Journal of Clinical & Medical Case Reports
Download PDF
Case Report
Candida Duobushaemulonii and Trichosporon Asahii in Hematopoietic Stem Cell Transplant Patient: A Rare Bug in Febrile Neutropenic Patient
Goutham KJ¹, Rubaina A¹, Delvin K¹, Nishit², Yesheswini N², Aswathy AN³, and Sachin SJ⁴*
1Department of Clinical pharmacology, HCG Cancer Hospital, Bangalore
2Junior consultant , Department of Hematology & stem cell transplant, HCG Cancer Hospital, Bangalore
3Department of nursing, Hematology & stem transplant, HCG Cancer Hospital, Bangalore
4Group Head, Hematology & stem cell transplant, HCG Cancer Hospital, Bangalore
2Junior consultant , Department of Hematology & stem cell transplant, HCG Cancer Hospital, Bangalore
3Department of nursing, Hematology & stem transplant, HCG Cancer Hospital, Bangalore
4Group Head, Hematology & stem cell transplant, HCG Cancer Hospital, Bangalore
*Address for Correspondence:Sachin Suresh Jadhav, Group Head Haematology & SCT HCG
Cancer hospital Bangalore E-mail Id: drsachinjadhav@gmail.com
Submission:13 April, 2024
Accepted: 16 May, 2024
Published:20 May, 2024
Copyright:© 2024 Goutham KJ, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords:Candida duobushaemulonii; Trichosporon asahii; Aplastic
anemia; Bone marrow; Stem cell transplant; Echinocandins; Azole
antibiotics
Abstract
Aplastic anemia is defined by profound reduction in number of
bone marrow- Hematopoietic stem cell or Hematopoietic progenitor
cell. Fungal infection is the second cause of infections caused in
hematopoietic stem cell transplant patients, with viral infection being
first and bacterial accounts third. Candida duobushaemulonii is an
emerging pathogen, given its resistance to multiple antifungal (to
azoles and amphotericin B) it poses a substantial problem of causing
invasive infection in immunocompromised setting. The Candida
duobushaemulonii requires molecular based method for accurate
identification and the conventional/ traditional biochemical method
is currently inadequate. Trichosporon asahii is one of the most common
species of trichosporon genus, which is a rare fatal emerging fungal
infection whose occurrence has increased in immunocompromised
patients with blood disease. A 58-year-old patient was diagnosed to
have very severe aplastic anemia and febrile neutropenia post stem
cell transplant.On basis of Sputum analysis the patient was diagnosed
to have aspergillus pneumonia with High resolution computed
tomography showing moderate pleural effusion and blood and
urine culture revealed presence of fungal infections for which he was
then started on antibiotics and antifungal. Blood Culture revealed
that Candida duobushaemulonii was resistant to fluconazole and
voriconazole and had a good sensitivity to echinocandins hence
the patient was started on inj Anidulafungin 100 mg OD for 12 days.
After 3 days the patient became hypoxic, required 2 litres of oxygen
through face mask to maintain saturation, the urine and blood culture
were sent in which urine culture reports showed Trichosporon asahii
which was then treated with inj Anidulafungin 100 mg after which the
patient was stable and afebrile. Echinocandins are more susceptible
to Candida duobushaemulonii whereas azoles and amphotericin
B are resistant. EarlyAnalysis of the risk factor to develop Candida
duobushaemulonii and Trichosporon asahii priorto stem cell transplant
is required and possibly will help in identifying this rare fungal infection
by using molecular method rather than by using a traditional method
and it also helps in choosing a better prophylactic antifungal.
Introduction
Aplastic anemia is defined by profound reduction in number of
bone marrow- Hematopoietic stem cell or Hematopoietic progenitor
cell (HSCs/HPCs) which is characterized by hypocellularity or
aplastic bone marrow or an “empty” BM, which is been replaced
precociously with fat cells. [1] This results in production of defective
mature blood cells and peripheral pancytopenia. The incidence rate
of aplastic anemia is 1-2 patients per million inhabitants per year.
[2]
Although few decades ago Aplastic anemia was considered
almost fatal universally, the Aplastic anemia can now be ameliorated
and cured by immunosuppressive treatment or by stem cell
transplantation. [3]
Hematopoietic stem cell transplant leads to various complications
in post- engraftment period due to the immunosuppression caused
by radiation, chemotherapy or immunosuppressive agents and type
of conditioning treatment (myeloablative or reduced intensity) given
prior to transplantation or presence of acute GVHD. [4,5] Were
infectious complication (bacterial/viral/fungal) account for most of
the morbidity and moratlity. [4] fungal infection stands second in
infections (4%) caused in hematopoietic stem cell transplant patients,
with viral infection being first and bacterial accounts third. [6]
C. duobushaemulonii is a long lasting but rare and unidentified/
misidentified fungal species. [7-9] Candida being genetically
heterogenous forms various complex which are phenotypically
identical making its accurate identification difficult. One of such
complexes is Candida haemulonii, which is classified into 2 species
such as C. Haemuloni sensu stricto and C. duobushaemulonii.
[7,8]
C. duobushaemulonii is an emerging pathogen, given its
resistance to multiple antifungal (toazoles and amphotericin B)
poses a substantial problem causing more invasive infection than
previously appreciated. But the species is sensitive to echinocandins.
[8]
The candida duobushaemulonii requires molecular based
method for accurate identification andthe conventional/ traditional
biochemical method is currently inadequate and cannot identify this
species accurately. [9]
>90% of fungal infections in post hematopoietic stem cell
transplant patients is caused by Candida, Aspergillosis and
Cryptococcus. Where Candida being main cause for bloodstream
infection during the pre- engraftment period of hematopoietic
stem cell transplant. [10] Many studies shows that Aspergillus
and candida albicans is most common pathogen causing fungal
infection in hematopoietic stem cell transplant in patients (where
incidence of candida albicans has been decreased with prophylactic
use of azole antifungals).[6] But there are no studies showing the
Candida duobushaemulonii infection in post hematopoietic stem cell
transplant patients.
Although the overall incidence of invasive fungal infection is 4%
in hematopoietic stem cell transplant patients, but in patients with
allogenic SCT the mortality rate is as high as 13%. [6] Trichosporon
asahii formerly called Trichosporon bigelli is one of the most common
species of Trichosporon genus, which is a rare fatal emerging fungal
infection whose occurrence has dramatically increased in recent
years, most frequently in immunocompromised patients with blood
disease. [11-13] it is one of the causes of fatal life threatening invasive
fungal infections (IFI) occurring in hematopoietic stem cell transplant
recipients or in patients with cancer and neutropenia, [12] Soil and
water, plants, and colonizing the human mouth, gastrointestinal
tract, respiratory tract, vagina, skin, and urine can can serve as a be
the major source of habitat for trichosporon species. [13]
The T. asahii has reduced susceptibility to antifungal therapy in
immunocompetent and immunocompromised patients especially in
patients receiving broad- spectrum antibiotics for a long period, in
heavy alcoholics, or in diabetic patient even in healthy individuals
[14]
Case Report
A 58-year-old male patient came to Outpatient department
with complains of a non-healing ulcer on his leg and epistaxis two
months back. The patient was found to have pancytopenia. Later he
developed fever after which sputum analysis was done which showed
aspergillus pneumonia and blood and urine culture revealed presence
of fungal infections for which he was then started on antibiotics and
antifungals.
Later he was shifted to our hospital, in view of severe hypoxia,
the patient was shifted to ICU and was managed symptomatically.
The patient was diagnosed to have very severe aplastic anemia with
HB of 6.8 g/dl and febrile neutropenia. The patient was started on
inj Teicoplanin, inj Ceftazidime avibactum and inj Azetreonam along
with anti-fungal prophylaxis of Isavaconazole and viral prophylaxis
tab acyclovir which was then changed to tab Valacyclovir. Herpes
simplex virus liver showed hypo dense lesion in the liver. Bone
marrow aspiration and biopsy was done which revealed hypo cellular
marrow. The patient was known case of paroxysmal nocturnal
hemoglobinuria and hepatitis B positive and tab Tentide AF was
added for further management.
Bronchoscopy BAL was done which revealed a poly-microbial
infection with Aspergillus,Staphylococcus aureus, Klebsiella
pseudomonas candida, Enteriobacteriaceae. The same antimicrobials
were continued throughout the ICU admission the patient received
inj Teicoplanin for 17 days, inj Ceftazidime avibactum and inj
Azetreonam for 14 days along with anti-fungal prophylaxis of
Isavaconazole for 20 days which was then changed to tab Voriconzole
and viral prophylaxis tab Acyclovir which as then changed to tab
Valacyclovir 1 gm and continued. He was then planned for matched
identical allogenic stem cell transplantation with his donor 9/10
match. The patient underwent stem cell infusion and achieved
neutrophil engraftment on day +12 and platelet engraftment on day
+15.
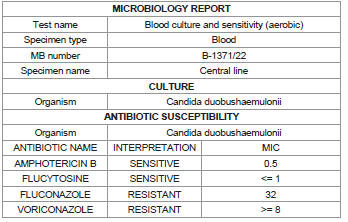
Patient on day -2 of transplant developed febrile episodes, so
cultures and molecular panel were sent. Molecular PCR and blood
culture revealed Candida duobushaemulonii and urine culture
showed growth of Aeromomas hydrophila and E. coli (Multi Drug
Resistant), in view of febrile neutropenia the patient was started
on inj Ceftazidime avibactum 2.5 g for 16 days and the patient was
stable. Cultures revealed that Candida duobushaemulonii was
resistant to fluconazole and voriconazole and had a good sensitivity
to echinocandins hence the patient was started on injAnidulafungin
100 mg OD for 12 days. After 12 days the blood cultures showed no
growth for any organisms and the patient was stable and afebrile
which showed that anidulafungin monotherapy was effective enough
for the treatment of candida infections.
After 3 days (day +11 of transplant) the patient became hypoxic,
required 2 litres of oxygen through face mask to maintain saturation,
post which repeat high-resolution computed tomography (HRCT)
was done which showed interval increase in pleural effusion. The urine
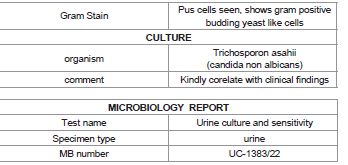
and blood culture were sent in which urine culture reports showed
Trichosporon asahii which was then treated with inj Anidulafungin
100 mg after which the patient was stable and afebrile.
The patient was started with inj anidulafungin 100 mg OD after
the first molecular pannel report, after 5 days of treatment repeat
blood cultures were obtained which did not show any organisms.Since
urine culture developed Trichosporon asahii, inj Anidulafungin 100
mg OD was continued for a total of 7 days which showed a significant
improvement in the patient as well as urine culture showing no growth
of any organisms. hence a total course of 12 days of inj Anidulafungin
100 mg OD was effective for treatment of multi species fungal
infection in blood as well as urine for a post hematopoietic stem cell
transplant patient with significant improvement in patient health.
Discussion
Although few decades ago Aplastic anemia was considered almost
fatal universally, the Aplastic anemia can now be ameliorated and cured
by immunosuppressive treatment or by stem cell transplantation.
[3] A study suggest an improved outcome can be seen in acquired
aplastic anemia patients with hematopoietic stem cell transplantation
when compared with conventional immunosuppressive therapy.[5]
Hematopoietic stem cell transplant leads to various complications
in post- engraftment period due to the immunosuppression caused
by radiation, chemotherapy or immunosuppressive agents, use of
corticosteroids and type of conditioning treatment (myeloablative or
reduced intensity) given prior to transplantation or presence of acute/
chronic GVHD or through catheter and central/peripheral insertion.
[4-6]
These complications include myelosuppression with neutropenia,
anemia, thrombocytopenia,sinusoidal obstruction syndrome (SOS),
mucositis, acute or chronic GVHD, gram positive/ gram negative
infections, HSV, CMV, Candida and Aspergillosis. [5,10] Were
infectious complications account for most of the morbidity and
mortality. [4] The recovery and reconstitution of immune system is
more rapid in autologous hematopoietic stem cell transplant than
in allogenic hematopoietic stem cell transplant. This is because the
allogenic hematopoietic stem cell transplant Recipients under goes a
long-term immunosuppressive therapy for chronic GVHD. [4] hence,
more negative outcomes of fungal infections are seen in allogenic
hematopoietic stem cell transplant when compared with autologous
hematopoietic stem cell transplant.[6]
C. duobushaemulonii is a long lasting but rare and unidentified/
misidentified species. [7-9] The misidentification of these species may
be related to the inaccurate biochemical methods used to identify
the species, thus requiring molecular based methods to guarantee
its accurate identification. [7,9] According to study by Irene Jurado-
Martin et al, they discovered that the isolate identified in 1996 as
C. intermedia by API®ID 32C was actually a C. duobushaemulonii.
[7] Neutropenia and mucosal damage present during the preengraftment
period are risk factors to develop invasive candidiasis. As
the neutropenia and mucosal skin loss recovers in post engraftment
period the risk of developing candida infection decreases. [4]The
incidence of fungal infections in post engraftment period can be
reduced by use of prophylactic antifungal for 1 month following
transplant, usually with fluconazole or voriconazole (in patients with
high risk profile). [5,10] in pre- engraftment period the prophylactic
antifungal treatment has been shifted from amphotericin B to
itraconazole, voriconazole and echinocandins, which have shown
better efficacy and decreased adverse effects. [6]
According to literature the candida species especially the
complex candida species showed the reduced susceptibility to
fluconazole, itraconazole and Amphotericin B, but where susceptible
to echinocandins making it the best treatment options for infections
caused by complex candida species. The tendency of complex species
to develop resistance to azoles, echinocandins and amphotericin B
increase the importance of identifying these rare or uncommon
species. [7,8] Trichosporon asahii is one of the most common
species of Trichosporon genus, which is a rare fatal infection whose
occurrence has dramatically increased in recent years, most frequently
in immunocompromised patients with blood disease. [11-13]
The growth of Trichosporon asahii was most common in urine
culture (27.9%) when compared to other cultures, hence affecting
urinary system most frequently (28.6%). The review shows the risk
factor associated with this fungal infection was antibiotics use being
highest, followed by invasive medical equipment, chemotherapy,
neutropenia, bacterial infection, ICU hospitalization, glucocorticoids
use, immunosuppressant and trauma being the least frequent risk
factor. [11]
Conclusion
To accurately identify the species which forms complex for
example Candida duobushaemulonii in our case which is one of the
complexes of Candida haemulonii it is required to use molecular
based method of identification. This will lead to a proper study of
its prevalence, susceptibility and resistance pattern. Echinocandins
are more susceptible to Candida duobushaemulonii whereas azoles
and amphotericin B are resistant. Early Analysis of the risk factor to
develop Candida duobushaemulonii and Trichosporon asahii prior
to stem cell transplant is required and possibly will help in identifying
this rare fungal infection by using molecular method rather than
by using a traditional method and it also helps in choosing a better
prophylactic antifungal rather than only focusing on most common
fungal infections such as candida albicans or Aspergillosis.
Acknowledgement
The Authors wish to thank Department of Hematology,
Department of Clinical Pharmacology,HCG Cancer Hospital.
Author Contributions:
All authors helped in data acquisition, manuscript preparation,
read and approved the final manuscript, and guarantees the integrity
of the study.