Journal of Andrology & Gynaecology
Download PDF
Case Report
Giant Ovarian Mass: About an Uncommon Case Report
Slaoui A1,2*, Mahtate M1, Slaoui A2, Koutani A2, Iben Atyya A2, Zeraidi N1, Lakhdar A1, Kharbach A2 and Baydada A1
1Department of Gynaecology-Obstetrics & Endoscopy, Maternity
Souissi, University Hospital Center IBN SINA, University Mohammed
V, Rabat, Morocco
2Department of Gynaecology-Obstetrics & Endocrinology, Maternity
Souissi, University Hospital Center IBN SINA, University Mohammed
V, Rabat, Morocco
3Urology Department, Avicenne Hospital, University Hospital
Center IBN SINA, University Mohammed V, Morocco
*Address for Correspondence: Slaoui A, Department of Gynaecology-Obstetrics & Endoscopy, Maternity
Souissi, University Hospital Center IBN SINA, University Mohammed V,
Rabat, Morocco; E-mail: azizslaoui27@gmail.com
Submission: 10 October, 2022
Accepted: 18 November, 2022
Published: 22 November, 2022
Copyright: © 2022 Slaoui A, et al. This is an open access article
distributed under the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited.
Abstract
Background: Ovarian giant masses remain today an uncommon
clinical presentation thanks to their early incidental radiological
discovery. Their symptomatic presentation is usually characterized
by abdominopelvic pain and a feeling of heaviness. The most
important management is the removal of the tumor in order to allow
the anatomopathological study which is the only way to confirm or
deny the malignancy. We hereby present an atypical case due to its
occurrence in a young 48-year-old female patient, the considerable
size of the tumor, its non-specific clinical and radiological presentation
making the diagnosis difficult.
Case Presentation: This was the case of a 48-year-old woman with
no particular antecedents, gravida 5 para 4 with four vaginal deliveries
resulting in the birth of four healthy children and one miscarriage. She
came to our department for management of a large abdominopelvic
mass of more than 30 cm that was bulging out all abdominal organs.
She had an MRI that strongly suspected ovarian origin and ROMA score
that came back negative for malignancy. A left oophorectomy was
followed by abdominal plasty. Anatomopathological study confirmed
a serous cystadenoma with no sign of malignancy. The patient was
discharged at D4 postoperatively. The follow-up was uneventful.
Conclusion: Giant ovarian masses, although uncommon, raise
a double difficulty for the clinician. On the one hand, the diagnosis,
although largely guided by MRI, can only be confirmed during
surgery. On the other hand, it represents a surgical challenge
whether by laparotomy or by laparoscopy. In addition, the ROMA
score based on the dosage of tumor markers CA125 and HE4 allows
malignant tumors to be screened, but confirmation is only provided by
anatomopathological study, hence the importance of not rupturing
the cyst during its extraction.
Abbreviations
BMI: Body Mass Index; MRI: Magnetic Resonance Imaging;
ROMA: Risk of Ovarian Malignancy Algorithm
Introduction
Ovarian giant masses remain today an uncommon clinical
presentation thanks to their early incidental radiological discovery.
Their management depends on the size of the tumor, the age of the
patient and the histological type [1]. Frequency of malignancy is only
37-66% in perimenopausal women and 18-86% in postmenopausal
women [2,3]. We hereby present an atypical case due to its occurrence
in a young 48-year-old female patient, the considerable size of the
tumor, its non-specific clinical and radiological presentation making
the diagnosis difficult. We then confront this case with the data of the
literature.
Case presentation
We hereby present the case of a young 48-year-oldfemale patient,
gravida 5 para 4 with four live children delivered vaginally and
one miscarriage, who came to our structure for management of an abdominal mass evolving for about 8 years. The initial erroneous
diagnosis of chronic ascites had been made and several evacuation
punctures had been performed. The patient complained of chronic
pelvic pain, complicated by digestive disorders with alternating
diarrhea, constipation and vomiting. The examination on admission
revealed an apyretic and stable hemodynamic state, a much distended
abdomen, with hyper lordosis making any movement of the patient
difficult. The patient weighed 90 kg for a height of 1.64 m with
a BMI of 33.5, the xypho-pubic distance was 60 cm, the umbilical
circumference was 100 cm. The vulva-perineal inspection was
without particularity and the speculum revealed a healthy cervix
without bleeding or leucorrhea, the vaginal examination coupled
with the abdominal palpation showed the presence of an enormous
mobile abdomino-pelvic mass which could not be separated from the
uterus. On rectal examination, a prolapsed liquid mass was perceived
in the Douglas pouch, the recto-vaginal septum and the parameters
were without particularity.
Ultrasound revealed a large abdomino-pelvic mass of difficult
exploration containing diffuse particles with localized small thickened
partitions and no visible intestinal loop. The liver, spleen and kidneys
were normal. Abdomino-pelvic MRI showed a huge cystic mass with
clear and regular contours and vegetation on the right anteroinferior
wall. It measured 35.7 x 22.4x12 cm without peritoneal effusion or
liver lesion. Biologically, the tumor markers including CA125 and
HE4 were normal. ROMA score was negative.
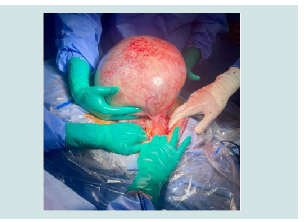
Xyphopubic median laparotomy confirmed the diagnosis of a
large cyst of the left ovary very adherent to the anterior abdominal
wall and the intestinal loops (Figure 1). The uterus and right adnexa
were of normal size and morphology. A left oophorectomy was
performed after extensive adhesiolysis. Anatomopathological study
showed macroscopically a cystic mass measuring 32x23x12 cm with a thin wall and clear liquid content and microscopically a cystic cavity
lined by a cubic epithelium with a band of fibrous connective tissue; in
some places there were pieces of normal ovarian parenchyma in favor
of a serous cystadenoma and no histological evidence of malignancy.
The epiploic and peritoneal biopsies and the peritoneal cytology were
free of any tumor infiltration.
Surgery included an abdominal plasty, preserving the umbilicus
with multiple suction drains. The patient’s weight went from 90 kg
to 76 kg, allowing her BMI to go from 33.5 to 28.3, her umbilical
perimeter from 100 cm to 68 cm and her xyphopubic distance from
60 cm to 29 cm. The postoperative course was simple with resumption
of transit on day 2 postoperatively. The patient was discharged home
at 4 days postoperatively. The follow-up was uneventful.
Discussion
Giant ovarian cysts are relatively uncommon; between 1947 and
1988, only 25 cases were described in the literature [4]. The largest
ovarian cyst described in the literature was reported in Texas in 1905
and was reported to have weighed 169 kg [5]. The diagnosis of these
giant ovarian cysts is usually easy in the presence of disproportionate
abdominal distension with depletion of the umbilicus and alteration
of the general condition. Ignorance, negligence and sometimes fear of
hospitals explain the delay in consultation in low-and middle-income
countries. A giant cyst of the ovary may simulate severe obesity or
abundant ascites [4,6].
Exploration of giant ovarian cysts relies essentially on ultrasound
and MRI. The last allows a more precise diagnosis and a better
understanding of the tumor’s relationship with other nearby organs
[4,7-10]. Surgical management of giant ovarian cysts requires perfect
collaboration between surgeons and anesthetists. The surgical
procedure can be fraught with complications such as hypovolemic
shock on removal of the tumor, intraoperative hemorrhage,
atelectasis, pulmonary edema and postoperative ileus [5,6]. All
of these conditions can be prevented by careful vascular filling,
positioning the patient in the left lateral decubitus position prior
to tumor removal, and also by proper colonic preparation of these
patients [5,6]. The wide approach by xypho-pubic incision allows a
good exposure with progressive and careful dissection of the cyst.
Given the significant stretching of the anterior abdominal wall,
abdominoplasty by longitudinal or transverse elliptical excision of the
excess skin is necessary for aesthetic reasons and above all to promote
respiratory mechanics [7,8].
Since the advent of laparoscopy and more particularly at the
beginning of the 2000s, several authors have managed giant ovarian
cysts laparoscopically, but as intra-abdominal rupture can be
dramatic for the patient especially in case of malignancy [11,12], we
have chosen classical management.
The specificity of this case is the presence of a giant mass in a
perimenopausal patient with a slow evolution of the symptomatology.
The frequency of malignancy is 37 to 66% and the size of the tumor
points to a malignant pathology [2,3]. Serous cystadenomas produce
non-specific symptoms. The most common symptoms include a
feeling of pressure in the lower abdomen and symptoms of the
gastrointestinal and urinary systems. Acute pain may also occur
with adnexal torsion or cyst rupture [13]. Serous tumors develop by
invagination of the surface epithelium of the ovary and secrete serous
fluid. Generally benign, 5-10% has borderline malignant potential
and 20-25% is malignant [14].
Measurement of the tumor marker CA125 may be helpful [15].
Many benign conditions such as fibroids, pregnancy, endometriosis,
and pelvic inflammatory disease can cause elevated CA125 levels [16].
More recently, the biomarker HE4 has been evaluated and appears
to be as sensitive as CA125 and better predictive of recurrence
than CA125 [17]. The ROMA score with both markers provides
greater sensitivity and specificity [18]. In our patient the score was
negative which is in correlation with our anatomopathological
study which did not find any sign of malignancy. Indeed, it is only
the anatomopathological examination that distinguishes between
benign, borderline and malignant serous tumors.
Conclusion
Giant ovarian masses, although uncommon, raise a double
difficulty for the clinician. On the one hand, the diagnosis, although
largely guided by MRI, can only be confirmed during surgery. On the
other hand, it represents a surgical challenge whether by laparotomy
or by laparoscopy. In addition, the ROMA score based on the dosage
of tumor markers CA125 and HE4 allows malignant tumors to be
screened, but confirmation is only provided by anatomopathological
study, hence the importance of not rupturing the cyst during its
extraction.
References
13. Muronda M, Russell P (2018) Combined ovarian serous cystadenoma and thecoma. Pathology 50: 367-369.