Journal of Clinical & Medical Case Reports
Download PDF
Case Report
One Case of Iodine-125 Particle Implantation for Forehead Kimura’s Disease
Ye C1, Cao WH1*, Cai WC1 and Ye ER2
1Department of Plastic Surgery and Cosmetology, Taizhou Hospital of
Zhejiang Province Affiliated to Wenzhou Medical University, Taizhou,
China
2Department of Pathology, Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical University, Taizhou, China
2Department of Pathology, Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical University, Taizhou, China
Address for Correspondence: WeiHong Cao, Department of Plastic Surgery and cosmetology,
Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical University, China, E-mail Id: caoweihong@hotmail.com
Submission: 24 April, 2024
Accepted: 21 May, 2024
Published: 23 May, 2024
Copyright: © 2024 Ye C, et al. This is an open access article distributed under the Creative Commons Attribution License,which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords:Kimura’s Disease; Forehead Mass; Recurrence; Iodine-125
Particle Implantation
Abstract
Background: Kimura’s disease is a rare idiopathic inflammatory
disease of unknown etiology, often involving head and neck lymph
nodes. Because the clinical manifestations are not typical, the
diagnosis is difficult or it is misdiagnosed as malignant tumor. After the
diagnosis of Kimura’s disease, due to the high recurrence rate, surgery,
drugs, radiation and other comprehensive treatment methods are
often used. Here we present a rare case of forehead Kimura’s disease
from diagnosis to Iodine-125 implantation without recurrence.
Case Report: A 58-year-old man was diagnosed with Kimura’s disease and underwent 1 excision biopsy, 3 surgical excisions, and 2 postoperative recurrences. Since the patient refused to take oral immunosuppressants for a long period of time and local radiotherapy for several times, after the patient’s second recurrence resection, we used a gun implant to retrograde implant 125 iodide particles in the subcutaneous area of the forehead under local anesthesia with the consent of the patient, and implanted a total of 4 Iodine-125 particles at a interval of 1cm.After 1 year of implantation, the patient’s forehead mass showed no obvious protrusion and pruritus. After 1 year and 6 months of implantation, the patient’s forehead mass showed no obvious protrusion and pruritus, and the patient indicated satisfactory results.
Conclusion:When it is difficult to confirm the diagnosis of forehead skin masses with similar clinical manifestations as this patient, the possibility of Kimura’s disease should be considered, and comprehensive treatment such as surgery and adjuvant radiotherapy should be actively taken according to the pathological situation. Iodine-125 particle implantation may provide a new approach for the comprehensive treatment of Kimura’s disease patients to reduce postoperative recurrence. More clinical controlled studies are needed to confirm these findings in the context of radiation safety studies.
Case Report: A 58-year-old man was diagnosed with Kimura’s disease and underwent 1 excision biopsy, 3 surgical excisions, and 2 postoperative recurrences. Since the patient refused to take oral immunosuppressants for a long period of time and local radiotherapy for several times, after the patient’s second recurrence resection, we used a gun implant to retrograde implant 125 iodide particles in the subcutaneous area of the forehead under local anesthesia with the consent of the patient, and implanted a total of 4 Iodine-125 particles at a interval of 1cm.After 1 year of implantation, the patient’s forehead mass showed no obvious protrusion and pruritus. After 1 year and 6 months of implantation, the patient’s forehead mass showed no obvious protrusion and pruritus, and the patient indicated satisfactory results.
Conclusion:When it is difficult to confirm the diagnosis of forehead skin masses with similar clinical manifestations as this patient, the possibility of Kimura’s disease should be considered, and comprehensive treatment such as surgery and adjuvant radiotherapy should be actively taken according to the pathological situation. Iodine-125 particle implantation may provide a new approach for the comprehensive treatment of Kimura’s disease patients to reduce postoperative recurrence. More clinical controlled studies are needed to confirm these findings in the context of radiation safety studies.
Abbreviations
KD: Kimura’s disease; I125Iodine-125; ESR: Erythrocyte
sedimentation rate; CPR: C-reactive protein; ANCA: Antinuclear
antibody; RF: Rheumatoid factor; ANA: Antinuclear antibody; IgE:
Immunoglobulin E
Introduction
Kimura’s disease KD is a rare immune-mediated inflammatory
disease of unknown etiology. Its clinical manifestations are not
typical, mainly characterized by peripheral blood eosinophiliosis and
elevated serum IgE. The diagnosis mainly relies on Histopathological
examination, which often affects lymph nodes. A few literatures
have reported the occurrence of preauricular parotid gland and
posterior ear [1], and it is rare in the forehead. Literature have
proposed many treatment modalities include surgical resection,
systemic immunosuppressant’s combined with oral corticosteroids,
cyclosporine, mycophenolic acid or mycophenolic acid, targeted
therapy, fractionated radiotherapy or combination therapy [2]. The
treatment of KD with I125 implantation has not been reported.In this
case, we implanted I125 particles after surgical resection of the lesion
of rare forehead KD. After 1 year and 6 months of follow-up, it was
found that the patient had no obvious signs of recurrence, and the
treatment effect was satisfactory.
Case Report
A 58-year-old male with progressive enlargement of the left
forehead mass and left upper eyelid mass for 6 years came to our
Department of Plastic Surgery on February 17, 2021. Physical
examination showed that the left forehead mass was about 3*5cm,
protruding from the skin surface, centipede-like eminence, tough,
indistinct boundary, poor mobility, no obvious redness, swelling,
ulceration and exudation, accompanied by obvious pruritus, and no
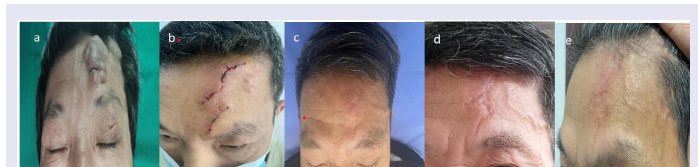
obvious swelling of superficial cervical lymph nodes [Figure 1a].
We are unable to determine the type of tumor and recommend
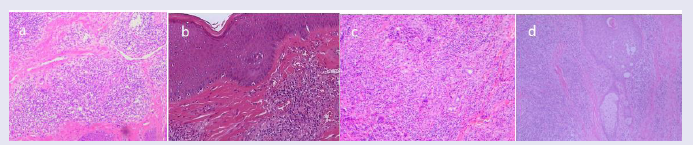
that treatment be determined after excision biopsy. The biopsy of the
left upper eyelid mass was completed, and the pathology revealed that
the skin tissue (left upper eyelid) was accompanied by granulation
tissue hyperplasia [Figure 2a].
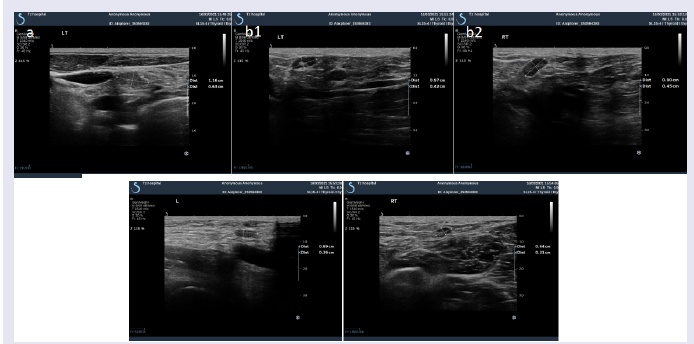
Systemic lymph node ultrasound: multiple lymph nodes on the
left neck (partial shape full), multiple lymph nodes on both sides of
the axilla (partial shape full), multiple lymph nodes on both sides
of the groin region and no retroperitoneal enlarged lymph nodes
[Figure 3a-c].
Peripheral blood eosinophil ratio was 13.7%, higher than the
normal range0.4-8.0%, and peripheral blood eosinophil value
was 0.73*10^9/L, higher than the normal range0.02-0.52*10^9/L.
Immunoglobulin A, G, M, ESR, CPR were all in normal normal
range. ANCA, RF and ANA were all negative. IgE levels were not
detected. The possibility of Kimura’s disease was not considered. It
is recommended to go to a superior hospital for diagnosis and then
determine the final treatment plan. On April 10, 2021, On April 10,
2021, the patient required surgical resection to our Department due to
Figure 1:Forehead clinical manifestations. a: Patient on admission; b: 7 days after first surgery, c: First recurrence; d: 1 year after 1125 particles implantation, e: 1 year and 6 months after 1125 particles implantation.
Figure 2: Postoperative biopsy histology.
a: Surface squamous epithelium, angiogenesis, more lymphoid tissue, eosinophilic infiltration (100x) b: The epidermal squamous epithelium showed lymphoid follicles in the dermis, small vessel proliferation, numerous lymphocytes, eosinophilic infiltration, and eosinophilic microabscess formation (100x), c. Epidermal
squamous epithelium, interstitial parenchyma multiple parenchymal hyperplasia, perivascular lymphoid tissue hyperplasia, lymphocyte, plasma cell and a few eosinophils infiltration, lymphoid follicles formation (100x) d: The squamous epithelium was covered with hyperkeratosis and hypokeratosis on the surface.
The dermis showed more small vessels with cluster hyperplasia, infiltration of lymphocytes, plasma cells and eosinophilic granulocytes, formation of lymphoid follicles, and a few multinucleated giant cells were seen in the focal area (100x).
the size of the forehead mass which seriously affected the appearance
and accompanied by obvious pruritus.The forehead mass was
completely removed. Postoperative pathology revealed: eosinophilic
lymphogranuloma (Kimura’s disease) (Figure 2b).The stitches were
removed one week after surgery (Figure 1b), and We informed
the patient that KD was likely to recur and suggested continued
treatment with oral medication after surgery, but the patient refused.
On October 29, 2021, the patient came to our Department due to
“recurrent forehead mass requiring another operation”. Physical
examination: old surgical scar on the left forehead. Some skin
ridges can be seen on the surgical scar about 2*2cm, slightly higher
than the skin surface, with poor mobility and no obvious redness,
swelling and ulceration (Figure 1c).Peripheral blood eosinophil
ratio was normal (3.6%) and peripheral blood eosinophil value was
normal (0.20*10^9/L).Postoperative pathology: chronic cutaneous
inflammation with lymphoid hyperplasia (Figure 2c).We consider
the patient with recurrent forehead KD. We recommend that patients
take medication after surgery to reduce recurrence. The patient
stopped taking cyclosporine orally after 2 weeks. On May 21, 2022,
the patient complained of a small amount of swelling in the forehead,
accompanied by pruritus, and requested another surgical resection.
Postoperative pathology: chronic inflammation of skin tissue with
more small vessel hyperplasia and eosinophilic infiltration in dermis
(Figure 2d). We told him that he needed regular medication or
local external radiation therapy to reduce postoperative recurrence.
Patients worried about the side effects of drugs, but also because of the
inconvenience of repeated visits to the hospital to refuse radiotherapy.
In our department, for patients with head and neck skin tumors, I125
particle implantation is frequently applied to reduce postoperative
recurrence. We consulted relevant literature on iodine-125 and
Informed patients that after Iodine-125 particle implantation, it is
recommended to stay away from relatives and caregivers for more
than 1 meter for 2 months, and stay away from pregnant women and
children for 3 months. The patient said that there were no pregnant
women and children in his family, which was acceptable. With the
consent of the patient, a total of 4 I125 particles were implanted in the
subcutaneous area of the forehead under local anesthesia one week
after the stitches were removed using a gun implant in a retrograde
way, with an interval of 1cm and an activity of 0.5-0.7mci for each
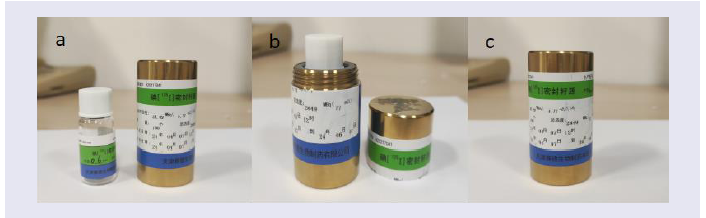
particle. At the same time, we also gave the patient a lead vial [Figure 4]
after the operation, and told the patient to recover and come to
the hospital in time once radioactive materials were found to be
discharged. During the follow-up period of 1 year and 6 months, the
patient reported that no particle discharge was found. During the
follow-up, we also suggested that the patient come to the hospital for
reexamination of whole body radionuclide tomography and internal
organ radionuclide tomography to check the location and quantity
of Iodine-125 particles in the body. The patient was refused on the
grounds of inconvenience.
Figure 3:Systemic lymph node ultrasound
a: Cervical lymph node ultrasound: On the left neck, there were several low-echo nodules with clear boundaries, some of them were full in shape and had
envelopes, the larger one was about 12*6mm, and blood flow signals could be seen inside. There was no obvious enlarged lymph node echo in the right neck.
b(1,2): Axillary lymph node ultrasound: Multiple hypoechoic nodules can be seen in both axillary pits, with clear boundaries, envelopes, and some of them are
full in shape. The larger one on the left side is about 104mm(b1), and the larger one on the right side is about 95mm(b2). The blood flow signals in the nodules
are not obvious.
c(1,2):Inguinal lymph node ultrasound:Multiple hypoechoic nodules can be seen in the two sides of the inguinal region, with clear boundaries and envelopes,
the larger one on the left side is about 94mm(c1), the larger one on the right side is about 63mm(c2), and the blood flow signal in the nodules is not obvious.
Figure 4:Lead Containers are used to store expelled Iodine-125 particles: save as shown in figure (a,b,c).
During the follow-up within 1 year after surgery, there were no
obvious protrusions or pruritus in the patient’s forehead mass [Figure 1d].
After 1 year and 6 months of follow-up, the patient’s forehead
mass showed no obvious protrusion and pruritus [Figure 1e], and the
patient indicated that the effect was satisfactory.
Discussion
Kimura’s disease (KD), also known as eosinophilic
lymphogranuloma or eosinophilic proliferative lymphogranuloma, is
a rare chronic immune inflammatory disease with unknown etiology,
which is difficult to diagnose due to its similar benign or malignant
disease and low incidence. Although some histological identification
is helpful in distinguishing KD, more clinical features are needed to
differentiate the diagnosis. General clinical manifestations include
subcutaneous nodules, lymph node enlargement, salivary gland
hypertrophy accompanied by peripheral blood eosinophilia and
elevated serum IgE [3]. Mainly manifested in lymph nodes, few
literature reported the occurrence of preauricular parotid gland and
posterior ear [1], and rarely occurred in the forehead. Pathological
examination is the gold standard for the diagnosis of KD, and it is
difficult to confirm pure fine-needle biopsy or partial biopsy, which
needs to be confirmed by surgical specimen. It is locally aggressive
and can lead to facial paralysis if left untreated, so it is critical to
improve the diagnosis rate at the first visit. We did not confirm KD
at the first biopsy to remove the left upper eyelid mass. The pathology
of KD was not confirmed until after the second complete resection of
the forehead mass. The clinical manifestations of this case can be used
as a reference for differentiating the head and face mass, which can
improve the diagnosis rate of the first visit.
At present, there is no standard guideline or consensus on
the treatment of the disease. Previous literature has proposed
a variety of treatment modalities, including surgical resection,
systemic immunosuppressant combined with oral corticosteroids,
cyclosporine, mycophenolic acid or mycophenolic acid, targeted
therapy, fractionated radiotherapy or combined therapy, systemic
steroids, immunosuppressive drugs and radiotherapy, etc. Resulting
in local recurrence rates ranging from 41.2% to 100% [3-5]. In a
previous meta-analysis, surgical excision and adjuvant radiotherapy
had the lowest recurrence rate at 8.3% [4,5].
KD is sensitive to radiation therapy, which has been advocated
for patients with positive surgical margins, patients with repeated
postoperative recurrence, and patients with refractory recurrence
during systemic steroid therapy. In order to avoid radiation damage
and the potential risk of radiation cancer, low-dose radiotherapy is
advocated. Recent literature has reported that KD can be well locally
controlled at a radiation dose of 30-40 Gy for 3-4 weeks, and late
toxicity is not obvious. It is suggested that radiotherapy should be
one of the first treatment methods for KD, whether it is primary or
recurrent [6]. In this case, the patient refused low-dose radiotherapy
due to the long duration and inconvenience of travelling to and from
the hospital.
In our department, for patients with head and facial skin
tumors, I125 particle implantation is frequently applied to reduce
postoperative recurrence. The particle source core is a palladium
wire of 125 iodine-particle radionuclide, clad in a cylindrical sealed
titanium alloy tube, with a half-life of 59d and an average energy
of 27 ~ 35 keV, which is commonly used in brachytherapy. The
killing mechanism of the cells is summarized as follows: After the
implantation of radioactive particles, through the release of a large
number of X-rays and gamma rays, the cell mitosis is suppressed,
the DNA of the nucleus is destroyed, and oxygen free radicals are
generated to continuously kill the cells, thus shrinking the lesions and
reducing the further progression of the lesions, and thus significantly
improving the quality of life of patients.
125I is a low-energy radioisotope that, outside the therapeutic
target volume, rapidly reduces dose deposition to tissue with distance
from the radioactive source due to its low penetration, resulting in
limited damage to normal tissue. Compared with soft tissue, bone
tissue is denser and has a better attenuation effect on radiation. [7]
In the studies on the treatment of early parotid ACC, it has been
reported that iodine-125 particle implantation in parotid gland is an
effective and safe method with low radiation toxicity [8]. It has also
been reported that I-125 particle implantation radiotherapy in the
average range of 94.15 Gy (62.31 ~ 128.39 Gy) in the treatment of
spinal metastatic tumors still has no serious complications, which is
safe and effective [9].
However, I125 particle implantation into KD lesions for internal
radiotherapy of KD lesions has not been reported at home and abroad.
Our studies on iodine-125 and KD suggest that the penetrability of
iodine-125 particles for KD is moderate, its energy is low enough,
and its inhibition and killing effects on lesions are effective and longlasting,
with less radiation damage to neighboring tissues.
Generally, the recommended dose of external superficial
radiotherapy for KD is 20-40Gy. As there have been no reports on
internal radiotherapy with I125 particles implanted in KD patients,
our center has not conducted large-scale controlled studies, so a
more accurate assessment of effective radiation dose and radiation
safety cannot be obtained. But we believe that the dose is comparable
or moderately reduced to that of external radiotherapy. Forehead
subcutaneous implantation through the skull attenuation, the dose
is lower, we believe that the impact on brain tissue is less, is safe and
effective.
With the informed consent of the patient, 125 iodized particles
were implanted subcutaneously in the patient’s forehead after the
second recurrence of surgery, with 1 iodized particle implanted
every 1cm or so, and a total of 4 iodized particles were implanted.
No tumor regeneration, no obvious pruritus, no colorless, and no
color loss were observed in the forehead during follow-up 1 year and
1 year and 6 months after surgery. We concluded that I125 particle
implantation in this patient has achieved good clinical efficacy in
controlling postoperative recurrence in KD patients. Although no
recurrence was detected during the 1 year and 6 months follow-up,
further monitoring was required. Future studies are also needed
to further explore the recommended clinical dose limits for I125
particle implantation for KD.The literature suggests that for 125I
implantation patients, work colleagues, non-pregnant adults who do
not share a bed with the patient, or non-pregnant adults who share a
bed with the patient do not need to take precautions. A typical 125I
patient should only avoid sleeping in the “spoon” position (i.e. contact
with a pregnant woman) and avoid holding the child on their lap for
prolonged periods of about 2 months [10].We also inform patients of
precautions before Iodine-125 particle implantation and carry out the
above education after surgery.
In this case, the reasons for the patient’s recurrence twice after
surgery may be as follows: 1. The pathogenic factors were not
removed, leading to local recurrence of the lesion; 2. The lesion is
highly invasive and heavily adhered to the surrounding tissue,
making it difficult to completely resect. There was no recurrence after
I125 implantation because I125 could inhibit the residual lesions
for a long time. However, due to the inconvenience of the patient
coming to the hospital, the radiation dose was not determined, and
the duration of particle inhibition on the lesion and late toxicity still
need further follow-up. The possibility of spontaneous regression
[11] and complete resection of the lesion after multiple operations
cannot be ruled out. We want to further explore the dose-biological
effects of I125 particles on the clinical treatment of KD and explore
its molecular mechanism. More clinical controlled studies are needed
to confirm these findings in the context of radiation safety studies.
Conclusion
Kimura’s disease is a rare, difficult to diagnose and recurrent
inflammatory disease. This KD patient gives us the following tips:
(1) KD should be considered when the patient has a forehead mass
that is difficult to diagnose and has similar clinical manifestations
as this patient, and comprehensive treatment such as surgery and
adjuvant radiotherapy should be actively taken according to the
pathological situation. (2) I125 particle implantation can provide a
new therapeutic idea for comprehensive treatment of KD patients
and reduce postoperative recurrence. More clinical controlled studies
are needed to confirm these findings in the context of radiation safety
studies