Journal of Clinical & Medical Case Reports
Download PDF
Case Report
Unveiling Tuberous Sclerosis Complex: A Case Report of Seizure Disorder and Inherited Predisposition
Shrestha A1, Fatima M2, Joti S1, Yadav A1*, Gurung A3, Tamang S4 and Shrestha N5
1Medical Officer, Silverline Hospital, Balaju, Kathmandu, Nepal
2Candidate MMSCI (Master of Medical Science)’25, Harvard Medical School, USA
3Medical Officer, KIST Medical College and Teaching Hospital, Lalitpur, Nepal
4Medical Officer, Stupa Community Hospital, Boudha, Kathmandu, Nepal
5Medical Officer, Kharanitar Hospital, Nuwakot , Nepal
2Candidate MMSCI (Master of Medical Science)’25, Harvard Medical School, USA
3Medical Officer, KIST Medical College and Teaching Hospital, Lalitpur, Nepal
4Medical Officer, Stupa Community Hospital, Boudha, Kathmandu, Nepal
5Medical Officer, Kharanitar Hospital, Nuwakot , Nepal
Address for Correspondence:Ashmita Yadav, Medical Officer, Udayapur District Hospital,
Udayapur, Nepal. Email Id: ashmitayadav84@gmail.com
Submission:25 September, 2024
Accepted:24 October, 2024
Published:30 October, 2024
Copyright: © 2024 Shrestha A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords:Tuberous sclerosis; Seizure; Adenoma; Sebacum
Abstract
Tuberous sclerosis complex (TSC) is an autosomal dominant
genetic disorder with high penetrance and extensive clinical variability
that affects multiple organ systems: the skin, brain, kidneys and
heart. It is characterized by a variety of dermatological symptoms
like angiofibromas, periungual fibromas, shagreen patch, and leaf
macules, as well as neurological manifestations such as seizures,
mental retardation and behavioral disorders. A typical clinical triad
comprising epilepsy, intellectual disability, and adenoma sebaceum
defines TSC.
We present a case report of an 18-year-old male with characteristic clinical and radiological features of tuberous sclerosis complex having a significant family history. The patient admitted to the hospital with features of status epilepticus revealed multiple hypo pigmented macules, adenoma sebaceum in a butterfly pattern, shagreen patch on the abdomen and a nodule in the fingertip, likely periungual fibroma thus fulfilling 5 major criteria of TSC. Patient also had a slightly impaired mental status. A tiny sub-enendymal nodule on brain MRI also supported the case. In general, only one-third of the disease is hereditary, while the rest are sporadic in nature. But significant family history is reported in our case where the 2 generations seem to be affected in sequence with variable manifestations. The severity has been noticed to be more in 2nd generations, mostly the younger siblings.
This case report intends to raise awareness of this illness among medical professionals and improve patient care. Further research on the genetic association of TSC and its severity as per generations needs to be evaluated to bring out more accurate statistical information. It is imperative to let the medical community know about the underlying condition, producing seizures to reduce the morbidity and mortality of this disease.
We present a case report of an 18-year-old male with characteristic clinical and radiological features of tuberous sclerosis complex having a significant family history. The patient admitted to the hospital with features of status epilepticus revealed multiple hypo pigmented macules, adenoma sebaceum in a butterfly pattern, shagreen patch on the abdomen and a nodule in the fingertip, likely periungual fibroma thus fulfilling 5 major criteria of TSC. Patient also had a slightly impaired mental status. A tiny sub-enendymal nodule on brain MRI also supported the case. In general, only one-third of the disease is hereditary, while the rest are sporadic in nature. But significant family history is reported in our case where the 2 generations seem to be affected in sequence with variable manifestations. The severity has been noticed to be more in 2nd generations, mostly the younger siblings.
This case report intends to raise awareness of this illness among medical professionals and improve patient care. Further research on the genetic association of TSC and its severity as per generations needs to be evaluated to bring out more accurate statistical information. It is imperative to let the medical community know about the underlying condition, producing seizures to reduce the morbidity and mortality of this disease.
Introduction
Tuberous sclerosis complex is known as a neurocutaneous
disease characterized by variety of dermatological symptoms like
angiofibromas, periungual fibromas (Koenen’stumors), shagreen
patch and leaf macules, fibromatous plaque as well as neurological
manifestations including seizures, mental retardation and behavioral
disorders.[1] It is an autosomal dominant genetic disease that
affects multiple organ systems.[2] In 1862 Von Recklinghausen
first described the disease.[3] Then Désiré-Magloire Bourneville
first demonstrated the pathologic brain lesions in 1880 and termed
“sclerosetubereuse”(tuberous sclerosis). Due to having various extra
cranial manifestations, it is termed as “tuberous sclerosis”. According
to his name, it was also called “Bourneville’s Disease”.[4,2] A typical
clinical triad comprising epilepsy (EPI), intellectual disability (LOI),
and adenoma sebaceum (A), defines TS.[4] A recent study reported
that about 80% of children with TS have epilepsy. The same study
established that about 44% of the respondents had mental retardation,
which was profound in two thirds of cases (IQo21). Patients without
a history of seizures are extremely unlikely to have a significant
learning problem.[5] People with TSC often acquire epilepsy within
the first year of life, however people with TSC who have never had
seizures continue to have a higher risk of developing epilepsy.
[6]
Here we present a case report of a 18 years old male with
characteristic clinical and radiological features of tuberous sclerosis
complex having significant family history. It is imperative to let
the medical community know about the underlying condition that
produces seizures in order to reduce the morbidity and mortality
of this disease. By disseminating this case report, we intend to raise
awareness of this illness among medical professionals and improve
patient care. This article was previously presented as a meeting
abstract at the 2023 Bangladesh International Medical Students
Scientific Congress (BIMSSCON) on 12 May, 2023.
Case Presentation
An 18 yrs old male was admitted to The Department of Medicine,
Mymensingh Medical College Hospital, Mymensingh, Bangladesh
with presentation of status epilepticus. On query, he was on
antiepileptic drugs for the last 8 years as recommended by primary
health center but the control was very unsatisfactory. He used to have
several episodes of generalized tonic clonic convulsion lasting for 7-8
minutes occuring at intervals of 3-4 min that relieved spontaneously.
However due to their economic constraints it was not possible for
his family to take further consultation. The status epilepticus was
managed accordingly then further examination was done which
imparted GCS= E1V1M3, pulse 80 bpm ,blood pressure 130/80,
absence of bilateral Babinski sign, absence of meningeal irritation
sign, decreased tone in both lower limbs, loss of deep tendon reflex.
There were bumpy areas in the head, multiple hyperpigmented
papular growth over the nasolabial region in a characteristic butterfly
pattern consistent with adenoma sebaceum [Figure 1]. We also noticed
multiple (about 5) hypopigmented macules (ash leaf pattern) [Figure 2] with diameter greater than 5mm in body especially in trunk and abdomen along with a well defined roughened hypermelanotic patch
region showing orange peel appearance indicative of Shagreen patch
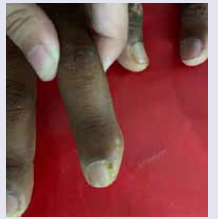
on his abdomen near left flank [Figure 3]. A nodule was present in the
finger tip with degenerative change of nail likely periungual fibroma
[Figure 4]. Other systems revealed no significant abnormality.
Further neurological examination was done to evaluate the
mental status. Upon inquiry he was dropped out from school due
to episodes of convulsion in his early childhood. Higher psychic
function test revealed he is slightly unable to follow commands
immediately, normal behavior, intact immediate, recent and remote
memories. Visual memory was intact but verbal memory was
disturbed. He couldn’t perform calculations, mainly subtractions and
slightly delayed abstract thinking. Constructional ability is impaired
and has a depressed mood mostly worrying about his illness and was
shy responding only to direct questions.
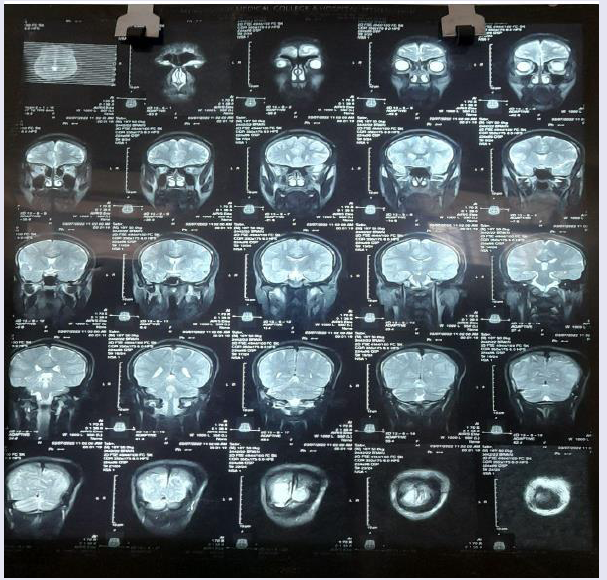
Investigation revealed a tiny subependymal nodule on MRI
of Brain [Figure 5], fundoscopy was normal. Ultrasonography of
the whole abdomen revealed a small focal lesion in the left kidney
[Figure 6]. Other tests like hemoglobin, complete blood count,
renal function test and liver function test were within normal limits.
Electrocardiogram, echocardiogram, chest Xray were also normal.
On the query about, he was born of consanguineous marriage
and uneventful prenatal and postnatal birth history and there
was significant family history. His father also has typical adenoma
sebaceum on his nose [Figure 7A,7B] but gave no history of
having convulsion in his life and is found to be mentally sound. His
mother is leading a normal life. The couple gave birth to 6 children
out of which 3 died in early life due to various causes. Now they
have an elder daughter of 21 years who also has skin manifestation
(adenoma sebaceum) but no other features. The younger daughter is
11 years old and has skin manifestation (adenoma sebaceum) as well
as neurological manifestation ( suffered from convulsions during 1st
year of life and likely to be mentally retarted). As per her father, the
youngest one being 11 years is unable to perform her daily routine on
her own, needs help even for eating and using bathrooms, changing
clothes. She is not able to communicate properly and becomes furious
even with little things and in a new environment. Thus she is not even
attending school. Further evaluation and diagnosis of siblings were
not possible as they were not present in hospital.
Based on the findings of episodes of convulsion with status
epilepticus in between, adenoma sebaceum, ash leaf patterns, shagreen
patch, periungual fibroma, intellectual disability and subependymal
nodules, which fulfilled most of the major criteria of TSC, the patient
was diagnosed to be suffering from Tuberous Sclerosis Complex. Due
to financial constraints and lack of facilities in Bangladesh genetic
study could not be done.
Discussion
Angiofibromas, periungual fibromas (Koenen’stumor), shagreen
patch and leaf macules, fibromatous plaque, and certain other
dermatological manifestations, as well as neurological characteristics
like seizures, mental retardation, and behavioral issues, are some
of the different symptoms of the neurocutaneous disease, tuberous
sclerosis complex.[1] Up to 90% of TSC patients have epilepsy, which
is considered a significant contributor to intellectual disability.[7]
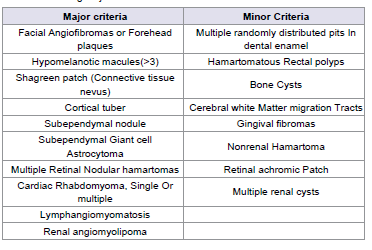
TSC has a specific set of clinical diagnostic criteria as per the
Tuberous Sclerosis Consensus Conference of 1998 and are divided
into major and minor features (Table 1). Presence of either 2 major
features (out of total 11) or one major feature with 2 minor features
(out of total 9) indicated definite TS.[8]
In our patient there are adenoma sebaceum, hypomelanotic
macules, shagreen patch, periungual fibroma and subependymal
nodules fulfilling 5 major criteria of tuberous sclerosis.
Though Tuberous sclerosis is characterized by the development
of unusual tumor growths like hamartoma in brain, skin, retina and
other viscera, Arguably the most important hamartomas are cerebral
ones and these are responsible for the grave neurologic symptoms
and complications. MRI of brain showing tiny subependymal nodule
along with small focal lesion in left kidney in ultrasonography of
abdomen are the positive imaging findings in our case.[8] The 18-yearold
male in this case had neurological and skin manifestations with
a normal chest radiograph and the unremarkable echocardiography
finding. This is not surprising since the cardiac rhabdomyomas are
usually seen in fetuses and neonates and disappear during infancy.[7]
Although tuberous sclerosis complex is a well-known genetic
disorder of autosomal dominant category with high penetrance
and extensive clinical variability.1 Only one-third of the disease is
hereditary, while the rest is due to de novo mutations and are the effects
of parental mosaicism, hence sporadic in nature.[1,2] But significant
family history is reported in our case where the 2 generations seem to
be affected in sequence with variable manifestations. The severity has
been noticed to be more in 2nd generations, mostly the younger siblings.
The father and 1st child had only dermatological manifestations but
the younger children had both dermatological and neurological
manifestations, where neurological manifestations were profound in
the youngest child even leading to behavior problems like intellectual
disability. So further research on the genetic association of TSC in
Bangladesh and its severity as per generations needs to be evaluated
to bring out more accurate statistical information.
While the case presented above is consistent with other published
case reports on TSC, some differences are also noted. For example,
the patient in this case had a family history of TSC, which is not
always present in other cases. Additionally, the patient in this case
had an unusually severe form of TSC, with intellectual disability and
status epilepticus, which may not be present in all cases of TSC.
Prenatal diagnosis is not commonly practiced as no specific
prenatal laboratory test is available but first trimester chorionic villus
sampling and molecular genetic diagnosis is an option if the mutation
in the index case is known.[4,5]
The severity or multiplicity of organ involvement determines
the prognosis of TSC. About a quarter of severely affected infants is
thought to die before the age of 10 years and 75% before 25 years.
However, in the case of individuals diagnosed late in life with few
cutaneous signs, prognosis depends on the associated internal tumors
and cerebral calcifications.[8]
There is no absolute cure for TSC.[4] The management of these
patients includes a multidisciplinary team approach including both
medical and surgical methods. Seizures are treated with antiepileptic
drugs and systemic complications are treated symptomatically.
Surgery, including dermabrasion and laser treatment may be useful
for treatment of skin lesions.
[2] Intervention programs including special schooling and
occupational therapy may benefit individuals with special needs and
developmental concerns. Drug therapy for some of the manifestations
of TSC is currently in the developmental stage. Recent trials have
shown the use of topical 0.1% rapamycin on facial angiofibromas. The
use of inhibitors of mTOR like rapamycin in regression of various
hamartomatous growths is a newer modality in the management⁸ of
TSC.[7]
Patients with TS have a 50% risk of passing on the condition to
each of their offspring although the risk of a severely affected child
is lower.[5,8] Hence genetic counseling should be offered to families
with affected members, even though accurate counseling remains
difficult because of the variability of gene expression.[8] All the
patients diagnosed to have TSC should be evaluated for this by 2-D
Echo, ECG, USG abdomen, cranial CT, and CT of the chest.[4]
TSC has no known cure, but treatment with anticonvulsant
drugs, educational support, and occupational therapy can help
with symptom relief, provide the best quality of life with the fewest
complications from the underlying disease process, least harmful
treatment effects, and require the fewest medications. [8,10]
TSC has a substantial negative impact on the quality of life (QoL)
of patients, affecting psychosocial factors with negative consequences
for education and career along with negative impacts on family, social
and work-related dynamics.[9]Thus early analysis of a child will help
us to control neurological manifestation mainly seizure at early phase
thus reducing risk of neurological impairment, mental retardation,
multiple behavioral problems including sleep disorder, attention
deficit hyperactivity disorder and development of autism spectrum
disorder and hence improving the quality of life of an individual.[8]
Conclusion
As TSC is a lifelong condition, regular surveillance to look for
symptoms and early treatment are associated with better health
and quality of life outcomes for people with TSC. In our case, if the
patient could be diagnosed in early childhood, the severity of Autism
Spectrum Disorder, intensity of epilepsy could be minimized. The
patient could live a near normal life. Moreover, minimal medication
would have been sufficient in that case. Thus, this case report sheds
light to the sheer importance of proper evaluation of a TSC patient
during childhood. As skin manifestation is one of the most common
presentations of this disease, any suspected skin pathology in a child
must be evaluated with paramount concern. In addition, any risk
factor such as positive family history needs to be excluded. From
our findings, we can firmly say, despite the rare association of family
history with TSC in various studies, it is indispensable to evaluate
family history.
Acknowledgements
The authors would like to acknowledge the patient and his
family.
Consent: Written consent was taken from the patient and his father