Journal of Addiction & Prevention
Download PDF
Research Article
Opioid Misuse Among Sexual and Gender Minorities in Texas: The Most Vulnerable Populations
Di Paola A , McCurdy SA, Schick V and Wilkerson JM*
Division of Health Promotion and Behavioral Sciences, School of Public Health, USA
*Address for Correspondence: Wilkerson JM, Center for Health Promotion and Prevention Research, Division of Health Promotion and Behavioral Sciences, School of Public Health, The University of Texas Health Science Center at Houston 7000 Fannin, Suite 2620, Houston, TX 77030, USA, Tel: 713.500.9974, Fax: 713.500.9750; E-mail: Johnny.M.Wilkerson@uth.tmc.edu
Submission: 22 December, 2020;
Accepted: 28 January, 2021;
Published: 30 January, 2021
Copyright: © 2021 Di Paola A. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background: Increasing opioid-related mortality is especially
concerning in Sexual and Gender Minority (SGM) persons who are
more likely than cis-gender heterosexual persons to have substance
use disorders. These analyses identified variables associated with
opioid (heroin and prescription pain medication) use by SGM Texans.
Method: Analyses were conducted on 1273 SGM Texans who
completed an online cross-sectional survey. Variables including
demographic characteristics, substance use, and notable life
experiences. Variables found to be significant in bivariate analyses
were entered into logistic regression models.
Results: 128 (10.0%) of participants reported opioid use within the
12 months prior. Those who reported opioid use were more likely to
use another substance or engage in hazardous drinking. Those who
reported injection drug use and having a non-monosexual private
identity were more likely to report opioid use. Although age was not
found to be a significant predictor of opioid use, those under 19 year of
age accounted for 57.0% of those who reported opioid use.
Discussion: Opioid use is a concern among SGM persons, especially
those who have a non-monosexual identity. Organizations serving
SGM persons provide services to youth should consider implementing
a screening, intervention, treatment, and harm reductionfor opioids,
alcohol, and other substances.
Introduction
An estimated 11.4 million people in the United States (U.S.) over
the age of 12 years (4.2%) have misused opioids, and 2.1 million met
criteria for an opioid use disorder [1]. In 2017, the time of the data
collection in the results presented in this article, 67.8% of all drug
overdose related deaths were due to opioid overdoses, increasing
significantly from 2016 by 12.0% [2]. National data shows a decline
in opioid related overdose deaths from 2017 to 2018 of 2% [3].
Unfortunately, this decline was short-lived. Opioid overdoses are
again increasing at alarming rates as the U.S. population deals with
stressors associated with coronavirus disease 2019 (COVID-19) [4-6].
Although opioid overdose deaths are highest in the eastern U.S.
[7], an increasing number of deaths in other densely-populated states
is cause for alarm. For example, in Texas rates of opioid overdose
deaths increased from 5.1% in 2013 to 14.9% in 2017, a 9.8% increase
[2]. While this increase is lower than the national increase, incidence
rates are still high. There is some concern that these rates could be
underestimating the true rate of opioid overdose deaths in the state.
Only 15 of 254 counties in Texas have medical examiners that can
perform autopsies and verify a death was opioid related [8]. Thus, it is plausible that the rate of opioid overdose is higher in Texas, and perhaps in similar states with limited numbers of medical examiners.
Although opioid overdoses have increased in almost all
demographic characteristics [2], persons most likely to report
misusing or meet Diagnostic and Statistical Manual of Mental
Disorders (DSM-5) criteria for an opioid use disorder include those
who are uninsured, unemployed, or have lower family income levels
[9]. Young adults between the ages of 18 and 25 are effected by the
epidemic more than older adults. It is estimated that 7.3% of young
adults misuse opioids and 1.3% meet criteria for an opioid use
disorder [1].
Although opioid overdoses have increased in almost all
demographic characteristics [2], persons most likely to report
misusing or meet Diagnostic and Statistical Manual of Mental
Disorders (DSM-5) criteria for an opioid use disorder include those
who are uninsured, unemployed, or have lower family income levels
[9]. Young adults between the ages of 18 and 25 are effected by the
epidemic more than older adults. It is estimated that 7.3% of young
adults misuse opioids and 1.3% meet criteria for an opioid use
disorder[1].
High rates of prescription opioid misuse have been linked to the
initiation of heroin use [14-16], injection drug use [17], HIV and
hepatitis C transmission [18-20], and an increased risk of opioid
overdose [18,21]. Given the already elevated rate of HIV among men who have sex with men and transgender women [22,23] it is important to identify SGM persons most at risk for experiencing
opioid-related adverse health events to introduce secondary and indicated prevention and treatment interventions.
The minority stress theory proposes that various environmental
factors which are less supportive of an individual’s identity leads to
stress producing circumstances including rejection and internalization
contribute to negative mental health and behavioral health outcomes
including substance use [24-26]. The individual identities and factors
that are included in the theory include: sexual identity, gender, and
race/ethnicity, general stressors, discrimination, and prejudice based on the individual’s identity [24-26]. Previous research has shown
that SGM persons who experience discrimination have higher rates
of problematic alcohol consumption [27,28] substance use disorders [29-31], and injection drug use [27], than those that do not experience discrimination. In comparison to cisgender heterosexual persons,
SGM persons are also more likely to report life experiences such as
homelessness and intimate partner violence [32-36]. The purpose of
this article is to explore the prevalence rate of opioid misuse, type of
opioids used, social factors, and theory-based constructs associated
with opioid misuse among SGM persons.
Methods
Study design:
Using social media banner ads, participants were recruited in
collaboration with SGM-serving community centers to complete a
statewide online cross-sectional survey, Tell Us, Texas. Social media
banner ads targeted toward persons age 13+ who indicated in their profile that they were a sexual or gender minority living in Texas or were interested in at least one SGM-related topic (e.g., Gay Pride,
LGBT bars, or LGBT community centers). SGM-serving community
centers referred persons to the survey link. Between March 2016 and
January 2017, participants completed the survey (N=1273) in English
or Spanish. To be eligible for the study, participants must have been
living in Texas, been 13 years of age or older, and identified as a
sexual or gender minority. To verify participants lived in Texas and
remove invalid entries, we adapted a previously published protocol
to include a Texas zip code [37]. Persons that did not have a Texas
zip code were excluded from the analyses. Participants completed
an online consent form prior to viewing the survey, which took
approximately 20-minutes to complete. Upon completion, the first
1,000 participants received a $5 e-gift card. All study protocols were
reviewed and approved by the researcher’s institutional review board.Measures:
Researchers at The University of Texas Health Science Center
at Houston and staff at a local SGM-serving community center
developed the survey. It included questions about demographic
characteristics, HIV sexual risk behaviors, minority stress theory based
constructs, physical and mental health diagnoses, substance
use, alcohol consumption, and various life experiences. This analysis
focused on the association between opioid misuse and individual
demographic characteristics, minority stress theory-based constructs,
notable life experiences, and co-occurring substance and alcohol use.Demographic characteristics included gender, age, race/ethnicity,
student status, insurance status, and perceived quality of life. The
majority of these variables were converted to categorical variables
for these analyses, with the exception of age. Participants were asked
to indicate their sex at birth and current gender. Using this twostep
method [38], we categorized participants as cisgender men
(assigned male at birth and identified as a men), cisgender women
(assigned female at birth and identified as awomen), or non-binary/
transgender persons (identified as a different gender than assigned at
birth). Participants’ responses” to race and ethnicity items were used
to categorize participants as Hispanic/Latinx, White non-Hispanic,
Black non-Hispanic, or other non-Hispanic. We created dichotomous
(yes/no) variables using participants’ responses” to questions about
whether or not they were a student or had health insurance. We also
created a dichotomous variable using participants’’ responses to one
item from the Center for Disease Control and Prevention Health
Days core questions (CDC HRQOL-4), which asked, “Would you say
that in general your health is” with responses of a five-point Likertscale
from “excellent” to “poor”. Those who responded being in
“good”, “very good”, or “excellent” health were categorized as being
in good general health [39]. Due to the positive skewness and kurtosis
of age, the natural logarithm was included in analyses as a continuous
variable.
Participants were asked to indicate their sexual identity. To
compare health disparities between participantsidentifying as nonmonosexual
or monosexual [40,41] we categorized participants
identifying as heterosexual or homosexual as monosexual, and
categorized participants identifying as another sexual orientation,
including bisexual, pansexual, and queer, as non-monosexual.
Participants were asked how open to others they were about their
sexual orientation. Response options were on a 5-point Likert scale
ranging from not at all out to out to most or all people [42]. A
dichotomous variables was created to compare participants who were
out to few family and friends (1 and 2) to those who were out to half
or more family and friends (3 to 5).
Minority stress theory-based constructs were also explored
in these analyses. Participants were asked if they had experienced
discrimination in the past month to completing the survey based
on their sexuality, gender, or race/ethnicity [43]. Response options
were on four-point Likert-scale ranging from “never” to “often.”
A dichotomous variable was created to compare participants
reportingany recent discrimination to those with no (“never”) recent
discrimination. A single-item social support question was used to
determine the individual’s level of social support. Those reporting
have little or no social support were compared to those who reported
higher levels of social support [44]. On a 6-point Likert scale, participants were asked about their current level of stress from “Not
at all” to “Very much” [45]. Using a cutoff value of 3, we created a
dichotomous variable to compare participants with higher or lower
levels of stress. Participants were also asked items regarding their
level of involvement in the Lesbian, Gay, Bisexual, and Transgender
(LGBT) community. We created a dichotomous variable to compare
those who were to those who were not active in the LGBT community.
In order to identify other factors associated with opioid use
participants were asked if they had experienced a verity of notable
life events. Participants were asked to indicate if and when they
experienced incarceration, homelessness, or intimate partner
violence. They were also asked to indicate if and when they had
received a diagnoses for psychological distress (depression, anxiety
or panic disorder, or Post-Traumatic Stress Disorder [PTSD]) and
if they were diagnosed with HIV. Response options for all items
included never, within the past 30 days, within thIn order to identify other factors associated with opioid use participants were asked if they had experienced a verity of notable
life events. Participants were asked to indicate if and when they
experienced incarceration, homelessness, or intimate partner
violence. They were also asked to indicate if and when they had
received a diagnoses for psychological distress (depression, anxiety
or panic disorder, or Post-Traumatic Stress Disorder [PTSD]) and
if they were diagnosed with HIV. Response options for all items
included never, within the past 30 days, within the past 12 months, or
more than a year ago. Participants’ responses were dichotomized to
compare those who did or did not report experiencing each life event
within the 12 months prior to completing the survey.e past 12 months, or
more than a year ago. Participants’ responses were dichotomized to
compare those who did or did not report experiencing each life event
within the 12 months prior to completing the survey.
Alcohol and substance use behaviors were collected for the 12 months prior to completing the survey. The three item Alcohol Use Disorder Identification Test (AUDIT-C) was used to determine if participants met criteria for hazardous drinking within the 12 months prior to completing the survey [46,47]. Those with a score of three or above for women or four or above for men where coded as being a hazardous drinker based on gender assignment at birth. Participants were also asked if they misused various substances within the 12 months prior to completing the survey. These substances were grouped by drug category: stimulants (e.g. ecstasy, ADHD medications, methamphetamine, and cocaine), benzodiazepines (e.g. Valium, and Ativan), depressants (e.g. GHB and rohypnol), and cannabis taken illicitly or not as medically prescribed. Due to the high prevalence of polysubstance use, a collective substance misuse variable was created to better understand the social determinates of opioid misuse in this population. Participants were also asked if they had injected any of the substances. A dichotomous variable was created to compare participants who reported a history of injection drug use versus those who did not.
Outcome variable:
Similar to the substance misuse categories, participants were
asked if they had used various substances illicitly or not as medically
prescribed within the 12 months prior to completing the survey.
Those who reported misuse of any of the individual opioids were
coded as having misused opioids in the 12 months prior to completing
the survey. Individual items including heroin, prescription pain
medication (e.g. Vicodin and Dilaudid), cough syrup with codeine,
buprenorphine, or methadone.Analyses
Chi-squared, Fisher’s exact, or t-tests were used to determine if
there were differences at a bivariate level for the various participant
demographic characteristics, minority stress theory-based constructs,
notable life experiences, hazardous drinking, and substance misuse
among those who did or did not report opioid misuse within the
12 months prior to completing the survey. Those found statistically significant at a p<0.10 level were entered into a logistic regression
model [48,49]. Due to the high rate of poly substance use, the
combination substance misuse variable was used in the regression
models and not the individual substances. Variables with a p<0.05
were considered to be statistically significant in the logistic regression.
All analyses were conducted in STATA version 14 [50].
Results
This was a young sample averaging 24.3 years of age (range 13
to 67 years), 51.1% of the sample was under the age of 19 years.
Among participants, 46.3% reported being a cisgender female, 38.9%
reported being a cisgender male, and 15.5% reported being a nonbinary
or transgender person. The sample was ethnically and racially
diverse; 32.2% identified as Hispanic/Latinx and 6.0% identified
as non-Hispanic Black. More than half (58.2%) reported having a
monosexual private identity, the majority of whom identified as
gay or lesbian (91.3%). Among the 41.8% reported having a nonmonosexual
private identity 63.5% identified as bisexual, 17.4%
as pansexual, and 19.0% as queer. Nearly a third of the sample
(30.2%) identified as students, and 16.6% reported not having health
insurance. A quarter (25.3%) of the participants reported having
experienced sexual, gender, or race-based discrimination, and 28.7%
reported being diagnosed with either depression, anxiety, or PTSD
within the 12 months prior to completing the survey.
Of the full sample, 10.0% (n=128) reported having misused an
opioid. The most commonly misused opioids were prescription
pain medications (79.7%, n=102), cough syrup with codeine (25.6%,
n=20), and heroin (12.3%, n=17). Those accounting for the majority
of the opioids misuse were those under the age of 19 years (57.0% of
the opioid users).
Bivariate level analysis::
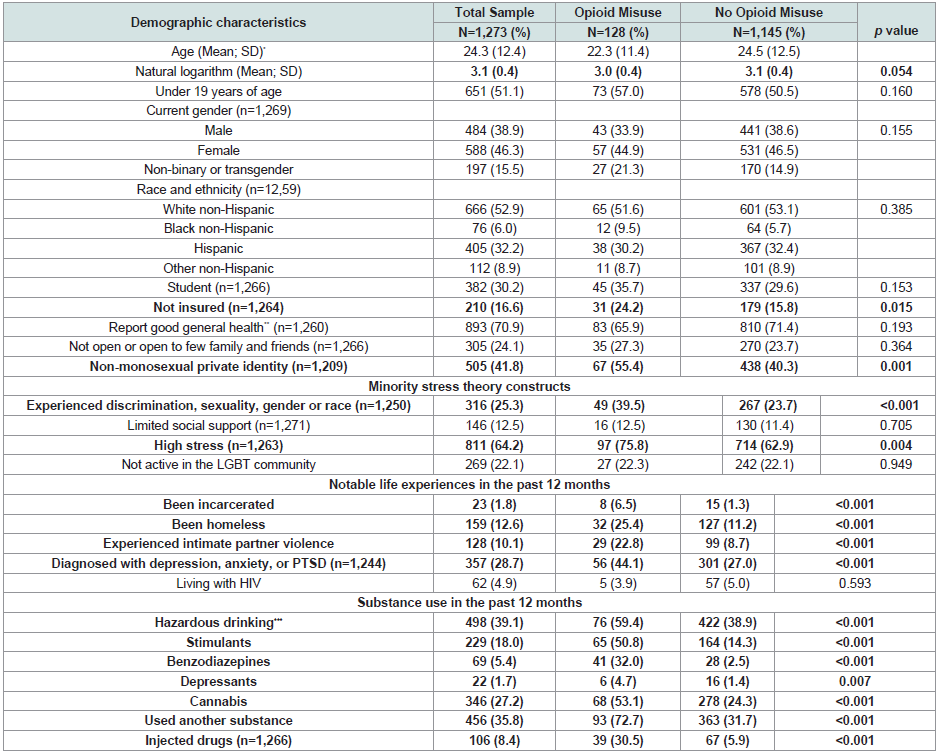
Results of bivariate analyses are summarized in (Table 1). Those who reported opioid misuse were younger than those who did not report misusing opioids in the 12 months prior to completing the survey (p=0.054) and uninsured (p=0.015). Opioid misuse was more common among participants out to most or all people they knew (p=0.048), and among those who had a non-monosexual private identity (p=0.001). Those who reported opioid misuse also reported experiencing discrimination (p<0.001) or high levels of stress (p=0.004). Participants with a history of incarceration, homelessness, intimate partner violence, or a recent mental health diagnoses (all p<0.001) were also likely to report opioid misuse. Opioid misuse was also more common among participants reporting other substance use (p<0.001 for all categories and the combined variable except depressants p=007), hazardous drinking, (p<0.001), and for those who engaged in injection drug use (p<0.001).Logistic regression:
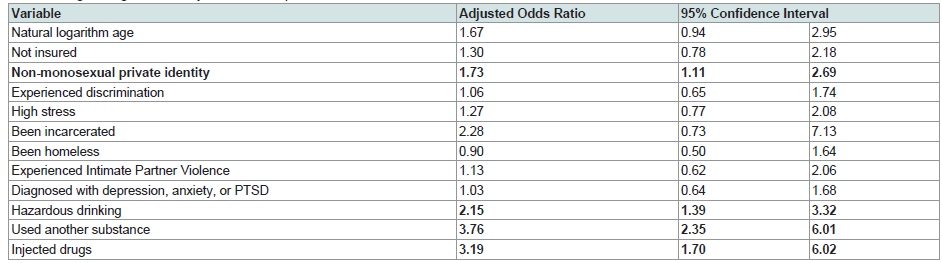
Variables found to be statistically significant (p<0.10) at the
bivariate level were entered into a logistic regression model to obtain
adjusted odds ratios for factors most strongly associated with opioid
misuse (Table 2). Participants with a non-monosexual identity
(adjusted Odds Ratio [aOR] 1.73; 95% Confidence Interval [CI]:
1.11, 2.69) were more likely misuse opioids. Participants reporting
using another substance (aOR 3.76; 95% CI: 2.35, 6.01), engaging
in hazardous drinking (aOR 2.147; 95% CI: 1.39, 3.32;), or engaging
in injection drug use (aOR 3.19; 95% CI: 1.70, 6.02) were also more
likely to misuse opioids.Discussion
SGM Texans misused opioids at rates similar to those reported
else where using data from a national sample (10.0%) [10]. What is
perhaps unique to Texas is the high off-label use of prescription pain
medication (79.7% of the opioid misused), which is associated with
the initiation of heroin use and injection drug use [4,7,15]. It is plausible that Texas will see an increasing number of SGM persons
using and injecting heroin. Surveillance efforts should include
monitoring of SGM substance use. These analyses also show that of
those who misused opioids in the 12 months prior to completing the
survey had an increased rate of hazardous drinking, other substance
misuse, and engage in injection drug use behavior. Therefore, a more
effective screening and referral to substance use treatment is needed.
SGM persons over the age of 18 have higher rates of opioid use
then their cisgender peers [10]. What is notable from our sample is
the high proportion of opioid using adolescents. Of the 128 opioid
users in our sample, 57% were under 19 years of age. Furthermore,
within our sample, 11.2% of those between 13 and 18 years old
reported opioid misuse, far exceeding the national estimate of 3.1%
for adolescents between the ages of 12 and 17 years [1]. It is imperative
that SGM-serving youth organizations, pediatricians and adolescent
physicians screen SGM patients for substance misuse.
Non-monosexual participants were more likely to report opioid
misuse than monosexual participants. There is a growing body of
literature suggesting that among SGM persons, those who express attraction to individuals of more than one gender are more likely to
experience negative health outcomes [32,35,36]. An application of
minority stress theory offers a plausible explanation for this difference
[24,25]. It is plausible that non-monosexual persons experience more discrimination due to their sexual minority status than monosexual
persons, including persons identifying as gay or lesbian. These
discriminatory experiences could result in more psychological distress
and hostility and distrust of monosexual persons outside of and within
the SGM community [51]. This psychological distress could intern
contribute to greater social isolation by non-monosexual persons,
missing potential psychological benefits of social support experienced
by persons with monosexual identities [41], an important moderator
of the relationship between minority stress and health outcomes [52].
While our findings suggest all SGM persons should be screened for
a substance use disorder and linked to culturally competent social
services, it is important to ask nuanced questions about a client’s
sexual identity and behavior so that non-monosexual individuals
can be appropriately directed to providers who are considerate of the
unique challenges that they may encounter.
Although not found to be significant in the logistic regression,
some demographic characteristics and notable life eventsfoundto be
significant at the bivariate level provide additional guidance on how
to tailor interventionsand increase access to culturally competent
healthcare for opioid-using SGM persons. Compared to participants
not using opioids, more participants reporting opioid misuse
lacked health insurance; decreasing access to routine medical care,
emergency services, and substance use detoxification, treatment,
and recovery services [53-58]. This lack of health insurance is
more concerning in a non-Medicaid expansion state, like Texas,
where uninsured persons might face additional financial barriers to
accessing healthcare. Future researchers might want to assess the
cultural competency to serve substance-using SGM persons of staff
at federally qualified health centers and other community-based
clinics to determine if additional training and support is needed to
increase the willingness of substance-using SGM persons to access
their healthcare services.
Those who reported opioid misuse were also more likely to report recent discrimination based on sexuality, gender, or race. We did not ask about discrimination based on recent substance use. However, SGM persons sometimes delay accessing healthcare to avoid potential discrimination by a healthcare provider [54,55] as do persons with a substance use disorder [59,60]. This is an important area for future research. By identifying sources of discrimination especially discrimination that might impact accessing health
services-researchers, practitioners, and policy makers might identify new collaborative efforts to develop and evaluate structural-level
interventions that reduce stigmatization based on sexuality, gender,
race/ethnicity, and substance use.
Within this sample 6.5% of persons who reported misusing
opioids were incarcerated compared to 1.3% of those who did not
use opioids. Given the small number of previously incarcerated
persons in the sample, it is likely that a larger sample would have
found a significant difference in the logistic regression. Similarly,
this regression was not powered to determine the effect of those that
have experienced homelessness, discrimination, intimate partner violence, and having been diagnosed with a mood or anxiety disorder among those who reported opioid misuse. Yet these are important
experiences that should be considered when screening for opioid and
other substance misuse, as well as when developing a treatment plan
for each individual.
Concerning are the changes in substance use related overdose
during the COVID-19 pandemic. During the early months of
COVID-19 pandemic, March to May 2020, the largest monthly
increase in substance use related deaths since 2015 was record [6].
Between June 2019 and May 2020, nationally there was a 20% increase
substance use related overdoses, primarily driven by a 38.4% increase
in synthetic opioid related overdose deaths [6]. Alarmingly the
increase in synthetic opioid related overdose deaths in Texas, as well
as 16 other states, increased over 50% in that timeframe [6]. Given
SGM persons have higher rates of opioid use than their cisgendered
peers, there is an urgent need for research, prevention, and treatment
services in this community.
Although we were able to obtain a large sample of only SGM
persons across Texas, including a subsample of persons currently
engaging in substance misuse, there are some limitations to this study.
This was a cross-sectional study, therefore changes over time and
causality cannot be determined. However, participants were recruited
using social media ads, and considering that the majority of the U.S.
population use social media these results may able to be generalizable
to many SGM Texans, and possibly nationally [61]. A second
limitation of our study was the age of the sample. While recruiting
a mostly young sample resulted in persons most likely to misuse
opioids, the lack of older participants prohibited a comparisons of
opioid use across age cohorts. This study is the use of brief self-report
measures to reduce the burden on participants completing the survey.
The use of more extensive psychosocial and cultural measures would
likely add to our understanding of the effect of discrimination and
notable life experiences on SGM persons who misuse opioids.
Conclusion
These results support the need for integrated and tailored
screening, harm reduction, and treatment interventions with
SGM culturally competent care providers or community-based
organizations, especially among adolescence. Some of the possible
interventions include harm reduction education and naloxone
distribution for those at risk for overdose. In addition, pediatricians
treating large numbers of adolescents might wish to implement
routine screening, referral, and linkage for substance use disorders.
Our findings also support the need for further integration of mental
health and trauma related services with substance use treatment
and recovery support services, and increased access to medication
assisted treatment, telehealth services, recovery coaches, recovery
residences, and peer-based support groups to provide more holistic
care solutions.