, previous research on empowerment has failed to address
social concepts of power and positioning because the methods and
measures used to explore it have been largely top-down. To reiterate: the
dominant construct of empowerment understands self-management as a set of strategies that once adopted will move a patient to change
their health behaviors. However, as is noted in sociocultural-focused
diabetes studies, self-management does not happen in a vacuum
[16,40,41]. Socially, the interventions for improving self-management
through empowerment principles, like action-planning, goals setting,
and problem solving [37,38], identifying and addressing personal
challenges [39], and integrating coping strategies [40], actually work
to authenticate the stigmatization faced by people with diabetes. That
is, it suggests that the location of the problem of poor management
lies within the abilities, attitudes, and beliefs of individuals. When our
empowerment research fails to account for the social and community
aspects of power, they also fail to challenge dominant discourses
and inequities actively reproducing power differentials. This stigma reproducing
dynamic has been shown to negatively impact research
recruitment in minority populations, as well [41].Calling For More Participatory Methods:
In part, previous research on empowerment has failed to address
social concepts of power and positioning because the methods
and measures used to explore it have been largely top-down. To
reiterate: the dominant construct of empowerment understands
self-management as a set of strategies that once adopted will move
a patient to change their health behaviors. However, as is noted in
sociocultural-focused diabetes studies, self-management does not
happen in a vacuum [16,42,43]. As such, the dominant construct
of empowerment and the ways in which we study it must shift to
better reflect the rich lived experiences of this population. From a community perspective, being empowered is politicized when the
individual focus expands into the public/community sphere [4].
Empowerment, therefore, is an emancipatory construct when rooted
in community experience. Where we see overlap between clinical and
community-based definitions and constructs of empowerment comes
by way of the central aim: mobilization.Within diabetes online communities (DOC), a user-generated
term that encompasses people affected by diabetes who engage
in online activities to share experiences and support in siloed or
networked platforms[42], mobilization looks like social media-based
social movements through hashtags, the formation of grassroots
organizations, and public outcries in response to stigmatizing media
portrayals of diabetes.
While clinical and behavioral benefits have been identified
[43,44], the psychosocial [45,46], and community benefits are the
cornerstone of DOC participation [47-49].
Events and meet-ups within DOCs are abundant, as are calls
to influence diabetes research and outcomes by initiating and codesigning
workshops and collaborative events like those hosted by
diabetes community organizations, Diabetes Mine, The Diabetes
Empowerment Summit, Diabetes Patient Advocacy Coalition
(DPAC), Diabetes Social Media Advocacy (DSMA), We Are Diabetes,
The College Diabetes Network, Diabetes Sisters, and more.
DOC users have also actively advocated against research
methodologies that focus exclusively on summative metabolic measurements pre-and post- intervention research. The hemoglobin
A1C is a blood test that measures the concentration of glycated
hemoglobin in the blood, representative of an individual’s 3-month
average blood glucose level. A1C is the most commonly used
clinical measure of glucose and is often used in the context of how
well someone is managing their diabetes in research. In response,
members across DOCs initiated a conference called “Beyond A1C”
bringing together stakeholders, including researchers and professional
organizations, to generate research ideas for measuring change
beyond A1C [50]. Within diabetes online communities (DOCs), a
user-generated term that encompasses people affected by diabetes
who engage in online activities to share experiences and support in
siloed or networked platforms [44], mobilization looks like social
media-based social movements through hash tags, the formation of
grassroots organizations (like Insulin4All), and public outcries in
response to stigmatizing media portrayals of diabetes. While clinical
and behavioral benefits have been identified [45,46], the psychosocial
[47,48], and community benefits are the cornerstones of DOC
participation [49-51].
Events and meet ups within DOCs are abundant, as are calls
to influence diabetes research and outcomes by initiating and codesigning
workshops and collaborative events like those hosted by
diabetes community organizations, Diabetes Mine, The Diabetes
Empowerment Summit, Diabetes Patient Advocacy Coalition
(DPAC), Diabetes Social Media Advocacy (DSMA), We Are Diabetes,
The College Diabetes Network, Diabetes Sisters, and more.
DOC users have also actively advocated against research
methodologies which focus exclusively on summative metabolic
measurements pre- and post- intervention research. The hemoglobin
A1C is a blood test which measures the concentration of glycated
hemoglobin in the blood, representative of an individual’s 3-month
average blood glucose level. A1C is the most commonly used clinical
measure of glucose and is often used in the context of how well someone
is managing their diabetes in research. In response, members across
DOCs initiated a conference called “Beyond A1C” bringing together
stakeholders, including researchers and professional organizations, to
generate research ideas for measuring change beyond A1C [52]. This
example demonstrates that diabetes online communities are actively
interested and involved in ensuring research methods make sense to
their lived experience, in itself an act of social empowerment.
Patients with diabetes who post diabetes-related content online
are actively engaging in self-empowerment by inserting their
argument into the research process and agenda, making the need
for a measure of social validity paramount. When measuring social
validity, researchers ask what is the social importance and community
acceptability of this study and the resulting findings [51]?[53]?
Including a measure of social validity would add to the knowledge
produced by the field and allow findings to be translated into the realworld
more seamlessly. However, this is not enough. The historical
movement away from reliance on metabolic outcomes and toward
psychosocial ones in diabetes is an indication that making a more
drastic shift is a possibility [38,40].
Methodological Gaps:
To quell the over-reliance of individually-based measures of
empowerment predominantly used in the diabetes space, more participatory frameworks are needed. When methods incorporate
participatory elements, the scope and concepts of what empowerment
means to communities will shift. It will become more possible for
research to build capacity within communities by recognizing the
potential importance of identification with the group as a form of
stigma management. Rather than seeing diabetes empowerment as a
form of self-efficacy to be gained by individuals, it can be translated
more into a process of creating or shifting power toward the diabetes
community as a whole. Some studies have done this by inviting
influencers of varying levels in social media spaces relevant to their
study populations to engage with the research [52]. One recent study
argues that beyond increasing the social validity of a study, engaging
with influencers through participatory design facilitates the flow of
information about the study and its subsequent findings [53,54].
One recent study argues that beyond increasing the social validity
of a study, engaging with influencers through participatory design
facilitates the flow of information about the study and its subsequent
findings [55]. What’s more, participatory frameworks are also often
paired with social change.The spirit of participatory action research is based on the concept
of participation and change theorized by Paulo Freire [54,56].
According to Freire, change relies on the participation, knowledge,
and buy-in of local community members who ought to be “partners
in the processes of knowledge creation and social change” [55,57]. Not
only are community members included as partners in the research
process using this framework, they also may more directly benefit.
Participatory action research has been regaled as a framework
which “may also yield research that is more socially relevant, valid,
and accessible to people with disabilities and communities alike;
qualities which may result in more actions to improve participation
opportunities and decrease disparities” [56,58].
There are examples beyond diabetes literature which embrace the
concept of empowerment as a process of creating or shifting power in
the health fields. One Australia-based study which used a participatory
design, brought together individuals from patient, advocacy, industry,
tech, research, and academic stakeholder groups to ask “What is
currently working and not working in digital health in Australia?”
and “Where should digital health go in the future?” [57,59]. By virtue
of its design, this study actively engages patients in empowerment
principles by giving them a seat at the table - something we need to
see more of as we reimaging empowerment within diabetes research
and care [60,61].
Reimagining Empowerment in Diabetes
It is imperative we use strategies intended to mobilize the
community when selecting participatory action research methods,
rather than those which perpetuate stigmatizing representations of
a diabetic person as lazy or unwilling to self-care. We acknowledge
that diabetes advocates in online spaces are already actively calling
for a more nuanced construct of empowerment, one which implicates
social conditions and inequities they face in their daily lives. We call
researchers in the fields of health, healthcare, and health services
to move toward participatory study designs which consider and
acknowledge online diabetes advocates so that we may collectively
reimaging diabetes empowerment.