Journal of Clinical & Medical Case Reports
Download PDF
Case Report
Postoperative Scalp Angiosarcoma was Accompanied by Ipsilateral Cephalic and Facial Herpes Zoster Appearance
Chao Ye1, WeiHong Cao1*, QianWen Zhang2 and YiJian Yu3
1Department of Plastic Surgery, Taizhou Hospital of Zhejiang Province
Affiliated to Wenzhou Medical University, Taizhou, China
2Dermatology Department, Taizhou Hospital of Zhejiang Province affiliated to Wenzhou Medical University, Taizhou, China
3Department of Pathology, Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical University, Taizhou, China
2Dermatology Department, Taizhou Hospital of Zhejiang Province affiliated to Wenzhou Medical University, Taizhou, China
3Department of Pathology, Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical University, Taizhou, China
Address for Correspondence: WeiHong Cao, Department of Plastic Surgery, Taizhou Hospital
of Zhejiang Province Affiliated to Wenzhou Medical University, No. 150 XiMen Road, Taizhou, Zhejiang 317000, China, E-mail Id: caoweihong@hotmail.com
Submission: 01 November, 2023
Accepted: 05 December, 2023
Published: 08 December, 2023
Copyright: © 2023 Ye C, et al. This is an open-access article
distributed under the Creative Commons Attribution License,
which permits unrestricted use, distribution, and reproduction
in any medium, provided the original work is properly cited.
Keywords: Cutaneous angiosarcoma; Scalp; Herpes zoster Appearance;
Perineural invasion metastasis
Abstract
Background: Cutaneous angiosarcoma is a rare cutaneous
malignancy with poor prognosis. Because of its diverse clinical
manifestations lack of specificity, clinical treatment is difficult.Here we
present a case of postoperative scalp angiosarcoma with ipsilateral
cephalic and facial herpes zoster appearance.
Case Report: An 88-year-old man was diagnosed with scalp angiosarcoma and underwent extensive excision and skin graft. Red induration occurred around the skin graft area of the scalp 1 month after surgery, along with ipilateral head and face blister-like changes and intermittent aggravated neuralgia. Finally, he died 3 months later due to refusal of further treatment. Immunohistochemistry was performed on sarcoma tissue and paracancer tissue obtained by pathological examination. The results indicated that the expression of NGF and TrkA were positive in sarcoma tissue and negative in paracancer tissue.It is speculated that there may be perineural invasion metastasis in angiosarcoma of scalp which is associated with sarcoma progression, increased local recurrence, intense pain, and poor prognosis.
Conclusion: Once cutaneous angiosarcoma patients indicate nerve invasion, immunohistochemical staining of pathological section NGF and TrkA should be performed when necessary to determine whether there is positive expression, so as to determine the possibility of perineural invasion metastasis. When such patients present with vesicular manifestations accompanied by progressive aggravated neuralgia, they should be highly vigilant about the possibility of sarcoma recurrence and perineural invasion metastasis, so as to actively take further treatment measures early to prolong the life of patients as much as possible.
Case Report: An 88-year-old man was diagnosed with scalp angiosarcoma and underwent extensive excision and skin graft. Red induration occurred around the skin graft area of the scalp 1 month after surgery, along with ipilateral head and face blister-like changes and intermittent aggravated neuralgia. Finally, he died 3 months later due to refusal of further treatment. Immunohistochemistry was performed on sarcoma tissue and paracancer tissue obtained by pathological examination. The results indicated that the expression of NGF and TrkA were positive in sarcoma tissue and negative in paracancer tissue.It is speculated that there may be perineural invasion metastasis in angiosarcoma of scalp which is associated with sarcoma progression, increased local recurrence, intense pain, and poor prognosis.
Conclusion: Once cutaneous angiosarcoma patients indicate nerve invasion, immunohistochemical staining of pathological section NGF and TrkA should be performed when necessary to determine whether there is positive expression, so as to determine the possibility of perineural invasion metastasis. When such patients present with vesicular manifestations accompanied by progressive aggravated neuralgia, they should be highly vigilant about the possibility of sarcoma recurrence and perineural invasion metastasis, so as to actively take further treatment measures early to prolong the life of patients as much as possible.
Abbreviations
cAS: cutaneous angiosarcoma; PNI: perineural invasion;
NGF:nerve growth factor; TrkA: tropomyosin receptor kinase A; CT:
computed tomography; PET: positron emission tomography
Introduction
Cutaneous angiosarcoma((cAS)) is a rare cutaneous malignancy
with poor prognosis. It is characterized by multifocal, diffuse, invasive,
and high recurrence rate, and has the worst prognosis among all soft
tissue sarcomas [1]. Various clinical manifestations of cAS have been
reported in the literature, while herpes zoster appearance had rarely
been mentioned, and they were all treated as herpes zoster in the
early stage [2]. Based on this case, we speculated that angiosarcoma
of scalp may have a metastatic mode of perineural invasion, which
is associated with sarcoma progression, increased local recurrence,
intense pain, and poor prognosis.
Case Report
An 88-year-old male with left top mass for 2 months and ulcerative
bleeding for 1 week presented to our Plastic and aesthetic department
on September 17, 2021.On physical examination, the mass on the top
of the head was about 3*3.5cm, purple in color, medium in quality,
unclear in boundary, poor in motion, red, swollen and ulcerated on
the surface, a small amount of fluid seepage, and no obvious swelling
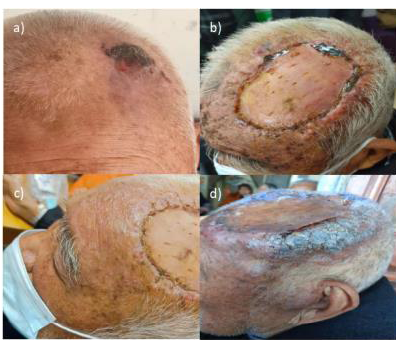
of superficial lymph nodes in the neck [Figure 1a].
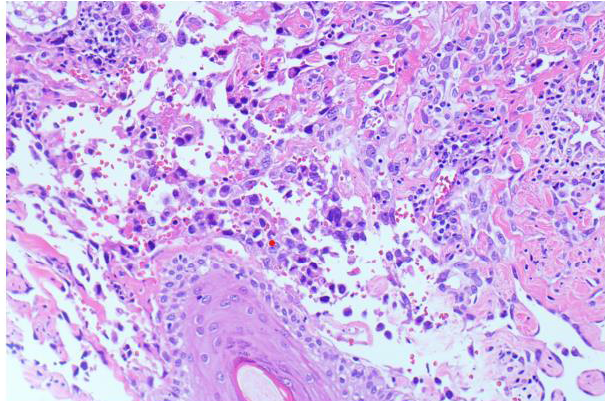
We suspected it was a skin malignancy. A biopsy was completed;
pathology revealed vascular-derived tumors with heterotypic
cells (considered angiosarcoma), immunohistochemistry was
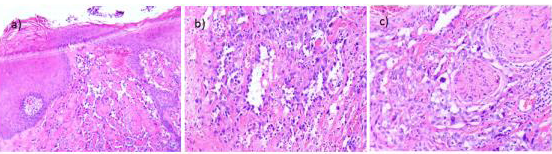
recommended [Figure 2].
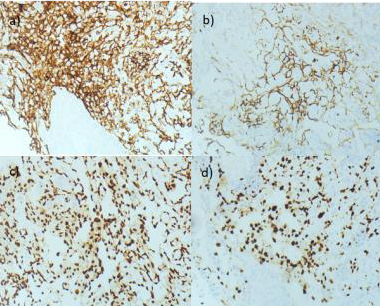
Immunohistochemistry indicated that CD31(+), CD34(+), D2-
40(+), ERG (+), CK (-), CK18(-), CD117(-), ki-67(50%+) [Figure 3a-d].
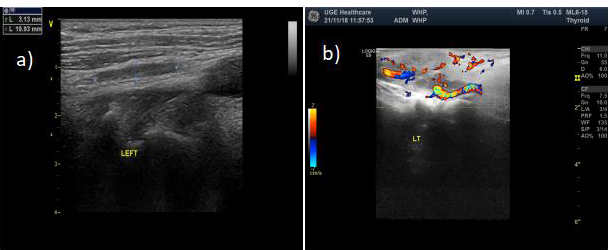
Cervical lymph node ultrasound did not indicate cervical lymph
node metastasis [Figure 4a,b]. Extensive excision of malignant scalp
tumor and skin grafting was performed on the right upper arm were
completed; pathology identified Hemangiosarcoma and all margins
were negative with perineural invasion [Figure 5a-c].
Ten days later, the patient came to the hospital to have the stitches
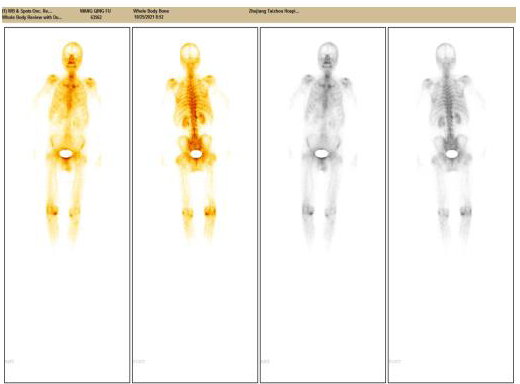
removed [Figure 1b].A staging PET/ CT scan revealed no systemic
metastasis [Figure 6].
But after one week, the patient returned to our department
for tingling pain on the left side of the head and face. On physical
examination, he had multiple blisters appeared on the left head and
face, the blisters were about the size of rice grains and the blisters
were clear and clustered into sheets. Some of the blisters were broken
Figure 1: Scalp clinical manifestations. a) Patient on admission; b) 10 days
after surgery; c)17 days after surgery; d) 31 days after surgery.
Figure 2: Scalp biopsy histology(200x). covered squamous epithelium,
subcutaneous lumen with abnormal hyperplasia, anastomosis, enlarged
endothelial nucleus, heterotypic, visible and schizotypic, incisal margin not clear.
Figure 3: Scalp biopsy histology.a)immunohistochemical staining for CD31
demonstrating positive cytoplasmicr staining, indicative of Cutaneous
angiosarcoma;b)immunohistochemical staining for CD34 demonstrating
positive cytoplasmic staining ,indicative of Cutaneous angiosarcoma;c)
immunohistochemical staining ERG demonstrating positive nuclear staining ;d)
immunohistochemical staining for ki-67 demonstrating positive nuclear staining.
Figure 4: Cervical lymph node ultrasound showed that there were multiple lowecho
nodes on both sides, with clear boundaries and capsula. The larger ones on
the left and right sides were 20*3mm and 17*5mm respectively (a), And the blood
flow signals in the nodules were not obvious; (b).
Figure 5: Postoperative scalp biopsy histology.a):Hemangiosarcoma of scalp
forming a 3.5*2.5*0.6cm mass which covered with squamous epithelium, and
the hypodermic dysplasia was observed(100x) ;b) Nucleolus could be seen,
the mitotic image was easily seen, the lamellar arrangement was observed,
and the abnormal hyperplasia lumen could be seen in some areas, which were
consistent with each other (200x); c)All margins were negative with perineural
invasion(200x).
Figure 6: A staging PET/ CT scan revealed Bone metabolism of the left side of
the parietal bone is mildly active(postoperative? Violation?)
and eroded, accompanied by a little exudation. The left eyelid was
red and swollen, and a lump about the size of a coin was visible
near the cheek of the left ear canal [Figure 1c]. It compatible with
herpes zoster were noted. Dexamethasone needles, penciclovir
needles and mecobalamin tablets were initiated. His pain eased after
1 week of treatment.But after two weeks, the patient returned to our
department for unbearable pain on the left side of her head and face.
On physical examination ,multiple nodules with hard texture and
poor mobility appeared at the margin of the skin graft area on the left
top of the head (Figure 1d).We recommend needle biopsy of scalp
induration to determine the nature of the scalp mass. The patient’s
family refused the treatment due to the patient’s age to continue with
morphine analgesic therapy.Follow-up 1 month later,the patient’s
family informed us that he passed away on December 23, 2021.
Discussion
Cutaneous angiosarcoma (cAS) has the worst prognosis among
all soft tissue sarcomas due to its multifocal, diffuse, invasive and high
recurrence rate [1]. cAS is very variable in clinical presentation and
can present as hematomatoid lesions, but also as rosacea, eczema,
hemangioma, purple spots or nodules, xanthoma, cellulitis, and
angioedema of the face and eyelids.Nodules, papules, plaques and
exophytic tumors appeared on the surface of advanced lesions [3].
If left untreated, these lesions grow rapidly and become multiple
highly elevated nodular lesions with bleeding areas [1]. A variety of
clinical manifestations of cAS have been reported in the literature,
while shingle-like manifestations are rarely mentioned, and they are
all treated as herpes zoster appearance at an early stage [2]. In the
case presented here. The patient developed post-operative ipsilateral
cephalic and facial herpes zoster appearance with intermittent
worsening neuralgia, and peripheral red induration in the
postoperative skin graft area. Subsequently, the patient developed red
induration around the skin graft area after surgery. Combined with
the advanced clinical manifestations reported in previous literature,
it was considered that the recurrence of sarcoma still needed
pathological support. The metastasis modes of cAS were mainly
hematogenous (metastasis to lung, liver, bone), lymphatic metastasis,
and local diffusion [4]. To date, PNI metastasis not been mentioned.By
referring to relevant literature, we found that relevant studies on PNI
in pancreatic cancer are relatively mature [5]. PNI is generally defined
as the occurrence of tumor cells along the nerve and/or in the nerve
sheath extraneuronal, extraneuronal, and intraneuronal, with cancer
cells surrounding at least 33% of the nerve, and the survival time of
patients with nerve invasion is significantly reduced compared with
those without nerve invasion, and the risk of local recurrence and
metastasis is significantly increased. Nerve growth factor (NGF) and
its receptor TrkA are highly expressed in pancreatic cancer tissues,
which can promote the proliferation and invasion of cancer cells
and is associated with poor prognosis and cancer pain of pancreatic
cancer [6]. Moreover, its high expression is more likely to find PNI
in pancreatic cancer tissues [7]. The postoperative pathology of the
patient indicated that nerve invasion (+). We consider recurrent and
progressive manifestations of hemangiosarcoma from red induration
around the skin graft area of the scalp, accompanied by ipsilateral
cephalic and herpes zoster appearance due to PNI metastasis, and
intermittent aggravation of neuralgia, resulting in a very short survival
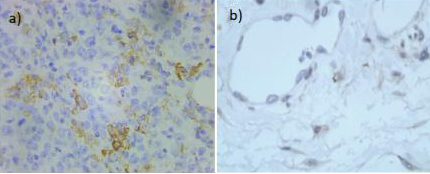
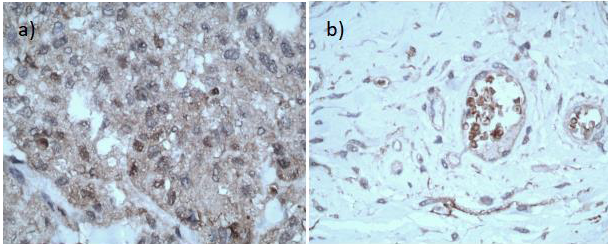
time.We used the monoclonal antibodies of NGF and TrkA ,and
selected the sarcoma tissue and paracancer tissue from the patient
for immunohistochemistry. The results indicated that the expression
of NGF and TrkA in the sarcoma tissue was positive [Figure 7a]
[Figure 8a], and the expression of TrkA in the paracancer tissue was
negative [Figure 7b] [Figure 8b]. It is speculated that there may be
PNI metastasis in cAS, which is associated with sarcoma progression,
increased local recurrence, intense pain, and poor prognosis.
Conclusion
cAS is a rare disease with poor prognosis,so the early recognition
of this entity is essential to start treatment and reduce the risk of longterm
sequela and even death.The cAS patient gave us the following
Figure 7: a) The sarcoma tissue: immunohistochemical staining for NGF
demonstrating positive nuclear and cytoplasmicr staining; b) The paracancer
tissue: immunohistochemical staining for NGF demonstrating negative
nuclear and cytoplasmicr staining
Figure 8: a) The sarcoma tissue: immunohistochemical staining for TrkA
demonstrating positive cytoplasmicr staining;b)the paracancer tissue:
immunohistochemical staining for TrkA demonstrating negative cytoplasmic
staining.
tips:
(1) Once cAS patients indicate nerve invasion,
immunohistochemical staining of pathological section NGF and
TrkA should be performed when necessary to determine whether
there is positive expression, so as to determine the possibility of PNI
metastasis.
(2) When such patients present with vesicular manifestations
accompanied by progressive aggravated neuralgia, they should be
highly vigilant about the possibility of sarcoma recurrence and PNI
metastasis, so as to actively take further treatment measures early to
prolong the life of patients as much as possible.
In this case,as the patient did not undergo pathological biopsy
around the skin graft area, it could not be determined whether the
patient died due to local recurrence and metastasis, or the trauma
caused by surgery, or other patient’s own causes. However, during
the whole process from diagnosis to final death of this patient, the
local clinical manifestations of cAS still have certain clinical reference
value.