Journal of Andrology & Gynaecology
Download PDF
Research Article
Evaluating the Efficacy of Microscopic Varicocelectomy in the Treatment of Primary and Recurrent Varicocele
Erkan Erdem*
- Department of Urology, Ota Jinemed Hospital, İstanbul, Turkey
*Address for Correspondence: Erkan Erdem, Department of Urology, Ota Jinemed Hospital, İstanbul, Turkey, E-mail: erkanerdemmd@gmail.com
Citation: Erdem E. Evaluating the Efficacy of Microscopic Varicocelectomy in the Treatment of Primary and Recurrent Varicocele. J Androl Gynaecol. 2018;6(1): 2.
Copyright: © 2018 Erdem E. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Andrology & Gynaecology | ISSN: 2332-3442 | Volume: 6, Issue: 1
Submission: 23 July, 2018 | Accepted: 24 August, 2018 | Published: 31 August, 2018
Keywords
Varicocele; Microscopic subinguinal varicocelectomy; Recurrence
Abstract
Objectıve: Varicocele is the most common and correctable cause of male infertility. Microscopic subinguinal varicocelectomy is the golden standard in the treatment of this disease, and recurrence is the most common complication. The aim of this study was to investigate the outcomes of microscopic varicocelectomy in primary and recurrent varicocele.
Materıals and Method: The data of 20 patients undergoing left subinguinal microscopic varicocelectomy due to left varicocele for the first time and 20 patients undergoing the same operation for the second time due to recurrence between April 2015 and May 2017, were retrospectively evaluated. Semen analyses, testicular volumes and complication rates were compared between the groups both prior to and 12 months after the operation.
Fındıngs: The mean age was 30.2±1.4 in the primary varicocele group and 31.3±1.1 in the recurrent varicocele group (p>0.05). No significant difference was observed between the pre- and the post-operative values of testicular volume in patients undergoing primary microscopic varicocelectomy (3.2±1.4 ml and 3.1±1.7 ml, respectively; p>0.05); however, a significant improvement was observed in sperm count, motility and morphology parameters (10.3±2.9 millions/ml, 28.2±7.8%, 2.2±1.4% and 11.3±3.3 millions/ml, 30.2±6.8%, 2.5±1.8%, p<0.05).
In the recurrent varicocele group, no significant difference was observed between the pre- and post-operative semen volume (3.23±1.7 ml and 2.4±1.6 ml, p>0.05), whereas a significant improvement was observed in sperm concentration, morphology and motility parameters (9.6±3.3 millions/ml, 20.3±4.5%, 2.3±1.7% and 11.6±2.6 millions/ml, 23.2±7.5%, 2.5±1.9%, p<0.05). The testicular volume was observed to have increased in the post-operative period in both primary and recurrent varicocele groups (12.5±2.6 ml and 13.2±3.4 ml vs. (11.8±2.4 ml and 12.3±2.7 ml), which was not statistically significant (p>0.05).
Conclusion: Microscopic subinguinal varicocelectomy, which is related to the highest success rates and lowest recurrence and complication rates in the treatment of varicocele, may be safely used in the treatment of recurrent varicocele as well.
Introduction
Varcicocele is one of the most common and correctable pathologies observed in males presenting to urology clinics due to infertility [1]. The incidence in the normal population is 10-15%; however, it may be as high as 40% among patients with primary infertility and 80% among those with secondary infertility [2]. Varicocele is characterized by impairment in sperm count, motility and morphology parameters, reduced testicular volume and Leydig cell dysfunction, and leads to infertility [3]. The disease should be treated in case of diagnosed varicocele in the patient with infertility via physical examination or radiological imaging, if more than one parameter in seminal analysis is impaired and when no pathology that may lead to infertility is detected in his sexual partner [3,4]. One of the most common complications observed following varicocele surgery is recurrence. Ineffective venous ligation and anatomical variants have been shown as the common causes of the recurrence observed [5]. Some investigators have related collateral reflux to recuurence as well [6,7]. The rates of recurrence may be as high as 29% in high ligation, whereas it may be as low as 1% in the microscopic subinguinal approach [8,9].
The aim of this study was to investigate the outcomes of microscopic varicocelectomy in patients undergoing left subinguinal microscopic varicocelectomy due to left varicocele diagnosed for the first time and patients undergoing the same operation for the second time due to recurrence.
Materials and Method
The data of 20 patients undergoing left subinguinal microscopic varicocelectomy in our clinics due to left varicocele for the first time and 20 patients undertaken the same operation for the second time due to recurrence between April 2015 and May 2017, were retrospectively evaluated. Age, semen analysis parameters, testicular volumes and complication rates were compared between the groups both prior to and 12 months after the operation. Statistical analysis was performed using the SPSS for Windows, Version 22 program package (SPSS, Chicago, IL, USA). The Wilcoxon test was used to analyze the data of the NMCV group, and the Paired Sample T testi was used to evaluate the data of the PMCV group. The Independent Samples T test was used for the comparison between the groups; a p value of <0.05 was accepted as statistically significant.
Findings
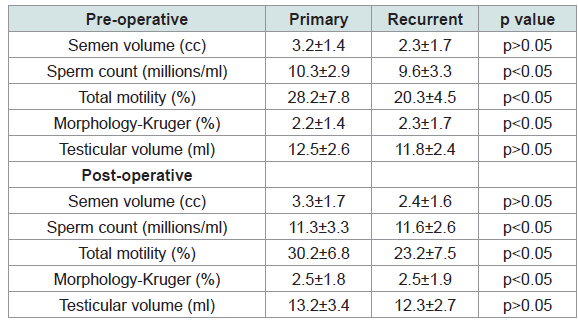
The mean age was 30.2±1.4 in the primary varicocele group and 31.3±1.1 in the recurrent varicocele group (p>0.05). Infertility was the indication for surgery in all of the patients. No complication was observed following the surgery in any of the groups (Table 1). No significant difference was observed between the pre- and post-operative values of testicular volume in patients undergoing primary microscopic varicocelectomy (3.2±1.4 ml and 3.1±1.7 ml, respectively; p>0.05); however, a significant improvement was observed in sperm count, motility and morphology parameters (10.3±2.9 millions/ml, 28.2±7.8%, 2.2±1.4% and 11.3±3.3 millions/ml, 30.2±6.8%, 2.5±1.8%, p<0.05) (Table 1).
In the recurrent varicocele group, no significant difference was observed between the pre- and post-operative semen volume (3.23±1.7 ml and 2.4±1.6 ml, p>0.05), whereas a significant improvement was observed in the sperm concentration, morphology and motility parameters (9.6±3.3 millions/ml, 20.3±4.5%, 2.3±1.7% and 11.6±2.6 millions/ml, 23.2±7.5%, 2.5±1.9%, p<0.05). Testicular volume was observed to be increased in the post-operative period, both in the primary and the recurrent varicocele groups (12.5±2.6 ml and 13.2±3.4 ml vs. 11.8±2.4 ml and 12.3±2.7 ml), which was not statistically significant (p>0.05) (Table 1).
Discussion
Varicocelectomy is the most frequently performed surgical procedure in infertile men. The target in varicocele surgery is to ligate the branches of the internal and external spermatic veins by maintaining the lymphatic vessels and artery within the spermatic cord. Since occlusion of the small collateral veins is not possible, recurrence in this method has been reported to be 4-11% [10-12]. In the inguinal and subinguinal microsurgery technique, the arteries and lymphatic vessels are mostly preserved and the other vascular structures are visualized more clearly; therefore, recurrence and complications are rather rare in these methods [13,14]. It has been reported in many studies that the recurrence rate of microscopic varicocelectomy performed within the same surgical region (inguinal or subinguinal) is significantly lower compared to the conventional methods [15].
The most important cause of recurrence in the treatment of varicocele is the failure to visualize the small internal branches of the spermatic vein and related failure of ligation. Thus, the recurrence rate is higher in conventional varicocelectomy performed without using a microscope or optic magnifiers [16,17]. Studies have demonstrated that the surgical method closest to ideal was inguinal or subinguinal varicocelectomy, which included the use of an optic magnifier [18]. However, the disadvantage of the subinguinal method has been reported as a higher risk of arterial injury due to a higher number of vein ligations and arteries, and the lower diameter of arteries observed in the more distal region, and the need for more experience in microsurgery [17]. Considering all these data, although the advantages of microscopic varicocelectomy over other methods in patients with primary varicocele have been largely accepted, studies in the literature on approach in recurrent varicocele are limited. In the light of the data obtained in this study, it may be concluded that the microsurgical method would yield better results for patients with recurrent varicocele.
Conclusion
Microscopic subinguinal varicocelectomy, which is related to the highest success rates and lowest recurrence and complication rates in the treatment of varicocele, may be safely used in the treatment of recurrent varicocele as well.
References
- Kendirci M, Miroğlu C (2004) Varicocele pathophysiology. İn: Kadıoğlu A, Çayan S, Semerci B, et al. (Eds) Male Reproductive System Diseases and Treatment. Turkish Andrology Society publication, Istanbul, Turkey, pp. 427-446.
- Gorelick JI, Goldstein M (1993) Loss of fertility in men with varicocele. Fertil Steril 59:613-616.
- (1992) The influence of varicocele on parameters of fertility in a large group of men presenting to infertility clinics. Fertil Steril 57: 1289-1293.
- Cayan S, Lee D, Black LD, Reijo Pera RA, Turek PJ (2001) Response to varicocelectomy in oligospermic men with and without defined genetic infertility. Urology 57: 530-535.
- Belli L, Arrondello C, Antronaco R, Curzio D, Morosi E, et al. (1998) Venography of postoperative recurrence of symptomatic varicocele in males. Radiol Med 95: 470-473.
- Lee JW, Paick JS, Kim SW (2008) Microsurgical subinguinal varicocelectomy: comparison of pediatric and adult patients. Korean J Urol 49: 1029-1034.
- Al-Kandari AM, Shabaan H, Ibrahim HM, Elshebiny YH, Shokeir AA (2007) Comparison of outcomes of different varicocelectomy techniques: open inguinal, laparoscopic, and subinguinal microscopic varicocelectomy: a randomized clinical trial. Urology 69: 417-420.
- Dohle GR, Colpi GM, Hargreave TB, Papp GK, Jungwirth A, et al. (2005) EAU guidelines on male infertility. Eur Urol 48: 703-711.
- Cayan S, Kadioglu TC, Tefekli A, Kadioglu A, Tellaloglu S (2000) Comparison of results and complications of high ligation surgery and microsurgical high inguinal varicocelectomy in the treatment of varicocele. Urology 55: 750-754.
- Weissbach L, Thelen M, Adolphs HD (1981) Treatment of idiopathic varicoceles by transfemoral testicular vein occlusion. J Urol 126: 354-356.
- Ferguson JM, Gillespie IN, Chalmers N, Elton RA, Hargreave TB (1995) Percutaneous varicocele embolization in the treatment of infertility. Br J Radiol 68: 700-703.
- 12.Oktar T, Ahmedov İ, Kadıoğlu A (2004) Varicocele treatment. In: Kadıoğlu A, Çayan S, Semerci B, et al. (Eds) Male Reproductive System Diseases and Treatment. Turkish Andrology Society publication, Istanbul, Turkey, pp. 463-472.
- Marmar JL, DeBenedictis TJ, Praiss D (1985) The management of varicoceles by microdissection of the spermatic cord at the external inguinal ring. Fertil Steril 43: 583-538.
- Goldstein M, Gilbert BR, Dicker AP, Dwosh J, Gnecco C (1992) Microsurgical inguinal varicocelectomy with delivery of the testis: an artery and lymphatic sparing technique. J Urol 148: 1808-1811.
- Hopps CV, Lemer ML, Schlegel PN, Goldstein M (2003) Intraoperative varicocele anatomy: a microscopic study of the inguinal versus subinguinal approach. J Urol 170: 2366-2370.
- Goldstein M (2011) Surgical management of male infertility. In: Wein AJ, Kavoussi LR, Novick AC, et al. (Eds) Campbell-Walsh urology (10thedn), Volume 1. Elsevier Saunders, Philadelphia, USA, pp. 648-687.
- Grober ED, Chan PT, Zini A, Goldstein M (2004) Microsurgical treatment of persistent or recurrent varicocele. Fertil Steril 82: 718-722.
- Cayan S, Shavakhabov S, Kadioğlu A (2009) Treatment of palpable varicocele in infertile men: a meta-analysis to define the best technique. J Androl 30: 33-40.