Journal of Clinical and Investigative Dermatology
Download PDF
Research Article
Anatomic Location is the Best Predictor of Bacterial Species in Postoperative Infections
Chow M, Miller A and Jiang SIB*
Department of Dermatology, University of California, USA
*Address for Correspondence: Jiang SIB, Department of Dermatology University of California, San Diego,Mohs and Dermatologic Surgery 8899 University Center Lane Ste 350, San
Diego CA 92122; Email: bjiang@ucsd.edu
Submission: 28 June, 2021;
Accepted: 30 July, 2021;
Published: 08 August, 2021
Copyright: © 2021 Chow M, et al. This is an open access article distributed
under the Creative Commons Attribution License, which permits unrestricted
use, distribution, and reproduction in any medium, provided the original work
is properly cited.
Abstract
Introduction: Postoperative surgical site infections are the
most common complication following dermatologic surgery. The
microbiology of these infections as it relates to patient and surgical
characteristics is not well discussed.
Methods: A retrospective chart review on all patients with
clinical evidence of wound infection and positive wound culture
between 2011-2020 was performed at our tertiary care institution. The
microbiology and resistance patterns were investigated in association
with patient and surgical characteristics.
Results: Anatomic location was most stronly associated with
the type of bacteria cultured, and contributed to the associations
between specific bacteria and type of repair (linear, flap, graft) as
well as suture material. There was no association between the bacteria
cultured and whether the patient was immunosuppressed, smoking,
anticoagulated, or diabetic. There was no association between the
bacteria cultured and suture technique or procedure type (Mohs
micrographic surgery vs excision vs biopsy vs electrodessication and
curettage).
Conclusions: Understanding the microbiology of postoperative
infections can help dermatologic surgeons in determining the best
antibiotic regimen for treatment of these infections. Our study shows
that anatomic location is the most important determinant of the
type of pathogenic bacteria that will be cultured in a postoperative
infection, and thus modifications on antibiotic based on the anatomic
location of a surgical site.
Introduction
Dermatologic surgery has historically been associated with low
rates of intraoperative and postoperative complications, though
postoperative surgical site infections (SSI) are the most commonly
reported adverse event. Prior studies have shown infection rates of
approximately 1-4.25% depending on anatomic location and type of
procedure performed [1].
SSIs are often diagnosed clinically based on signs and symptoms
of pain, warmth, edema, erythema and purulence [2,3]. Wound
cultures are helpful in identifying culprit bacteria and antibiotic
susceptibilities, though the interpretation of results is best
performed within a patient’s clinical context. In dermatologic
surgery, Staphylococcus aureus is the most commonly implicated
bacteria in wound infections, followed by Pseudomonas Aeruginosa,
Proteus Mirabilis, Enterobacter species, and Serratia Marcescens
[1-3]. Understanding of commonly implicated bacteria causing
postoperative infections can help surgeons in selecting appropriate
prophylaxis and treatment options. Because there are no standardized
guidelines, the use of antibiotics is increasing and varies widely, even
within institutions [5]. Recent reports have validated prior findings.
We previously investigated below the knee infections at our
institution [6]. We reported that patients undergoing wide local
excision were more likely to develop a lower extremity SSI than
patients undergoing MMS. Further, subcuticular sutures and vertical mattress sutures were associated with reduced infection rates than
other suture techniques. Our goal in performing the study was to
expand on this prior study, describe the SSIs that we have encountered
and treated over the previous 9 years to identify relationships between
cultured bacteria and host and clinical factors, as well as understand
the bacterial resistance patterns in our geographic location to better
help us treat SSIs going forward.
Methods
The study was approved by the Institutional Review Board of the
University of California, San Diego. Using the electronic medical
record, the authors reviewed records of all patients presenting to our
Dermatologic Surgery unit who was recorded to have developed a
postoperative infection with a positive bacterial wound culture from
2011-2020. In total, 491 patients were identified.
Patients were excluded from the study if no bacterial culture was
performed for the corresponding infection, if they had a positive
wound culture but no clinical suspicion of postoperative infection,
or if they had developed a postoperative infection from a surgery not
performed at our surgical unit. Patient demographics, comorbidities,
surgical details, antibiotic prophylaxis, culture results and resistances
were identified.
All data analysis was performed in SPSS. Chi square analysis was
applied for the analysis of categorical variables. A significance level of
p<0.05 was applied for final reporting.
Results
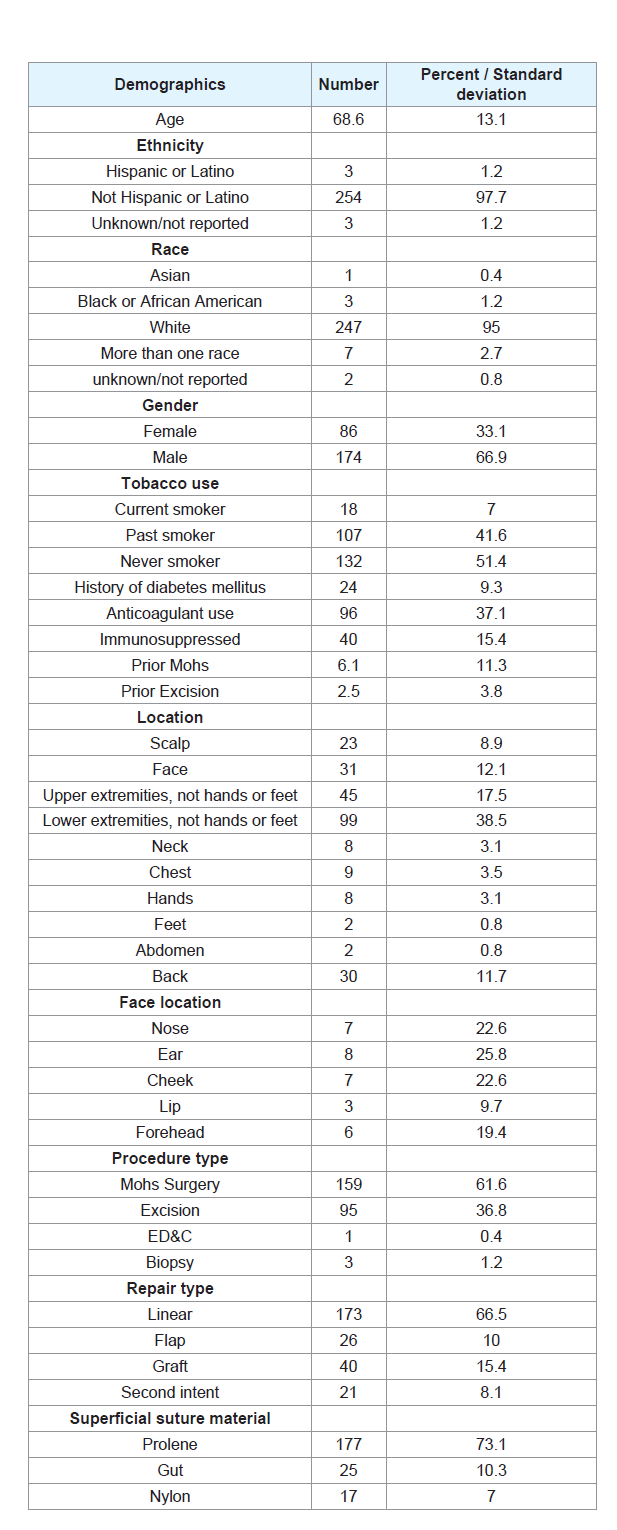
Of the 491 identified patients, 260 patients were included in the
analysis. The demographics of our samples are outlined in Table 1. The
average age of patients was 68.6 (SD 13.1) years, with a preponderance
of Caucasian (95.0%) male (66.9%) cases. The patients had an average
of 6.1 (SD 11.3) prior Mohs micrographic surgeries and 2.5 (SD 3.8)
prior cutaneous excisions. Almost 50% of patients were either current
smokers or previous smokers. In terms of medical history, 9.3% of
patients had a history of diabetes mellitus, 37.1% of patients had a
prescribed anticoagulant, and 15.4% were immunosuppressed.
Consistent with prior studies, the majority of infections were of
surgical sites on the lower extremities (38.5%), followed by the upper extremities (17.5%) and face (12.1%). The majority of the patients
had undergone Mohs surgery (61.6%), and most repairs were linear
closures (66.5%). Polypropylene was the most commonly used
superficial suture (73.1%), and simple running sutures were most
frequently used (60.0%) among these patients with SSIs. Doxycycline
(56.2%) and cephalexin (22.3%) were the most commonly prescribed
prophylactic antibiotics.
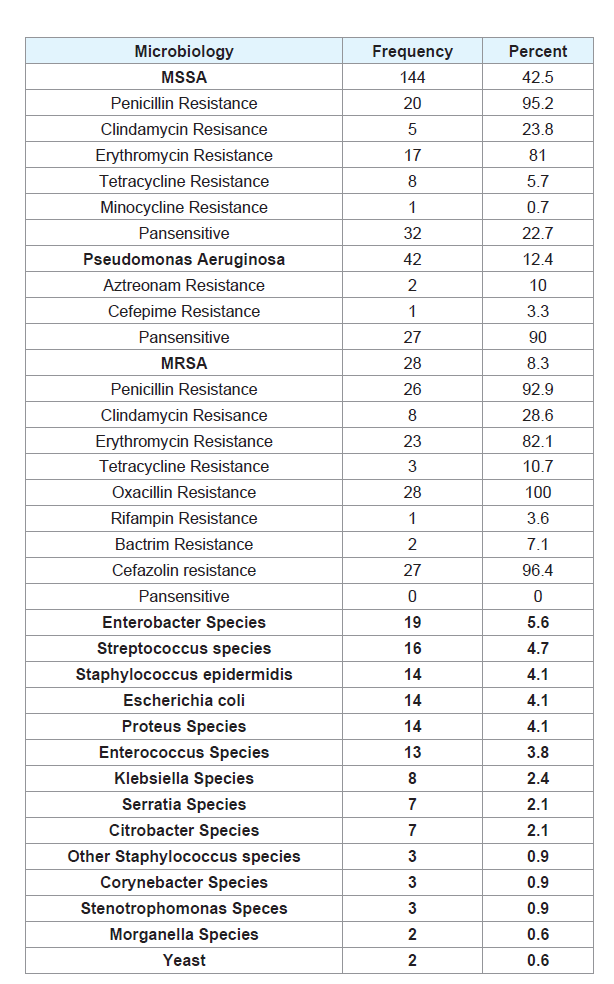
Methicillin-sensitive staphylococcus aureus (MSSA) was the
most commonly cultured bacterium at 42.5% of cultures, followed
by pseudomonas aeruginosa (12.4%) and methicillin-resistant
staphylococcus aureus 8.3%; MRSA; (Table 2). Most of the MSSA
cultures were resistant to penicillin (73.8%), and smaller percentages
were resistant to erythromycin (17.7%) and clindamycin (12.8%).
Ninety percent of the pseudomonas cultures were sensitive to all
common antibiotics tested; 2 cultures (10.0%) were resistant to
aztreonam and 1 culture (3.3%) was resistant to cefepime. For MRSA,
100% were resistant to oxacillin but only 92.9% were resistant to
penicillin. Additionally, most cultures were resistant to cefazolin
(96.4%). The culture result changed the recommended antibiotic 30%
of the time.
Next, we investigated the associations of surgical characteristics
to culture results. We would like to emphasize that this section does not discuss the rate of infections but rather the differences in the
types of bacteria cultured. Not surprisingly, anatomic location was
significantly associated with the type of bacteria cultured p<0.001. On
the lower extremities, MSSA (40.0%) was most commonly cultured,
followed by pseudomonas (20.0%) and MRSA (10.0%). Pseudomonas
was mainly cultured from the lower extremities and ears. Other
gram negative bacteria (E Coli, Enterobacter, Proteus, Klebsiella)
were similarly found almost exclusively on the lower extremities.
Though the upper and lower extremities and back were commonly
represented in our cases, there were relatively few infections on the
abdomen and chest. On the back, 28/30 (93.3%) infections were with
MSSA. Similarly, the infections on the scalp, face (excluding ears) and
extremities were most commonly with MSSA (Table 2), though the
type of bacteria cultured were not significantly associated with face
location (p=0.053).
The type of repair (linear vs flap vs graft vs healing by secondary
intention; p=0.003) and suture material (p<0.001) was significantly
associated with the type of bacteria cultured as well. As we know,
the type of repair and suture material is often dictated by the anatomic location, and posthoc analysis supported that anatomic
location confounded the bacteria results by type of repair and
suture material. Culture results were not associated with procedure
type, suture technique, smoking, diabetes, anticoagulant use or
immunosuppression status (p>0.05).
Discussion
In summary, of all cases of SSI in the last 9 years at our institution,
the majority occurred with surgical sites on the lower extremities
repaired with linear closures. There were a large number of male
patients with SSIs in our dataset. Overall, there were only a minority
of individuals who were immunosuppressed or had a history of
diabetes. Our results augment our previous study [6]: in our pool
of SSIs on all body sites in addition to the lower extremities, the
simple running suture technique was the most common. MSSA,
pseudomonas and MRSA infections were the most common bacterial
causes of infection. It is worrisome that some of our pseudomonas
cultures are resistant to aztreonam and cefepime. It is also worrisome
that MRSA is the third most common cause of SSIs in our sample,
with resistance to penicillin, cefazolin and erythromycin approaching
100% and to tetracyclines approaching 10%. Our results show that
despite the type of repair and suture material or technique used, the
surgical location is the most predictive of the type of bacteria that
will grow during a postoperative wound infection. In general, our
observations agree with those from other Centers [7]
.
We believe that some of our culture results differ from those
of prior studies due to our practice of prescribing prophylactic
antibiotics, usually doxycycline, for lower extremity surgical sites and
large flaps on the nose and ears [8]
. This may be the reason that, while
prior studies have cited MSSA, MRSA followed by pseudomonas as
their three most common causes of SSI on the lower extremities, we
report pseudomonas as being the second most common cause of SSIs
[9]. Though our study was not designed to show whether doxycycline
prophylaxis is effective at decreasing the rate of surgical infections, we
show that perhaps prophylaxis can at least change the microbiology
of infections.
In terms of sensitivities, most Staphylococcus Aureus strains
were sensitive to trimethoprim-sulfamethoxazole or doxycycline if
it was not sensitive to cephalexin. Additionally, if doxycycline is not
effective at treating a patient’s lower extremity SSI, gram-negative
coverage is most likely needed. We believe that in addition to poor
perfusion pressure in the distal limbs, higher tension and complex
closures [9], difficulty cleaning the area and washing of genital and
gastrointestinal bacteria over the area during showers could also
contribute to high infection rates.
There was a statistically significant association between surgical
location and the type of bacteria cultured [8]. The location of the
wound appears to be more important in determining the culture
results than the type of repair or suture material used. Furthermore,
suture technique, patient smoking status, immunosuppression,
diabetes, age and sex do not appear to be associated with the type
of bacteria cultured from postoperative surgical sites with suspected
infections.
As discussed in prior articles, we highlight that postoperative
wounds collect bacteria that may not be pathogenic, and culture results must be interpreted with clinical context. This is the reason
that we excluded patients with positive culture results but no clinical
signs or symptoms of infection and negative culture results despite
some clinical signs of infection.
Limitations
Our results are from a single institution and were collected
using a retrospective technique in the small number of patients
whose surgeries have been complicated by postoperative infections.
Our results are also skewed by our clinical practice of prescribing
prophylactic antibiotics in high risk surgical sites.
Conclusion
In summary, our study confirms findings from prior
investigations of postoperative wound infections and suggests that
anatomic location may be the most important determinant of the
bacteria cultured from a surgical site. In sum, the microbiology of the
cultures from SSIs can help clinicians decide which prophylactic and
treatment antibiotics are most appropriate for our surgical patients.