Journal of Cardiobiology
Download PDF
Case Report
*Address for Correspondence: Marion A. Hofmann Bowman, 5841 S. Maryland Avenue MC 6088 Chicago Il 60637, USA, Tel: 773 834 0807; Fax: 773 702 2681; E-mail: mhofmann@medicine.bsd.uchicago.edu
Citation: Kommineni M, Prachand V, Fedson S, Hofmann Bowman MA. New Onset of Left Ventricular Dysfunction Associated with Selenium, Zinc and Copper Deficiency Presenting Late after Gastric Bypass Surgery: Case Report and Review of the Literature. J Cardiobiol. 2013;1(2): 4.
Copyright © 2013 Kommineni M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Cardiobiology | ISSN: 2332-3671 | Volume: 1, Issue: 2
Submission: 10 October 2013 | Accepted: 03 December, 2013 | Published: 09 December, 2013
New Onset of Left Ventricular Dysfunction Associated with Selenium, Zinc and Copper Deficiency Presenting Late after Gastric Bypass Surgery: Case Report and Review of the Literature
Maya Kommineni1, Vivek Prachand2, Savitri Fedson1 and Marion A. Hofmann Bowman1*
- 1Department of Medicine, Section of Cardiology, The University of Chicago, IL 60637, USA
- 2Department of Surgery, Center for the Surgical Treatment of Obesity, The University of Chicago, IL 60637, USA
*Address for Correspondence: Marion A. Hofmann Bowman, 5841 S. Maryland Avenue MC 6088 Chicago Il 60637, USA, Tel: 773 834 0807; Fax: 773 702 2681; E-mail: mhofmann@medicine.bsd.uchicago.edu
Citation: Kommineni M, Prachand V, Fedson S, Hofmann Bowman MA. New Onset of Left Ventricular Dysfunction Associated with Selenium, Zinc and Copper Deficiency Presenting Late after Gastric Bypass Surgery: Case Report and Review of the Literature. J Cardiobiol. 2013;1(2): 4.
Copyright © 2013 Kommineni M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Cardiobiology | ISSN: 2332-3671 | Volume: 1, Issue: 2
Submission: 10 October 2013 | Accepted: 03 December, 2013 | Published: 09 December, 2013
Keywords
Thiamine; Cardiomyopathy; Bariatric surgery; MalnutritionBackground
The increasing rate of obesity and heart disease remain a global epidemic. Since 1980, the obesity rate has more than doubled to 1.4 billion adults worldwide and is related to 23% of all cases of ischemic heart disease [1]. Strategies to reduce body mass index (BMI) include diet, exercise, supplements and bariatric surgery. With proven benefit for sustained weight loss and improved cardiovascular parameters including lipids, glucose levels and blood pressure, gastric bypass surgery has increased in popularity [2-4]. The gold standard Roux-en-Y gastric bypass, indicated in patients who are morbidly obese (BMI >40 kg/m2) or in those with a BMI >35 kg/m2 with other significant comorbidities, can lead to both restrictive and malabsorptive effects. Though the effect of caloric restriction is thought to be the primary reason for weight loss, bypassing segments of bowel results in nutritional malabsorption and subsequent dyshomeostasis in minerals and micronutrients. The malabsorption following Roux-en-Y bypass is primarily due to the bypass of the duodenum, which could result in a lack of cation absorption. Of these, selenium, copper and zinc are integral for cellular function and the activity of endogenous antioxidant defenses, and reduction in their levels have been linked to dilated cardiomyopathy [5-8]. Witte et al. demonstrated a reduction in left ventricular (LV) volume and improvement in LV ejection fraction (LVEF) in heart failure patients supplemented with high dose minerals and vitamins [9]. In addition, small studies suggest a link between Vitamin B1 (thiamine) deficiency (TD), reversible heart failure, and wet Beri-beri [10-13]. Animal models demonstrated that TD leads to cardiac hypertrophy and depressed cardiac function and arrhythmias even in the absence of Beri-beri [14-16]. Thus we present a case of a young female with the acute onset of hypoglycemia ten years post gastric bypass surgery associated with severe malnutrition and significant micronutrient deficiencies in selenium, copper, zinc and B1 and subsequent development of systolic heart failure. Although other mechanisms leading to cardiomyopathy cannot be excluded, we propose that the chronic deficiency in micronutrients in conjunction with exacerbating factors associated with acute hypoglycemia/dumping syndrome may have played an important role in the development of cardiomyopathy that subsequently resolved after aggressive micronutrient supplementation.Case Report
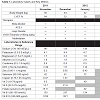
A 32-year-old female was referred to our cardiology clinic with a new diagnosis of LV dysfunction. She underwent a Roux-en-Y gastric bypass surgery at 21 years old for treatment of severe obesity with a body weight of 155 kg and body mass index of 53 kg/m2. For several years after the surgery she had a normal dietary intake including oral nutritional supplements post surgery and achieved substantial weight loss. She suffered from anxiety and depression requiring regular outpatient visits with a psychiatrist and medical therapy. Otherwise, she had no episodes of acute or chronic illness requiring hospitalization. Approximately 10 years after the Rouxen-Y gastric bypass surgery she was hospitalized for the acute onset of severe hypoglycemia and hypotension thought secondary to bacteremia and dumping syndrome. Her weight at that time was 56 kg. A transthoracic echocardiogram (TTE) at that time demonstrated a normal left ventricular function (LVEF) of 64.4% with no wall motion abnormalities. Given her new diagnosis of hypoglycemia and concern for severe malnutrition, several nutrients were measured and found to be well below the normal reference range including zinc 0.2 μg/ml, selenium 42 ng/ml, Vitamin D (9.5 pg/ml) and vitamin A 14.7 μg/ml (Table 1). She was initiated on oral supplementation of copper, selenium and zinc in addition to a multivitamin upon discharge.One month later, she presented to the emergency department with the acute onset of shortness of breath and hypoxia. Chest x-ray was consistent with pulmonary edema prompting a TTE which now showed a LVEF of 32.3% and global dysfunction (Figure 1). EKG showed regular sinus rhythm at 88 beats per minute. We were unable to make a definitive diagnosis as for the cause of her new onset cardiomyopathy. Cardiac enzymes were trended and total CK ranged from <20-32 U/L (Reference 9-185 U/L), Troponin T 0.06-0.08 ng/ml (Reference <0.10 ng/ml), and N-terminal BNP was 1502 pg/ml (Reference <125 pg/ml). Telemetry recording demonstrated sinus rhythm ranging from 72 to 135 beats per minute and few premature atrial and ventricular complexes (less than 2% of all QRS complexes). She was started on appropriate heart failure regimen including a betablocker, an angiotensin-converting enzyme inhibitor (ACE-I) and a loop diuretic. Because of her low body weight and malnutrition with persistent low serum Zinc, Selenium and Vitamin A, enteral nutrition via a gastric tube was also initiated.She was re-hospitalized again 1 month later in January 2012 for the initiation of total parental nutrition (TPN) after progressive gastrointestinal symptoms including accelerated weight loss and failure to thrive. TTE during this admission revealed an LVEF of 29.8% with severe global hypokinesis. Troponin T was borderline elevated to 0.06-0.10 (Reference <0.10 ng/ml), and total CK (22-32 U/L, Reference 9-185 U/L) and CK-MB mass concentration (1.2-1.3 ng/ml, Reference 0-9.9 ng/ml) were normal. To evaluate for myocardial injury, a cardiovascular magnetic resonance (CMR) imaging of the heart with gadolinium contrast was performed. The CMR imaging confirmed a globally dilated LV with severe global dysfunction. There was no pericardial effusion, and the tissue characterization including T2-weighted imaging and contrast enhancement were normal and not diagnostic for acute myocarditis or fibrosis. The right ventricle was normal in size and mildly reduced in function with EF 50-55%. A coronary angiogram was preformed which showed normal coronary arteries and an LV end diastolic pressure of 8 mmHg. Laboratory values indicated a normalization of blood copper levels with only minimal improvement in selenium and zinc levels. On discharge her TPN formulation was supplemented with increased levels of all three minerals. She was seen in the cardiology clinic 1 month after discharge in February 2012 and denied any clinical symptoms of heart failure. She was compliant with her heart failure regimen including a betablocker, ACE-I, and loop diuretic. Given her malabsorption and poor nutrition, we empirically recommended supplementation with 100 mg Vitamin B1 in addition to the other nutrients and minerals being provided via TPN given a low normal serum thiamine level at 124 nmol/L. At follow-up 3 months later, she remained asymptomatic from a cardiac standpoint with complete compliance of her mineral and vitamin supplements but only partial compliance with her cardiac medications, now only taking the beta-blocker. She had successfully been weaned of TPN to enteral nutritional support via her G-tube. Interestingly, her LVEF improved to 53.8% with no wall motion abnormalities despite chronically low levels of both selenium and zinc and malnutrition with abnormal low body weight of 39 kg. Over the next months the patient discontinued her beta-blocker but continued daily supplementation with thiamine 100 mg, Magnesium oxide 400 mg, and Peptamen gastrointestinal formula using 3-4 cans per day via G-tube. Repeat echocardiography 1.5 years after diagnosis of heart failure showed complete resolution in her cardiomyopathy with an LVEF of 60%. Unfortunately, her overall course has been complicated with ongoing gastrointestinal issues requiring continuation of enteral supplementation and repeat hospitalizations for complications related to malnutrition.
Discussion
The importance of cardiac function in relation to micronutrient levels has been reported in both human and animal models. Micronutrients including CoQ10, L-carnitine, thiamine, amino acids and the B vitamins are essential cofactors in energy transfer and are linked to critical myocyte pathways in the provision of ATP generation, myocardial calcium balance and balancing oxidative stress [17,18]. Less is known about the link between metallic elements and key cellular mechanisms linked to myocardial health. Selenium is a component of the antioxidant enzyme glutathione peroxidase playing a key role protecting against endothelial and myocardial dysfunction. Deficiencies in selenium and zinc have been shown to decrease myocardial and endothelial antioxidant reserve and subsequently increase oxidative damage to cell membranes thus likely causing associated cardiomyopathies. Thus, deficiencies in selenium have been linked to the development of cardiomyopathy in Chinese children, the development of heart failure post bariatric surgery, and in patients on long-term TPN [21-24]. With repletion of selenium and zinc in patients with chronic malabsorption secondary to intestinal bypass, significant improvements in both cardiac dimension and LV function were noted [24].Of the three deficient micronutrients in this patient, i.e. selenium, zinc and copper, the relationship between copper and development of human cardiomyopathy is the least understood. Copper is an essential metal co-factor in cytochrome c oxidase activity helping to regulate oxidative free radicals and is required for mitochondrial electron transport activity in cardiac and hepatic cells. In animal models, deficiencies in copper cause impairment in ADP phosphorylation and structural pathology linked to mitochondrial malfunction and subsequent cardiomyopathies [25-28]. In humans, copper supplementation has shown promise in reversing hypertrophic cardiomyopathy via induction of VEGF synthesis leading to promotion of angiogenesis in the wounded heart [29,30]. Overall, a limited number of studies and case reports have investigated micronutrient deficiencies on a small or large scale multi-nutrient spectrum that may provide insights in to the complex relationship between micronutrients and heart failure.
A key consideration in this case is the role gastric bypass plays in reducing cardiovascular risk and comorbidities in the direct relation to decreased visceral and abdominal adiposity. The Roux-en-Y gastric bypass remains the gold standard and most commonly performed of bariatric operations involving both restrictive and malabsorptive components to achieve desired weight loss via bypassing segments of bowel and decreasing the size of the stomach. Results from longitudinal studies have shown approximately 40% sustained weight loss correlating to decreases in cardiovascular risk factors including hypertension, hyperlipidemia, metabolic syndrome and diabetes [31,32]. Furthermore, several smaller nonrandomized trials suggest improved cardiovascular parameters and reversal of obesityassociated cardiomyopathy although the exact mechanism by which weight loss decreases onset of heart failure in this population has not been thoroughly studied [33]. In our patient, who maintained an approximate 95 kg weight reduction ten years post gastric bypass, her cardiovascular risk assessment post weight loss was low since she had no other cardiovascular risk factors such as diabetes or hypertension. The benefit from reduction in adiposity was likely negated by the development of severe nutritional deficiencies, which we conclude was the key determinant in the development of reversible heart failure in this patient. Although the serum values for zinc, selenium, and copper remained abnormally low after intensive supplementation, the clinical improvement of her heart failure symptoms and complete normalization of the severely reduced LVEF after initiation of TPN and intensive macro- and micronutrient supplementation led us to speculate that myocardial nutritional deficiencies may be corrected even before serum concentrations rise to normal concentrations. However, mechanisms other than nutritional deficiencies could have contributed to the reversible cardiomyopathy presented here, although our clinical, laboratory and imaging evaluation did not show evidence for tachycardia-mediated cardiomyopathy, myocarditis, coronary artery disease, or sepsis.
Of the micronutrients listed in Table 1, serum thiamine levels present an interesting avenue for further consideration. It is well documented that TD can lead to impaired cardiac function via impaired oxygen delivery through the inhibition of both the citric acid cycle and the hexose monophosphate shunt. TD can manifest in a spectrum of heart failure symptoms ultimately culminating in what is commonly known as wet Beri-beri. Furthermore, TD can be exacerbated by administration of loop diuretics, first described by Yui et al. in male Wistar rats [34]. Further studies have shown that long-term use of loop diuretics have been linked to TD via increased urinary losses thus contributing to cardiac impairment in heart failure patients [35,36].
Quantifying total body levels of thiamine has been a source of discussion. Thiamine, present in four unique compounds (unphosphorylated, thiamine monophosphate, thiamine diphosphate, and thiamine triphosphate), is typically determined via measuring thiamine pyrophosphate effect (TPPE) reflecting the activity of thiamine diphosphate on the transketolase enzyme in the pentose shunt. This commonly used assay indirectly ascertains thiamine levels measuring only the diphosphate compound without quantifying the other three sources of thiamine compounds. In cardiology clinic, she was empirically started on 100 mg of daily oral thiamine with the initiation of standard heart failure regimen. This was initiated despite a “low-normal” serum level of B1. Since more than 90% of B1 is bound to erythrocytes, the assessment of total body thiamine let alone myocardial concentrations continues to be a source of debate given a paucity of techniques to measure erythrocyte thiamine disphosphate levels, the likely key contributor to myocardial thiamine stores. Therefore, it is difficult to conclude the exact mechanism and relationship between aggressive nutritional supplementation in combination with standard heart failure regimen in the resolution of our patient’s heart failure. Future long-term studies are needed in the bariatric population to assess the relationship between nutritional macro- and micronutrient deficiencies and onset of cardiovascular disease.
Conclusion
This case demonstrates a probable relation between malnutrition as a key determinant in the development of heart failure. Following aggressive mineral and vitamin supplementation via both an oral and parenteral route, in addition to pharmacologic heart failure therapy, her LV dysfunction has since resolved. We conclude that malnutrition on a macro- and micronutrient level needs to be carefully monitored and treated in patients with signs of malnutrition. We speculate that the longstanding and chronic deficiency of micronutrients was further exacerbated by the late onset of dumping syndrome and hypoglycemia, and therefore may have unmask a cardiomyopathy resulting in reduced systolic left ventricular function and heart failure. We purpose the empiric supplementation of thiamine 100 mg daily at the diagnosis of heart failure in patients with malnutrition, in addition to other essential micronutrients, to prevent the potential development of thiamine deficiency with use of loop diuretics and potential subsequent progression of heart failure.Acknowledgements
This work was supported by funding from the Doris Duke Charitable Foundation. Dr. Hofmann Bowman is a recipient of the Doris Duke Clinical Scientist Development Award.References
- (2000) Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 894: 1-253.
- Sjostrom L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, et al. (2004) Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med 351: 2683-2693.
- Sampalis JS, Sampalis F, Christou N (2006) Impact of bariatric surgery on cardiovascular and musculoskeletal morbidity. Surg Obes Relat Dis 2: 587-591.
- McCloskey CA, Ramani GV, Mathier MA, Schauer PR, Eid GM, et al. (2007) Bariatric surgery improves cardiac function in morbidly obese patients with severe cardiomyopathy. Surg Obes Relat Dis 3: 503-507.
- Xia YM, Hill KE, Burk RF (1989) Biochemical studies of a selenium-deficient population in China: measurement of selenium, glutathione peroxidase and other oxidant defense indices in blood. J Nutr 119: 1318-1326.
- van Rij AM, Thomson CD, McKenzie JM, Robinson MF (1979) Selenium deficiency in total parenteral nutrition. Am J Clin Nutr 32: 2076-2085.
- Reeves WC, Marcuard SP, Willis SE, Movahed A (1989) Reversible cardiomyopathy due to selenium deficiency. JPEN J Parenter Enteral Nutr 13: 663-665.
- Ripa S, Ripa R, Giustiniani S (1998) Are cardiomyopathies a zinc-deficit related disease? A study on Zn and Cu in patients with chronic failure dilated and hypertrophic cardiomyopathies. Minerva Med 89: 397-403.
- Witte KK, Clark AL (2005) Chronic heart failure and multiple micronutrient supplementation: realistic hope or idealistic conjecture? Heart Fail Monit 4: 123-129.
- Mendoza CE, Rodriguez F, Rosenberg DG (2003) Reversal of refractory congestive heart failure after thiamine supplementation: report of a case and review of literature. J Cardiovasc Pharmacol Ther 8: 313-316.
- Pfitzenmeyer P, Guilland JC, d’Athis P, Petit-Marnier C, Gaudet M (1994) Thiamine status of elderly patients with cardiac failure including the effects of supplementation. Int J Vitam Nutr Res 64: 113-118.
- Shimon I, Almong S, Vered Z, Seligmann H, Shefi M, et al. (1995) Improved left ventricular function after thiamine supplementation in patients with congestive heart failure receiving long-term furosemide therapy. Am J Med 98: 485-490.
- Keith ME, Walsh NA, Darling PB, Hanninen SA, Thirugnanam S, et al. (2009) B-vitamin deficiency in hospitalized patients with heart failure. J Am Diet Assoc 109: 1406-1410.
- Yoshitoshi Y, Shibata N, Yamashita S (1961) Experimental studies on the beriberi heart. I. Cardiac lesions in thiamine deficient rats. Jpn Heart J 2: 42-64.
- Aldinger EE (1965) Effect of thiamine deficiency on potential myocardial contractility. Cir Res 16: 238-243.
- Cohen EM, Abelmann WH, Messer JV, Bing HL (1976) Mechanical properties of rat cardiac muscle during experimental thiamine deficiency. Am J Physiol 231: 1390-1394.
- Keith ME, Walsh NA, Darling PB, Hanninen SA, Thirugnanam S, et al. (2009) B-vitamin deficiency in hospitalized patients with heart failure. J Am Diet Assoc 109: 1406-1410.
- Sole MJ, Jeejeebhoy KN (2000) Conditioned nutritional requirements and the pathogenesis and treatment of myocardial failure. Curr Opin Clin Nutr Metab Care 3: 417-424.
- Boldery R, Fielding G, Rafter T, Pascoe AL, Scalia GM (2007) Nutritional deficiency of selenium secondary to weight loss (bariatric) surgery associated with life-threatening cardiomyopathy. Heart Lung Circ 16: 123-126.
- Fleming R, Lie JT, McCall JT, O’Brien JF, Baillie EE, et al. (1982) Selenium deficiency and fatal Cardiomyopathy in a patient on home parenteral nutrition. Gastroenterology 83: 689-693.
- Quercia RA, Korn S, O’Neill D, Dougherty JE, Ludwig M, et al. (1984) Selenium deficiency and fatal cardiomyopathy in a patient receiving long-term home parenteral nutrition. Clin Pharm 3: 531-535.
- de Lorgeril M, Salen P (2006) Selenium and antioxidant defenses as major mediators in the development of chronic heart failure. Heart Fail Rev 11: 13-17.
- Boldery R, Fielding G, Rafter T, Pascoe AL, Scalia GM (2007) Nutritional deficiency of selenium secondary to weight loss (bariatric) surgery associated with life-threatening cardiomyopathy. Heart Lung Circ 16: 123-126.
- Frustaci A, Sabbioni E, Fortaner S, Farina M, del Torchio R, et al. (2012) Selenium- and zinc-deficient cardiomyopathy in human intestinal malabsorption: preliminary results of selenium/zinc infusion. Eur J Heart Fail 14: 202-210.
- Weintraub ST, Wharton DC (1981) The effects of copper depletion on cytochrom c oxidate. J Biol Chem 256: 1669-1676.
- Klevay LM (1980) The influence of copper and zinc on the occurrence of ischemic heart disease. J Environ Pathol Toxicol 4: 281-287.
- Borg TK, Klevay LM (1982) Effects of dietary copper deficiency on the organization of collagen network in the cardiac skeletal muscle. Anat Rec 202: 18.
- Prohaska JR, Heller LJ (1982) Mechanical properties of the copper-deficient rate heart. J Nutr 112: 2142-2150.
- Chen Y, Saari JT, Kang YJ (1994) Weak antioxidant defenses make the heart a target for damage in copper-deficient rats. Free Radic Biol Med 17: 529-536.
- Jiang Y, Reynolds C, Xiao C, Feng W, Zhou Z, et al. (2007) Dietary copper supplementation reverses hypertrophic cardiomyopathy induced by chronic pressure overload in mice. J Exp Med 204: 657-666.
- Colquitt J, Clegg A, Loveman E, Royle P, Sidhu MK (2005) Surgery for morbid obesity. Cochrane Database Syst Rev CD003641.
- Sjostrom L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, et al. (2004) Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surery. N Engl J Med 351: 2683-2693.
- Despres JP, Lemieux I (2006) Abdominal obesity and metabolic syndrome. Nature 444: 881-887.
- Yui Y, Itokawa Y, Kawai C (1980) Furosemide-induced thiamine deficiency. Cardiovasc Res 14: 537-540.
- Freye E, Hartung E (1982) The potential use of thiamine in patients with cardiac insufficiency. Acta Vitaminol Enzymol 4: 285-290.
- Seligmann H, Halkin H, Rauchfleisch S, Kaufmann N, Motro M, et al. (1991) Thiamine deficiency in patients with congestive heart failure receiving long term furosemide therapy: a pilot study. Am J Med 91: 151-155.