Journal of Clinical and Investigative Dermatology
Download PDF
Case Report
Syphilitic Alopecia: Report of a Challenging Case and Review of the Literature
Golbert S*, Beguerie JR and Busso C
Department of dermatology, Hospital Universitario Austral, Argentina
*Address for Correspondence: Golbert S, Department of dermatology, Hospital Universitario Austral, Buenos Aires, Argentina Av. Peron 1500, Derqui (1629) Buenos Aires Province, Argentina, Email: sgolbert@cas.austral.edu.ar
Submission: 23 April 2020;
Accepted: 29 May 2020;
Published: 29 August, 2020
Copyright: © 2020 Mattos Simoes M, et al. This is an open access article
distributed under the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided the
original work is properly cited.
Abstract
Syphilitic alopecia (SA) is a rare manifestation of syphilis, which may be the
only manifestation of the disease.
Two clinical forms are described; a symptomatic alopecia and an essential
alopecia.
This last clinical form is the most frequently observed, presenting as a “motheaten”
or “patch-form” appearance, in a more diffused hair loss pattern. The term
neurosyphilis refers to the infection of the Central Nervous System (CNS) by
Treponema Pallidum (T. pallidum) and can occur at any time during the course
of the disease.
We present the case of a 61-year-old man who was diagnosed with early
neurosyphilis presenting with syphilitic alopecia, and a review of the current
literature. Although there are numerous reports of individual cases of both
syphilitic alopecia and neurosyphilis, to our knowledge there are only three reports
that describe their simultaneous presentation. We emphasize the importance of
recognizing this presentation of syphilis in clinical practice, in order to carry out a
timely treatment of the patient and their contacts.
Keywords
Secondary syphilis; Syphilitic alopecia; Neurosyphilis
Introduction
Syphilis is a sexually transmitted disease caused by Treponema
pallidum (TP), highly prevalent in Argentina. In 2018, this country
reported an increase in the incidence of this infection of 55.4% in
women and 36.4% in men, compared to the year 2017 [1]. However,
these numbers can be underestimated since syphilis is not a
mandatory reportable disease in Argentina. Syphilis presents three
stages throughout its evolution: primary, secondary and tertiary.
It may also present periods of latency between the secondary and
tertiary stages, in which it is diagnosed only by serological tests [2].
This disease has multiple cutaneous and systemic manifestations,
which depend on the stage of the disease. Syphilitic alopecia (SA)
is a rare manifestation of the secondary stage that usually occurs
in 2.9-11.2% of infected patients [3,4], as a single sign or associated
with other manifestations. Neurosyphilis (NS) is the infection of the
central nervous system (CNS) by TP and can occur at any time during
the course of the disease. Although there are numerous reports of
syphilitic alopecia and neurosyphilis, to our knowledge this would be
the fourth case with simultaneous presentation of both signs in the
same patient [5,6].
We present the case of a patient with multiple manifestations, but
undiagnosed for ten years, who after consulting about his alopecia,
was diagnosed with neurosyphilis.
Case Presentation
A 61-year-old male patient presented to the Dermatology
Department of the Hospital Universitario Austral (HUA) with a sixmonth
history of hair loss and pruritic eruption in the face. He had a history
of multiple non specific symptoms that required evaluation of various
medical specialties during the last ten years without reaching any
conclusive diagnosis. Initially, these symptoms included generalized
arthralgia of the cervical spine and shoulder girdle. Later on, the
patient presented persistent intense asthenia, myalgia, oppressive
holocranial headache, tinnitus, and decreased vision. Symptoms
increased insidiously with time.
Due to persistence and aggravation of his ocular symptoms,
a dilated fundus examination was performed in which papillae
edema was observed with small bilateral hemorrhages. A brain
magnetic resonance imaging (MRI) without gadolinium, as well as
an electroencephalogram was performed, without relevant findings.
Laboratory tests showed an increased erythrocyte sedimentation
rate (ESR) and a positive ANA 1/80. A lumbar puncture was
performed that demonstrated discrete pleocytosis (37 leukocytes /
mm3, 100% lymphocyte) and mild hyperproteinorrachia (0.55 gr /
L). Venereal Disease Research Laboratory (VDRL) test and cultures
on cerebrospinal fluid (CSF) were negative.
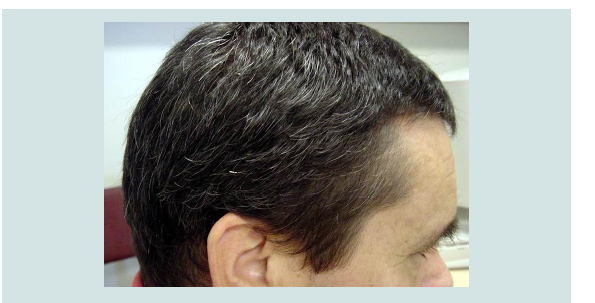
Subsequently, the patient consulted the dermatology department
for scalp alopecia with papular, erythematous and pruritic lesions on
the forehead, retro auricular region and on the scalp (Figure 1A,1B).
Alopecia was diffuse and in patches predominantly located in the
parietal region. Erythematous and asymptomatic macules were also
observed in the trunk. He had no lesions in the oral or genital mucosa,
palms or soles. Considering secondary syphilis as a differential diagnosis, a quantitative VDRL was requested. Also, a skin biopsy
of a papular lesion on the scalp was performed. The microscopic
examination showed folliculitis with acute perifolliculitis with a
neutrophilic predomination of the cells. Neutrophils compromised
the follicle wall and the peripheral area. Focal rupture of the follicular
wall was evident.
Figure 2: Three months after penicillin treatment. No alopecia is seen, nor
papules in the forehead or in the retro auricular areas.
The VDRL test was positive (512dils) which was confirmed
by fluorescent treponemal antibody absorption test (FTA abs).
Consequently, diagnosis of secondary syphilis was made. Moreover,
in this setting, the pathologic CSF analysis was interpreted as
neurosyphilis. Diagnostic tests for human immunodeficiency virus
(HIV) were non-reactive. In a new anamnesis, the patient reported a
risky sexual contact four years before the onset of systemic symptoms.
The diagnosis of syphilitic alopecia with neurosyphilis was reached.
Treatment with penicillin G sodium 24,000,000 IU / day was initiated
intravenously for 10 days.
Seven days after initiation of treatment, the patient presented
slight improvement of the ocular symptoms with decreased flashes
and improved vision and at day20 he reported improvement of the
asthenia. Over the next three months, the facial lesions disappeared
and the alopecia completely resolved (Figure 2).
Over a period of six years of follow-up, the patient remained
asymptomatic with normal fundus and serum VDRL values of 2 dils.
Discussion
Alopecia is a rare clinical manifestation of secondary syphilis and
its pathogenesis is not completely understood. One hypothesis is that
the presence of and the inflammatory response to TP, are responsible
for the loss of terminal hairs. Also, these two factors may interrupt the hair follicle cycle which results in empty follicles or broken hairs [7,8].
Another hypothesis suggests that SA is due to a telogen effluvium
secondary to the inflammatory process generated by the systemic
infection, rather than by a direct effect of the TP [8,9].
According to McCarthy’s classification (1940), SA can be symptomatic (coexisting with other clinical manifestations); or essential (when it is the only clinical manifestation) [4,9,10]. The latter is non scarring and can present in four different clinical patterns: 1)
moth-eaten, or glade like, characterized by small areas of alopecia,
mainly in the parieto-occipital region, not completely devoid of hair
and with poorly defined edges, this being the most frequent and
considered as pathognomonic [9,11]; 2) diffuse with uniform loss
and thinning of hair, similar to telogen effluvium; 3) mixed, as this
patient’s case; and 4) alopecia of the eyebrows: with thinning or
absence of hair in the distal third section of the eyebrow [11].
A diagnostic tool rarely used for the diagnosis of SA is skin
biopsy, which is usually indicated if there is a strong suspicion of
another alopecia that cannot be determined clinically [12]. The main
histological differential diagnosis of SA is alopecia areata (AA). In a
study that compared histopathological findings between these two,
the presence of peribulbar eosinophils was considered a distinctive
feature present in AA. On the contrary, the absence of eosinophils,
the presence of peribulbar plasma cells, and abundant lymphocytes
at the isthmus, suggests SA [7]. In the present case, microscopic
examination revealed a mild decreasein hair density, irregular hair
shafts, and no abnormalities in the terminal: vellus ratio. There was
no eosinophilicin filtrate. However, mild presence of periinfundibular
inflammatory lymphocytes was observed. No specific findings in the
direct immunofluorescence at the follicular basal membrane zone
were found.
To our knowledge, only three cases similar to ours have been
published in the literature. The first report was of a male patient
with alopecia of the scalp, eyebrows and eyelashes, oral ulcers,
maculopapular rash of the face and HIV infection, and rapid
progression to a left ocular panuveitis [5]. The second was a woman
with progressive headache and diffuse alopecia [6] and the last
case, a 53-year-old woman with patchy alopecia, dysphonia, genital
lesions and skin rash [13]. Although neurosyphilis can occur at any
stage of the disease, it is more frequent after 2 years of infection
(late neurosyphilis) [14]. In early stages, the spirochaete usually
affects meninges and blood vessels, manifesting as acute or chronic
meningitis and/or as auditory or ocular symptoms (iritis, retinitis or
uveitis).
In our patient, blood VDRL was positive with a titer of 512 dils,
but CSF VDRL was negative. So far, VDRL is the only validated test
for CSF evaluation. However, it can be non-reactive in up to 50% of
cases [6,15]. Consequently, this result does not exclude neurosyphilis,
in symptomatic patients. In addition, in this context, the finding of
pleocytosis and a high level of proteins in the CSF are also suggestive
of neurosyphilis [6].
Conclusions
We present the case of a patient with rheumatologic, neurologic,
ophthalmic, auditory and systemic signs and symptoms for more
than ten years, with no clear and certain diagnosis reached. This would be the fourth reported case of coexisting syphilitic alopecia
and neurosyphilis.
We highlight the importance of recognizing the cutaneous
manifestations of this polymorphic infection, given that it was
through alopecia that the final diagnosis was reached.