Journal of Cancer Sciences
Download PDF
Research Article
Markers of Radiogenic Cancer vs. Tumor Progression: an Overview of Chernobyl Studies
Jargin SV*
Department of Pathology, People’s Friendship University of Russia, Russia
*Address for Correspondence: Jargin SV, Department of Pathology, People’s Friendship University of
Russia, Russia, Tel: 7-495 9516788; Email: sjargin@mail.ru
Submission: 14 June, 2021
Accepted: 30 July, 2021
Published: 03 August, 2021
Copyright: © 2021 Jargin SV. This is an open access article distributed
under the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided
the original work is properly cited.
Abstract
Differences in the histological grade of malignancies may reflect
diagnostic quality, that is, averagely earlier or later tumor detection in a
given country. Studies of Chernobyl-related renal-cell carcinoma with
a control from Spain and Colombia are discussed here in comparison
with thyroid cancer research. It is concluded that suppositions
about averagely higher grade and enhanced aggressiveness
of malignancies from the areas previously contaminated by the
Chernobyl fallout are unfounded and can lead to overtreatment.
Results of many studies of Chernobyl-related malignancies are
valuable; but conclusions should be reassessed taking into account
that some cases, classified as aggressive radiogenic cancers, were
in fact late-stage neglected malignancies. Associations of various
markers with the tumor progression can become a field for the future
research and re-interpretation of data obtained in studies comparing
malignancies from different countries. Some markers may reflect
efficiency of healthcare services.
Abbreviations
RCC: renal-cell carcinoma; TC: thyroid cancer; PTC: papillary
thyroid carcinoma; VEGF: vascular endothelial growth factor; SU:
Soviet Union; CA, Chernobyl accident; mSv: millisievert; mGy:
milligray; UNSCEAR: United Nations Scientific Committee on the
Effects of Atomic Radiation; NF: nuclear factor; RET: rearranged
during transfection; PTC: papillary thyroid carcinoma; TGF:
transforming growth factor; IAEA: International Atomic Energy
Agency; NHEJ: тon-homologous end-joining.
Introduction
A tendency to overestimate health risks from low doses of
ionizing radiation has been discussed previously [1,2]. Apparently,
certain scientists exaggerating medical and ecological consequences
of the anthropogenic increase in the radiation background contribute
to a strangulation of the atomic energy, which would agree with the
interests of fossil fuel producers. Nuclear power has returned to
the agenda because of the concerns about increasing global energy
demand and climate changes. Health burdens are greatest for power
stations based on coal and oil. The burdens are smaller for natural gas
and still lower for nuclear power. The same ranking applies also to the
greenhouse gas emissions and thus probably to climate changes [3].
Studies of Chernobyl-related clear-cell renal-cell carcinoma
(RCC) with a control from other countries are discussed here in
comparison with thyroid cancer (TC). The series of studies [4-10], in
particular, the last study [10], compared RCC tissue specimens from
Ukraine (including the area of Chernobyl contamination) with those
from Spain and Colombia. In brief, RCCs from Ukraine tended to be
less differentiated than the overseas controls [4-10]. In the last study, the microvessel density in the RCC tissue from patients residing
both in “highly” and in “low contaminated areas of Ukraine” was
considerably higher than in RCC from Spain and Colombia (p<0.01).
The difference between both Ukrainian groups was statistically
insignificant. The increased level of angiogenesis was associated with
a higher expression of the immunohistochemical marker VEGF [10].
It has been assumed that the radiation exposure leads to an increase
in the microvessel density, which in turn is associated with a lower
level of differentiation (higher grade) and less favorable prognosis of
RCC [9,10,11].
It was pointed out in the preceding comment that the difference
in the RCC grade between Spain and Ukraine can be explained
by a more efficient and early cancer diagnostics in Spain [12]. The
proposed increase in the “aggressivity” of both RCC and TC after the
radioactive contamination in the Chernobyl area [4,13] apparently
resulted from detection by the screening of old neglected malignancies,
interpreted as radiogenic tumors with the “rapid onset and aggressive
development” [13]. The screening detected not only small nodules
but also advanced TCs, neglected because of the incomplete coverage
of the population by medical checkups prior to CA. This predictable
phenomenon was confirmed by the fact that the “first wave” TCs after
CA were on average larger and higher-grade than those diagnosed
later [14] because neglected cancers were gradually sorted out by the
screening. The hypothesis presented here is that radiation exposure
as a cause of differences between “exposed” and control groups from
abroad is improbable. As previously discussed in regard to TC, the
differences are caused at least in part by the averagely later cancer
diagnostics in the former Soviet Union (SU) [1]
Dose Comparisons
Individual effective doses from the natural background radiation
are generally expected to range from 1.0 to 10 mSv/year; some national
averages exceed 10 mSv/year [15,16]. The average for the Russian
Federation is 3.35 mSv/year; the highest background among federal
subjects is in the Altai Republic - 8.83 mSv/year [17]. The average
individual whole body dose to 6 million inhabitants of the territories,
recognized as contaminated by the Chernobyl fallout, received from
1986 through 2005, was ~9 mSv [18]. For comparison, according to
assessments of data on solid cancers and leukemia among survivors
of atomic explosions in Japan, there was a significant positive dose
response correlation among all survivors who received <500 mSv but the statistical significance vanished if only doses <200 mSv
were considered[19,20]. Doses <100 mGy at low rates may induce
adaptive response against neoplastic transformation [21]. Annual
average doses from natural radiation should be specified in papers
where cohorts from different geographical regions are compared;
otherwise doses among controls may turn out to be not significantly
different from those in the “exposed” cohort e.g. in patients from
Spain vs. those from Kiev [6,8]. The average annual individual dose
from the background radiation in Spain is ~5 mSv [22,23]. According
to an estimate, the mean whole-body individual dose to inhabitants of
Kiev from all sources was ≤10 mSv in 1986, decreasing thereafter [1].
No dose estimates were given in the articles [4-10]; it is only written
with a self-reference: “This observation also supports the prevailing
suspicion [9] that in Ukraine the radiation contamination levels were
similar within and beyond the officially-established 80-km extent of
radiation contamination around Chernobyl [1]” [10]. The source
[25], a Ministry report, has been unavailable.
Radiation Effects vs. Late Detection
The Chernobyl accident (CA) provides an example of considerable
difference in diagnostic quality before and after the accident. There
has been no convincing evidence of cause-effect relationships between
radiation exposures from CA and the incidence increase of cancers in
residents of contaminated territories other than TC in people exposed
at a young age [18]. TC and probably also other cancers were underreported
before CA. Mechanisms of the registered TC incidence
increase included the screening and improved medical surveillance
after CA [18]. According to the UNSCEAR, “the background rate of
thyroid cancer among children under the age 10 was approximately
two to four cases per million per year” [26]. The UNSCEAR 2008
Report compared the enhanced TC incidence rates 4 years after the
accident and later not with the pre-accident level but with the years
1986-1990 (Annex D, pp. 60-61), when the incidence had increased
up to 4.1 cases per million per year in people exposed at the age of
<10 years and up to 5.4 - in those exposed at <18 years [18]. The
period 1986-1990 was chosen for comparison because “since 1986
and not earlier, specific data on thyroid cancer incidence have been
specifically collected by local oncologists” (UNSCEAR Secretariat,
e-mail communication of 22 October 2013). According to another
source, the incidence of TC among people younger than 15 years in
the North of Ukraine (overlapping with the contaminated area) was
0.1 and in Belarus - 0.3 cases/million/year from 1981 through 1985
[27]; more details are in [28]. Only 5 children were diagnosed with
thyroid malignancies in Belarus during the period 1978-1985, the
detection rate of pediatric TC prior to CA being lower than that in
other developed parts of the world [29]. This indicates that there were
undiagnosed cases in the population. The underreporting tendency
is known also for renal malignancies[30]. Some neglected cancers,
detected by the screening, self-reported in conditions of increased
public awareness after CA, or brought from other areas and registered
as Chernobyl victims, were misinterpreted as rapidly growing
radiogenic malignancies[1]. Many people wanted to be recognized
as Chernobyl victims to gain access to health care provisions and
compensations [31]. Cases from non-contaminated areas must have
been averagely more advanced as there was no extensive screening
Renal cell carcinoma (RCC):
By analogy with TC, the registered incidence rise of RCC in
Ukraine following CA [4,7,9,10]was probably caused by improved
diagnostics [12]. As mentioned above, RCCs from Ukraine tended
to be less differentiated than those from Spain. RCCs from Ukraine
showed sarcomatoid i.e. poorly differentiated pattern more
frequently: 62 from 236 (26.3 %) of Ukrainian vs. 11 from 112 (9.8
%) of Spanish cases (p<0.001) [1]; the significant difference was
confirmed by the subsequent study [7]. Apparently, the difference was
caused by the more efficient and early cancer diagnostics in Spain. In
this connection, the following citations should be commented: “The
dramatic increase of aggressivity and proliferative activity” was found
in RCC from Ukraine, while “the majority of the high grade tumors
occurred in the Ukrainian (rather than in the Spanish) groups” [4].
These differences can be attributed to a more efficient and early
cancer diagnostics in Western Europe and, conversely, detection by
the screening of advanced cases in Ukraine. The misinterpretation of
such cases as aggressive radiogenic cancers has been conductive to an
overtreatment (discussed below).Some molecular-genetic characteristics of RCC from Ukraine
vs. those from Spain and Colombia need a re-interpretation e.g.
the absence of significant differences in the expression of ubiquitin
[8]. Considering that RCCs from Ukraine were averagely more
advanced than Spanish cases, these data indicate that ubiquitin is
not associated with the progression of RCC. In contrast, VEGF was
found more frequently in clear-cell RCC from Ukraine than in the
specimens from Spain and Colombia [10]. The statement that “in
RCC the level of serum VEGF has been shown to be closely related
to tumor stage and grade of RCC, and the expression of VEGF to
be significantly associated with tumor stage” [10] was confirmed by
the reference [11]. Other studies also reported associations between
VEGF expression and microvascular density, nuclear grade, tumor
size, stage, and prognosis of RCC [32-35]. The study under discussion
also “demonstrated a close relationship between VEGF expression
and the stage of clear-cell RCC” [11]. The same considerations
probably pertain to other markers, where substantial differences were
found between the Spanish and Ukrainian RCCs, in particular, the
transcriptional nuclear factor kappa B (NF-kappa-B), its p50 and
especially p65 subunits [7]. The >10% cell positivity for p50 was
found in 25 from 59 (42.4 %) of specimens from Ukrainian vs. 4
from 19 (21.1 %) of Spanish patients; the >50% p65 positivity was
found, correspondingly, in 18 from 59 (30.1 %) vs. 1 from 19 (5.3 %)
of the specimens (p<0.05) [7]. NF-kappa-B activation is discussed in
the literature as a potential biomarker and promoter of the cancer
progression [36-41].
Papillary thyroid carcinoma (PTC):
For interpretation of the above data, the analogy with RET/PTC3
chromosomal rearrangements in PTC is helpful. The RET/PTC3
fusions apparently correlate with the progression of PTC and hence
with the disease duration [42]. An association was found between the
RET/PTC3 expression and aggressive phenotype, advanced stage and
larger size of PTC [43]. With the time passing after CA, the prevalence
of RET/PTC3 declined [44,45] while advanced neglected TCs were
sorted out by the screening. The cohort of post-Chernobyl pediatric
PTC, with RET/PTC3 being the most prevalent RET rearrangement type, was supposed to be worldwide exceptional [46]. In fact, the cohort has been unique not globally but for industrialized highincome
countries where cancer is diagnosed relatively early. Similarly
to Chernobyl, RET/PTC3 was the most prevalent RET rearrangement
in the studies from India [47,48]. Asian populations generally
demonstrated a higher positive rate for RET/PTC3 compared to
Western populations (26.50% vs. 17.05%) [49]. Of note, in Japan
the frequency of RET/PTC3 is relatively low [49,50]. Pediatric TC in
Japan has been different from that after CA, showing less frequently
the poorly differentiated solid and solid-trabecular patterns
[51,52]. International comparisons of TC size and stage may be less
meaningful than those of differentiation grade because large nodules
with uncertain malignant potential can be classified as high-stage
cancers if there is a propensity to histological over-diagnosis, while
screening activities may be a confounding factor. Unlike Chernobyl,
most TCs after the Fukushima accident were of the classical papillary
i.e. higher differentiated type [53,54], which suggests the averagely
earlier tumor detection in such developed country as Japan. Along
the same lines, RET/PTC3 are rare in France [55]. Mutations were
found in TC from Russia more frequently compared to the United
States [56,57], which indicates earlier diagnostics in the latter country.Another recent example is the study making a comparison between
359 PTCs from patients who underwent radiation exposure from CA
and the control group - TCs from 81 patients born >9 months after
CA [58]. The “study population included a substantial number of
PTCs occurring after <100 mGy,” where development of radiogenic
cancer would be improbable as per dose comparisons presented
above. The study reported “…radiation dose-related increases in
DNA double-strand breaks in human TCs developing after the CA…
Non-homologous end-joining (NHEJ) the most important repair
mechanism… increased likelihood of fusion versus point mutation
drivers” [58]. These findings are not surprising: DNA damage tends
to accumulate along with the tumor progression. Double-strand
breaks with error-prone repair contribute to the genome diversity in
cancer cells [59]. The NHEJ repair pathway is potentially mutagenic
[60]. Some aberrant gene fusions drive the tumor progression
[61]. At the same time, no association of the radiation exposure
with transcriptomic and epigenomic features was found [58]. This
indicates that the latter markers are to a lesser extent associated with
the neoplastic progression than the DNA lesions. As for individuals
born after CA (the control group in [58]), the data pertaining to
them originated from a later period, when the quality of diagnostics
improved while the reservoir of advanced neglected cancers was partly
exhausted by the screening. Therefore, the average stage and grade of
TCs in the exposed group must have been a priori higher than among
the controls in [58]. The causative role of low-dose radiation e.g. “a
dose-dependent carcinogenic effect of radiation derived primarily
from DNA double-strand breaks” in the studied population [58] is
unproven. Finally, the “…increased detection of pre-existing PTCs in
the population that may not become clinically evident until later, if at
all, due to intensive screening and heightened awareness of thyroid
cancer risk in Ukraine” [58] should be commented. This concept has
been formulated in several publications since 2011 [1,2,32-66] that
have not been cited in [58]. The study [58] is well-designed; but the
authors should think about a re-interpretation of their results. Other
studies of molecular-genetic features of Chernobyl-related cancers
have been commented previously [65,66].
Overtreatment of Chernobyl-Related Lesions
Renal cell carcinoma (RCC):
The concept of enhanced aggressiveness of post-Chernobyl RCC
can have unfavorable consequences if surgeons get the message that
cancers from radio-contaminated areas tend to be more aggressive
than usual, while surrounding renal tissues harbor “proliferative
atypical nephropathy with tubular epithelial nuclear atypia and
carcinoma in situ”[5]. Based on this premise, some surgeons might
decide to perform nephrectomy more often than clinically indicated
instead of a kidney-preserving procedure.Thyroid cancer (TC):
The misclassification of neglected advanced cases as aggressive
radiogenic cancers has given rise to the concept that supposedly
radiogenic TCs, at least those from the “first wave” after CA,
were more aggressive than sporadic ones [14,67-69]. This had
consequences for the practice: the surgical treatment of radiogenic
TC was recommended to be “more radical” [70]. After 1998-1999,
the thyroid surgery in some institutions of the former SU, Belarus
in particular, adopted more radical approaches. The following
was recommended for Chernobyl-related pediatric TC: “Radical
thyroid surgery including total thyroidectomy combined with neck
dissection followed by radioiodine ablation” [29] and/or high-dose
external radiotherapy (40 Gy) [72]. Some experts regarded subtotal
thyroidectomy to be “oncologically not justified” and advocated total
thyroidectomy with prophylactic neck dissection [70,73-75]. More
limited resections were regarded to be “only acceptable in exceptional
cases of very small solitary intrathyroidal carcinomas without
evidence of neck lymph node involvement on surgical revision” [71].
It was stipulated in a recent instructive publication that a bilateral
neck dissection must be performed in all TC cases independently of
the tumor size, histology and lymph node status [76]. This approach
is at variance with a more conservative treatment of TC applied
internationally. The articles [77,78] were misquoted in the paper [73]
advocating total thyroidectomy with bilateral neck dissection for all
types of pediatric TC. The articles [79-81] were cited in support of the
statement: “The most prevailing opinion calls for total thyroidectomy
regardless of tumor size and histopathology” [71]. In fact, subtotal
thyroidectomy was used or recommended in these studies, in some
of them in parallel with total thyroidectomy [79-81]. The total
thyroidectomy with neck dissection is known to be associated with
complications e.g. hypoparathyroidism and recurrent laryngeal
nerve palsy. Moreover, a large part of post-Chernobyl thyroid
patients were young females potentially concerned about cosmetic
aspects. The overall survival rate was very high in adolescents and
young adults with differentiated TCs regardless of the extent of the
surgery [82], which indicates that the radicalism had sometimes been
superfluous. Similar surgical tactics were applied to TC patients from
the East Urals Radioactive Trace [83]. The relatively high suicide rate
noticed among patients with Chernobyl-related TC [84,85] can be
explained by a decreased quality of life after the excessively radical
surgery. Epidemiologists warned against the over-diagnosis and
overtreatment of patients with indolent thyroid tumors. It is essential
to exclude adenoma and borderline/precursor tumors because they
can be treated with simple excision or less extensive resections [86].
Relevant considerations about TC over-diagnosis and overtreatmenthave been phrased in the recent review: “After the Chernobyl
and Fukushima nuclear accidents, thyroid cancer screening was
implemented mainly for children, leading to case over-diagnosis;”
“The existence of a natural reservoir of latent thyroid carcinomas,
together with advancements in diagnostic practices leading to case
over-diagnosis explain, at least partially, the rise in TC incidence
in many countries;” “Total thyroidectomy, as performed after the
Chernobyl accident, implies patients must live the rest of their lives
with thyroid hormone supplementation. Additional treatment using
radioactive iodine-131 therapy in some cases may result in potentially
short- or long-term adverse effects” [87] without citing preceding
publications expressing the same ideas [1,2,66,88,89].
Potential mechanisms of TC false-positivity after CA have been
discussed in detail previously; among others, the misinterpretation of
nuclear pleomorphism as a malignancy criterion of thyroid nodules
[89]. Potentially misleading histological images from Russianlanguage
handbooks were reproduced and commented [64,90,91].
The post-Chernobyl radiophobia contributed to the over-diagnosis
of cancer, which can be illustrated by the following citation (from
Russian): “Practically all nodular thyroid lesions, independently
of their size, were regarded at that time in children as potentially
malignant tumors, requiring an urgent surgical operation” [92].
Ultrasound devices were introduced into practice earlier than fineneedle
biopsy [92], which probably contributed to the false-positivity
in the 1990s. The iodine deficiency on the contaminated territories
and goiter associated with it was a contributing factor because more
thyroid abnormalities were found by the screening, providing more
opportunities for the over-diagnosis of malignancy. The articles
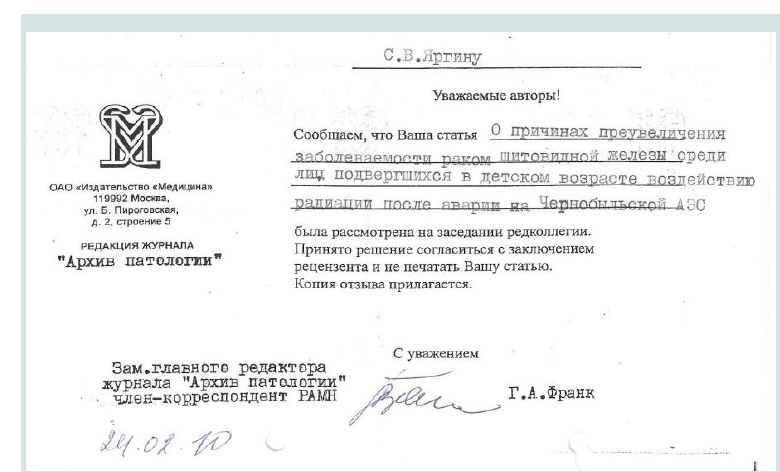
describing mechanisms of the false-positivity, possibly operative until
today, have been rejected by the main journal of Russian pathologists
Arkhiv Patologii (Archives of Pathology) despite personal
communications with the editor-in-chief Georgii Frank (Figure 1).
As a result, the articles about the over-diagnosis and overtreatment of
Chernobyl-related lesions have been published abroad and later also
in Russian journals that are rarely read by pathologists [93].
Urinary bladder lesions:
The over-diagnosis and potential overtreatment of post-Chernobyl
urinary bladder lesions was discussed previously [94]. The same
researchers, who participated in the RCC research discussed above
[4-10], found by means of cystoscopy and bladder biopsy in different groups of patients with benign prostatic hyperplasia and females with
chronic cystitis, from contaminated areas and Kiev, severe urothelial
dysplasia or carcinoma in situ in 56-96 % of all randomly selected
(consecutive) cases [95-100]. These percentages are unrealistic and
indicative of the false-positivity. The microphotographs from [95,96]
were reproduced in [94]: the sections are visibly thick, many nuclei
are poorly stained. Neither cancer nor severe dysplasia is recognizable
in the illustrations. The poor quality of specimens could have been
additionally caused by inadequate fixation, processing-related factors
and/or electrocoagulation. The over-diagnosis must have entailed overmanipulation
and overtreatment. Apparently, “Chernobyl cystitis” or
“irradiation cystitis” reiterated in [96,100], reportedly characterized
by the “reactive epithelial proliferation associated with hemorrhage,
fibrin deposits, fibrinoid vascular changes, and multinuclear stromal
cells” [100], was at least in part caused or maintained by repeated
cystoscopies with “mapping” biopsies, electrocoagulation etc.
Accordingly, some of the immunohistochemical and moleculargenetic
markers, especially those associated with the tissue alteration,
inflammation and cell proliferation (mitogen-activated protein
kinases, growth factors, TGF-β1, NF-κB, p38) as well as the “marked
activation of angiogenesis in urinary bladder lamina propria” [96],
discussed within the scope of the radiation-related carcinogenesis [96],
reflected chronic inflammation and increased cellular proliferation
unrelated to ionizing radiation and partly iatrogenic. Scrutinizing the
figures from [101,102] (reproduced in [94], it seems that the overdiagnosis
of malignant and premalignant bladder lesions by the same
experts occurred also earlier in the 1980s potentially leading to an
overtreatment. It is known that excessive screening for cancer and
precancerous lesions can lead to an over-diagnosis [87], especially if
diagnostic facilities are not perfect.Conclusions and Future Research
By analogy with RET/PTC3, there may be a correlation between
the tumor progression and those markers of RCC, where differences
between the Ukrainian and Spanish cohorts were found. In particular,
the higher microvessel density and VEGF expression in the Ukrainian
specimens vs. those from Spain and Colombia [10] can be explained
by averagely earlier cancer diagnostics and hence better functioning
health services in both latter countries compared to the former SU.
Associations of various markers with the tumor progression (disease
duration, tumor size, stage and grade, metastases etc.) is a potential
field for the future research and re-interpretation of the data already
obtained in studies comparing malignancies from different parts of
the world. Some markers may characterize efficiency of healthcare
services.
The medical surveillance of populations exposed to low-dose
ionizing radiation is important; but more consideration should
be given to potential bias e.g. screening effect, dose-dependent
selection and self-selection. Well-conducted epidemiological studies
can account for some bias, which has not always been the case in
the Chernobyl-related research [62,63]. In the author’s opinion,
epidemiological studies of populations exposed to the Chernobyl
fallout would hardly add much reliable information, among others,
because of inexact dose reconstructions and registration of unexposed
individuals as exposed. As mentioned above, some people wanted
provisions and compensations[31]. “Uncertainties in radiation dose
estimates” were acknowledged e.g. in the article discussed above [58].
Indeed, “doses were estimated using detailed information derived
from individual direct thyroid radioactivity measurements taken
within 8 weeks of the accident” [58], whereas the half-life of[131]
I is ~8 days. Furthermore, dose-effect correlations can be explained
by a recall bias: it is known that cancer patients tend to recollect
circumstances related to radiation better than healthy people [103].
It can be reasonably assumed that patients with advanced cancers
would recollect such circumstances better than practically healthy
individuals with small nodules. The higher the average dose estimate,
the greater would be the probability to undergo screening. Therefore,
even in the absence of the causative role of radiation, certain features
associated with post-Chernobyl cancer would be more prevalent in
populations with higher dose estimates and/or residing on more
contaminated territories. One of such features is the relatively high
percentage of advanced neglected cancers detected by the screening
after CA and misinterpreted as aggressive radiogenic malignancies
[1,63,64]. The following citation is insightful: “The tumors were
randomly selected (successive cases) from the laboratories of Kiev and
Valencia...The tumors were clearly more aggressive in the Ukrainian
population in comparison with the Valencian cases” [104] The
explanation is not far to seek: the more efficient and early diagnostics
in Valencia. Considering the above argumentation and the data from
the study [10], the same is probably true for Barranquilla (Colombia).
It can be reasonably assumed that the screening effect and
increased attention of exposed people to their own health will result
in new reports on the elevated cancer and other health risks in the
areas with enhanced natural or anthropogenic radiation background.
A promising approach to the study of dose-response relationships
are lifelong animal experiments. The life duration is known to be a
sensitive endpoint attributable to radiation exposures [105], which
can reveal the net harm or potential benefit (within a certain range
according to the concept of hormesis [106]) from low-dose exposures