Journal of Clinical and Investigative Dermatology
Download PDF
Review Article
Moisturizers Free of Paraben, Mineral Oil, Alcohol and Ingredients from Animal Origin (Pama) - A New Way Forward
Satish DA1, De A2, Gala MYN3*, Muchchala SS3 and Rathod R3
1Sagar Hospitals & at Skin Cosmetic & ENT Care Center, Bangalore, India
2Calcutta
National Medical College, Kolkata, India
3Dr. Reddy’s Laboratories, Hyderabad, India
*Address for Correspondence
Gala MYN, Dr. Reddy’s Laboratories, Hyderabad, India; Phone: +91
9004117134; E-mail: monil.yogesh@drreddys.com
Submission: 12 November, 2021
Accepted: 19 April, 2022
Published: 22 April, 2022
Copyright: © 2022 Satish DA, et al. This is an open access article
distributed under the Creative Commons Attri-bution License,
which permits unrestricted use, distribution, and reproduction in
any medium, provided the original work is properly cited.
Abstract
Effective management of dry skin conditions involves the treatment
of a defective skin barrier. Moisturizers enhance and preserve the
smoothness of the skin in patients with dry skin conditions as well as
those with healthy skin. Many ingredients of moisturizers have the
potential to cause irritant and allergic contact dermatitis; therefore,
it is necessary for clinicians to be aware of such potential allergens
to manage and advise their patients’ accordingly. Moisturizers free
of paraben, mineral oil, alcohol and ingredients from animal origin
(PAMA) have an advantage since they don’t cause sensitivity, allergy
or dermatitis. This review will help dermatologists understand the need
and benefits of low allergen containing moisturizers.
Keywords
Atopic dermatitis; Moisturizer; Psoriasis
Introduction
Inadequacy in barrier function is a prime factor in development
of dry skin conditions [1]. According to a questionnaire based survey,
32.3% of Indians had sensitive skin that made them more likely to
suffer from dry skin conditions [2]. Therefore, optimum water content
in stratum corneum (SC) is of utmost importance in preserving
skin’s appearance and texture. In the acute phase of atopic dermatitis
(AD), topical corticosteroids are frequently an important part of
the therapy procedure. Systemic adverse effects, such as inhibition
of the hypothalamus-pituitary-adrenal axis, are a serious issue with
topical corticosteroids [3]. Moisturizers are common personal care
products and widely prescribed by dermatologists for managing dry
skin conditions. Cosmetics/skin care products consisting of paraben,
mineral oil alcohol and ingredients from animal origin (PAMA) are
few of the main culprits of causing irritant and allergic reactions.
Limitations of PAMA containing moisturizers
Parabens:
Since parabens are rapidly absorbed and can build in the body,
they are one of the most used preservatives. The most prevalent
allergens are butyl paraben, methyl paraben, propyl paraben, and
ethyl paraben, which were discovered in 61.6% of the moisturizers
tested [4]. Contact dermatitis caused by parabens results in rash,
pimples, dry, and scaly skin. Furthermore, parabens have been
linked to the development of persistent dermatitis, which raises
the likelihood of sensitivity to topical therapeutic drugs. Literature
suggests that parabens are endocrine disrupting chemicals (EDCs)
that might cause fitness and functional problems. The presence of
unmetabolized form of parabens in human breast cancer tissue has
sparked controversy concerning its hazardous potential [5].Alcohol:
A study observed that 23.6% of moisturizers included benzyl alcohol, a common contact allergen [4]. Repetitive topical application
and use of moisturizer has been documented to produce reactions
[6]. Toxicological reactions observed are subjective irritation, contact
urticarial, non-immunologic type, immunologic type, allergic contact
dermatitis, and immediate-type reactions.Mineral Oil:
There has always been a controversy regarding mineral oil and
its benefits. Petrolatum, and paraffin oil are the most commonly used
mineral oil in topical cosmetic products. They have been a concern
in regulatory areas of consumer products such as cosmetics and food
[7]. Long-term use of mineral oil causes occupational folliculitis [8].
Medicinal white oils or waxes cause mild erythema on damaged skin.
Moisturizers containing 10% mineral oil make the skin slightly more
sensitive to UV [7]. As a result, the mainstay of prevention is avoiding
contact with such chemicals.Ingredients from animal origin:
Contact allergies to animal-derived compounds such as lanolin
and wool alcohols are becoming more common. Lanolin made from
sheep`s wool was found in 9.8% of moisturizers, making it the ninth
most common allergen, and reactions to lanolin more frequently
occur on compromised skin, similar to paraben sensitivity [4].The above data suggests that PAMA ingredients can potentially
cause sensitivity, allergy and delayed hypersensitivity reaction.
Contact dermatitis and chronic irritant dermatitis resulting in rash,
pimples, and dry and scaly skin may develop. Patients with AD are
at risk of flare-ups resulting in worsening of their clinical condition.
PAMA ingredients are known to cause persistent dermatitis,
increasing the risk of allergy and sensitivity to topical therapeutic
drug ultimately leading to delayed clinical benefit. Thus moisturizers
without PAMA ingredients maybe a more suitable option for patients
with dry skin conditions including AD and psoriasis.
Need of Natural Moisturizing Agents:
Moisturizers are common personal care products and widely
prescribed by dermatologists for managing AD. Many of the ingredients mentioned above have the potential to cause irritant and
allergic contact dermatitis (ICD and ACD). Hence, dermatologists
must be aware of such allergens to avoid ACD and ICD and improve
clinical outcome. Patients must be advised according to their skin
sensitivity and history of known allergens. Moisturizers containing
natural effective ingredients may be more suitable for improving
skin hydration. Consequently, natural moisturizers may be used in
moisturizing cosmetic formulations and also as a complement in the
treatment of dry skin. Explained below are few natural PAMA free
moisturizing ingredients.Mango butter:
Mango butter, also known as mango oil, is made from the seeds
of mango trees. The oil content of dry seeds varies between 4 and
13% [9,10]. Mango butter is highly recognized for its bacteriostatic
and anti-inflammatory properties, indicating that it could be used as
a cosmetic ingredient for healing and protection [11]. Its saturated
fatty acid profile is dominated by oleic (42%) stearic (40%) and
palmitic (8%) acids, which account for up to 50% of the saturated
fatty acid profile [12]. The unsaponifiable matter in mango butter,
which is made up of tocopherols, phytosterols, and triterpenes, helps
to minimize wrinkles and skin roughness, as well as its capacity to
heal, protect, and rebuild the skin’s lipid barrier. Mango butter is an
effective formulation for sensitive skincare products because of all of
these qualities. It is thought to be a viable alternative to cocoa butter
and mineral-based emollients.Aloe vera:
Aloe vera is beneficial in variety of skin diseases like seborrheic
dermatitis, psoriasis vulgaris, wound healing, and it has healing
effect, anti-inflammatory action, moisturizing and anti-aging effect,
anti-septic effect, anti-acne effect, laxative effect, antiviral action,
anti tumor activity and effect on immune system [13]. Moisturizing
effect is by increased production of collagen and elastin fibres making
skin more elastic, soft, and less wrinkled. Moisturization in dry skin
provides improved skin integrity, reduced fine lines and wrinkles
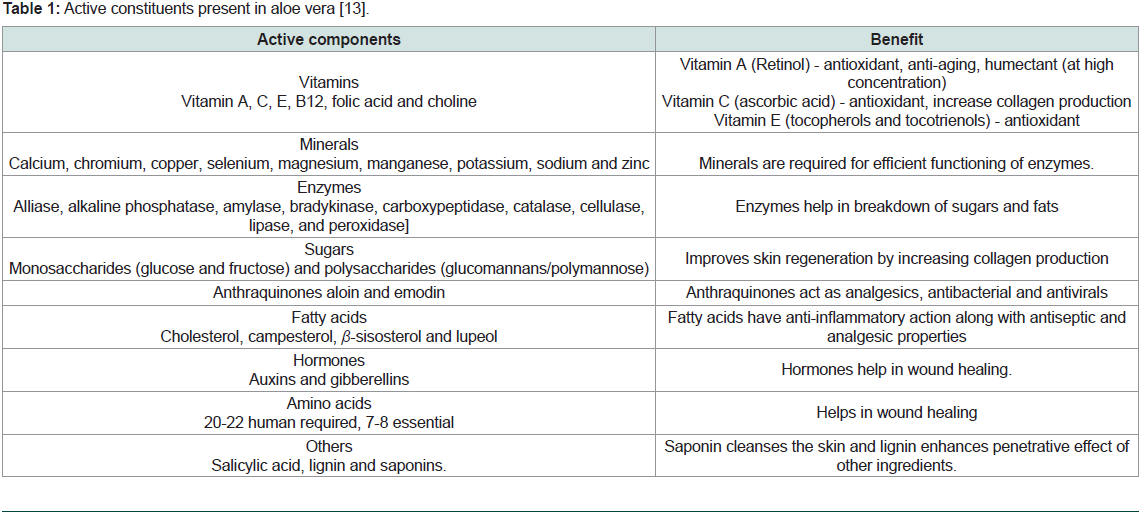
and decreases erythema [13]. Aloe vera contains 75 potentially active
constituents (Table 1).
Table 1: Active constituents present in aloe vera [13].
Aloe vera freeze dried extract is an effective ingredient for
improving skin hydration through humectant mechanism. It is used
to retain skin moisture and integrity of skin which makes it a potent
cosmetic formulation. As a complementary treatment aloe vera can
improve wound healing, treat dry skin and improve health of society
[14,15]. Aloe vera formulations with only 0.25% and 0.50% (w/w)
extract is known to increase the water content of stratum corneum.
Other formulation with (0.10%, 0.25% and 0.50%) extract is known
to have same impact after 2 weeks of application [14]. In one study,
participants were asked to discontinue all oral medications and replace
topical applications with botanical anti-inflammatory moisturizer
for a period of 2 weeks. The results showed significant improvement
in irritation, erythema, desquamation, roughness, dryness, itching,
and overall skin appearance [16]. Butters are intensive moisturizing
cream that maintains hydration and overall integrity of the skin by
improving skin barrier function, making it more resistant to external
irritants. Aloe vera butter is a plant based butter that it provides
hydration, softens and heals dry skin and has a good safety profile
[17]. Evidence suggests thatafter two weeks application of 0.1, 0.25
and 0.5% of aloe vera extract, skin hydration is increased [18]. Most
commonly used formulation for psoriasis is aloe vera extract (0.5%)
in a hydrophilic cream [17,19].
Shea butter:
Shea butter processed from the nut of vitellaria paradoxa
(shea tree) contains antioxidants such as stearic acid, linoleic acid,
catechins, and is used for inflammatory dermatoses such as psoriasis
and atopic dermatitis [20]. Shea butter is composed of five major fatty
acids, including palmitic, stearic, oleic, linoleic, and arachidic acids. It
also contains triterpene acetate and cinnamate esters, demonstrating
anti-inflammatory and anti-tumor promoting effects [21]. Clinical
studies have demonstrated shea butter as skin aging treatment, which
regenerates skin and gives smoother, clearer skin. Shea butter had
cicatrizing action in 70% of cases of hand dermatitis, sun burn and
scars. A cream with shea butter was also demonstrated to promote
good moisturization of the skin compared to placebo [22]. in a
pediatric study, the cream containing shea butter extract did not
differ in acceptability or efficacy from a ceramide-precursor product
for eczema [20].Glycerin:
Glycerin has been hypothesised to incorporate ceramides, which
play an important role in improving the barrier function of dry
flaky skin by easing digestion. The proportion of lipids in the solid
form, such as eicosapentaenoic (EPA), docosahexaenoic (DHA), and
stearidonic acid, may rise in dry skin, and glycerine may assist keep
the lipids in a liquid crystalline state at low relative humidity [23]. In
a randomized study, moisturizer with 20% glycerine appeared to be a
suitable alternative to urea/sodium chloride in the treatment of atopic
dry skin. Furthermore, adverse skin reactions such as smarting were
felt significantly less among patients using the glycerine moisturizer
compared with the urea/saline cream [24].Vitamin E:
After attempting numerous medications, such as antihistamines,
steroids, and cyclosporine A, the majority of patients get discouraged.
Vitamin E lowers the level of immunoglobulin E (IgE) antibodies in
AD patients in recent research [3]. Tocopherols and tocotrienols
are both types of vitamin E, however only alpha and gamma
tocopherols are biologically active [25]. The most important lipid
soluble antioxidant found in cell membranes is vitamin E. In the
stable form of tocopheryl acetate, vitamin E prevents oxidation of
chemical components found within the bottle of the moisturizer. This
preservative function coupled with excellent skin conditioning effects
is the main reason that vitamin E is frequently added to moisturizers
[26].A randomized, double-blind, placebo-controlled trial in patients
with mild-to-moderate AD concluded that vitamin E 400 IU/
day significantly improved itching, extent of lesion and severity
scoring of atopic dermatitis (SCORAD) index (p<0.05) compared
to control after four months of treatment. As vitamin E has no
side effects with a dosage of 400 IU/day, it can be recommended
for the treatment of AD [3]. A single-blind clinical study reported
remarkable improvements in facial erythema, lichenification, and
the appearance of normal skin in subjects with eczematous lesions
who were given 268 mg of vitamin E and these effects were mostly
due to the decrease in pruritus. In another randomized, doubleblinded,
placebo-controlled trial with 45 eczema patients, SCORAD
assessment showed improvement in the patients who ingested
vitamin E supplements [22]. In a recent Italian study, 46% of patients
in the vitamin E group showed improvement compared to only 2%
of patients in the placebo group [27]. A meta-analysis concluded that
vitamin E improved the SCORAD Indexin eczema patients [28].
Human body cannot produce this vitamin and the skin levels
of vitamin E depend on its oral or topical use. Alpha-tocopherol
prevents oxidative stress of free radicals on cell membrane. Vitamin
E protects the macrophage membrane against oxidative damage and
reduces production of prostaglandins through affecting the immune
system. Although contact dermatitis, burning, and itching have
been reported on topical use of vitamin E, none of them occurred in
patients receiving vitamin D (400 IU/day) [3].
Squalene:
Squalene is an isoprenoid molecule, a component of human
sebum that is one of the most prevalent lipids produced by human
skin cells. It is a single oxygen quencher, protecting skin from lipid peroxidation due to ultraviolet and other ionizing radiation exposure.
About 60% of dietary squalene is absorbed in humans. It is carried
in serum in conjunction with very low-density lipoproteins and is
found throughout the human body, with the highest concentration
in the skin [29]. Squalane, a saturated form of squalene is less
susceptible to oxidation. Thus, squalane is thus more commonly used
as a moisturizer. Although the body produces squalane naturally, its
synthesis drops dramatically around the age of thirty, contributing
to dry skin. Squalane has the added benefit of not having an oily
feel, being odourless, non-comedonal, antibacterial, and suitable for
sensitive skin, despite the fact that it is technically oil [21].Cocoa butter:
Pertaining to skin health, cocoa components have been utilized
in diseases, such as skin cancer, psoriasis, acne, and wound healing.
Cocoa has great potential not only for the treatments of skin diseases,
but also for their prevention [30].The overall mechanisms and advantages of PAMA free
moisturizing ingredients is depicted in Figure 1 and 2.
Burden of different dry skin conditions in India
Atopic dermatitis, contact dermatitis, dyshidrotic eczema, hand
eczema, neurodermatitis, nummular eczema, and stasis dermatitis
are the different types of eczema [31]. Dermatitis has a variable
incidence in India, ranging from 0.24-0.42 % in children aged 0-14
years, according to an out-patient department (OPD) study [32].
Dermatitis affects 0.9% of children aged 6-7 years in India, according
to a survey for adolescents and parents conducted by the International
Study of Asthma and Allergies in Childhood (ISAAC) [33]. The
reported prevalence of hand eczema in the general population is
around 10% [34]. It is difficult to report the exact prevalence of hand
eczema since it is underreported and very few seek medical attention
[35]. Depending on age and geography, the prevalence of AD ranges
from 11 to 21%. Furthermore, about 15-20% of children and 1-3% of
adults have steroid sensitive dermatoses [36].
Role of moisturizers in the management of atopic dermatitis
Moisturizers considerably reduce the severity of AD and
symptoms of inflammation, such as pruritus, erythema, fissuring,
and lichenification. Moisturizers also help to prevent flare-ups of
AD. They also aid in the reduction of prescription medicine usage
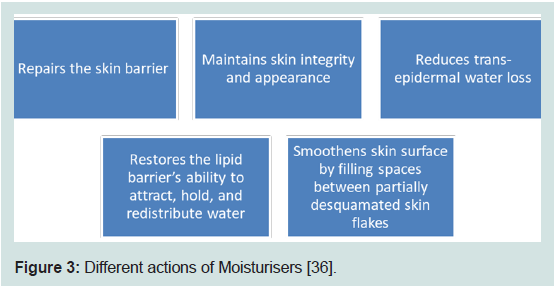
[37,38]. The different actions of moisturizers are mentioned in
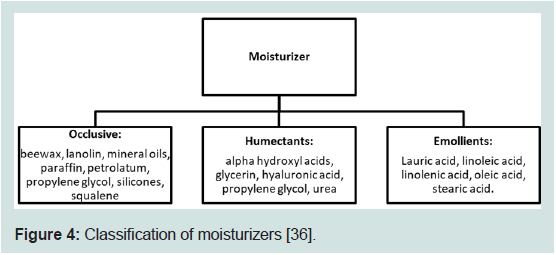
Figure 3. Moisturizers can be classified as occlusive, humectants and
emollients (Figure 4).
Figure 3: Different actions of Moisturisers [36].
Figure 4: Classification of moisturizers [36].
Place of Moisturizers in the management of atopic dermatitis and psoriasis
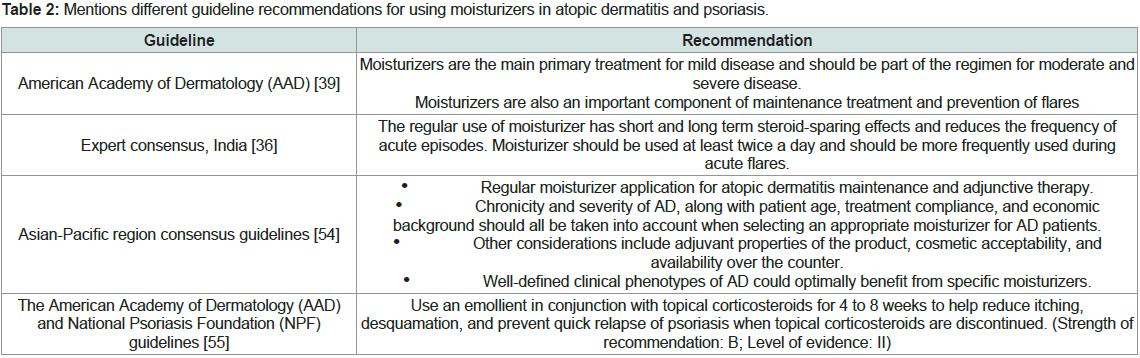
Different guideline recommendations for using moisturizers in
atopic dermatitis and psoriasis are mentioned in Table 2.
Table 2: Mentions different guideline recommendations for using moisturizers in atopic dermatitis and psoriasis.
Moisturizers are the core of the management of AD. Evidence
suggests that the use of moisturizers reduces and AD severity, along
with decreasing the amount of prescription anti-inflammatory
treatments required for disease control. Moisturizers are therefore a cornerstone of AD therapy and should be included in management
plans [39]. For all patients, daily showers or baths followed application
of emollients and moisturizers, with avoidance of trigger is the basic
management and flare prevention [40]. Moisturizers and emollients
should be used in the following cases: minimal psoriasis, napkin
psoriasis, psoriasis of the folds, psoriatic skin damaged by previous
local treatments, and in pregnancy or women of childbearing age
[41]. According to the Indian consensus, varying skin types (oily, dry,
combination, normal) guide the selection of amount, frequency and
type of moisturizer. Therefore, an ideal moisturizer must be tailored
with attributes adaptive to most circumstances and applicants [29].
Moisturizers for Covid-19:
According to the data, 4.5% of Covid-19 patients presented with
cutaneous manifestation such as itching, urticarial, vesiculopapular
rash, acral erythema, maculopapular rash, irritant contact dermatitis,
and others [42]. In India, an upsurge of hand dermatitis cases without
any previous history has been observed amidst the pandemic [43].
Few cases of new onset ACD/ICD have been observed. Among all
conditions, dryness due to hand hygiene tops the list followed by
ACD & ICD (6.2% and 1.4%, respectively). Lipid barrier of skin
is depleted due to the regular use of lipid dissolving alcohols and
detergents, leading to xerosis and thereby ICD or ACD. Lower
concentration of lipid dissolving alcohol and alkaline pH of causes
the dehydrative effect [35]. Another reported problem was ‘Acne
and Skin breakdown’, after 2-3 hours of wearing mask. Commonly
affected areas included bridge of the nose and cheek bones, attributed
to frequent changes and tight fitting masks and goggles.Moisturizers, emollients, barrier creams and low potency topical
steroids are recommended as symptomatic treatment, for reported
conditions and to prevent skin breakdown [44,45]. Moisturization
can be the sixth step in hand hygiene protocol. Regular applications of
moisturizing hand creams can reverse glove induced maceration and
minor erosions [34]. (Jindal R) Instructions of applying moisturizer
each time immediately after hand wash, before glove occlusion and a
thick layer every night has been provided by the American Academy
of Dermatologists (AAD) [46]. American Contact Dermatitis Society
recommends moisturizers for both prevention and treatment of
xerosis and dermatitis due to hand hygiene [47]. Furthermore, the
application of moisturizers seems to prolong the disease-free interval
in patients with controlled hand eczema [24].
Clinical Evidence of moisturizers for the treatment of dry skin disorders:
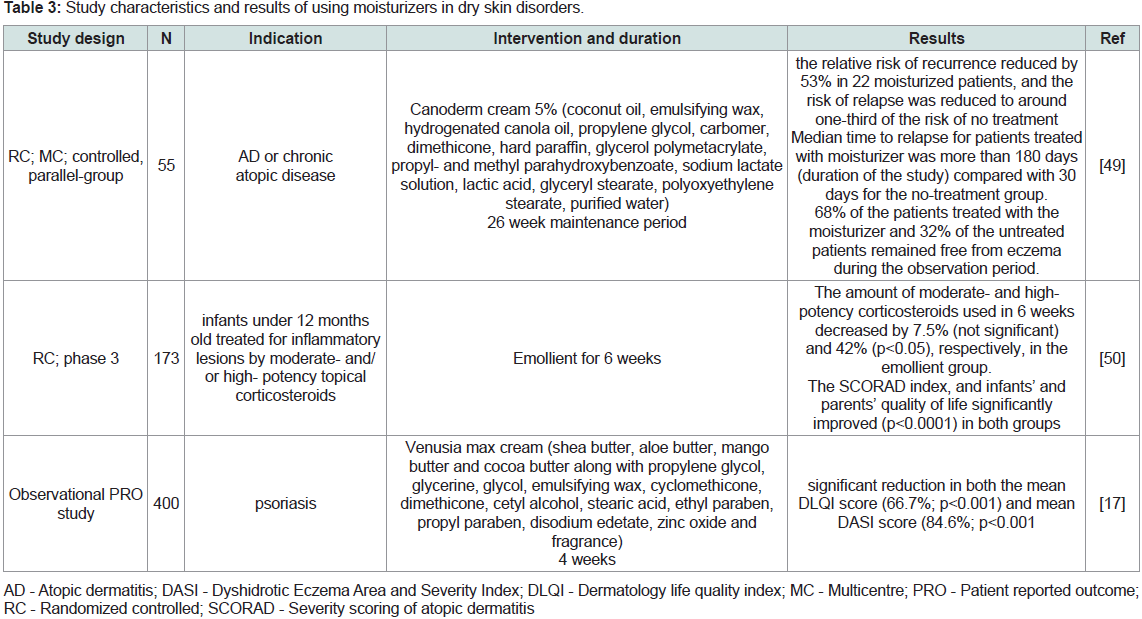
A Cochrane review (2016) concluded that most moisturisers
showed some beneficial effects; prolonging time to flare, reducing the
number of flares and the amount of topical corticosteroids needed
to achieve similar reductions in eczema severity [48]. Maintenance
therapy with a barrier-improving moisturiser on corticosteroidhealed
(betamethasone valerate) sites lowered the incidence of atopic
dermatitis return in AD patients [49]. Emollient treatment for six
weeks significantly reduced the high-potency topical corticosteroid
consumption and improved quality of life in infants with AD [50].
Clinical efficacy of moisturizers is depicted in Table 3.Lipid-rich moisturisers can successfully treat ICD based on
clinical evidence [51]. Most moisturisers have positive effects, such
as extending the time between flares, reducing the number of flares,
and lowering the dose of topical corticosteroids required to achieve
equivalent eczema severity decreases [52]. Literature suggests that
moisturisers improve clinical symptoms,transepidermal water loss
(TEWL) and stratum corneum hydration [53]. An intensive plantbased
butter moisturizing cream (Venusia Max) significant improved
quality of life by 67% and reduced eczema severity by 84.6% when
used as an adjuvant treatment option for the management of psoriasis
[17].
Conclusion
Moisturizers are common personal care products and widely
prescribed by dermatologists for managing dry skin conditions.
Skin care products consisting of allergens like paraben, mineral oil
alcohol and ingredients from animal origin (PAMA) cause irritant
and allergic reactions. Patients must be advised according to their
skin sensitivity and history of known allergens. Natural moisturizers
containing PAMA free ingredients may be more suitable for improving skin hydration. Consequently, natural moisturizers may
be used in moisturizing cosmetic formulations and also as adjuvant
therapy for the treatment of atopic dermatitis and other dry skin
conditions.