Journal of Emergency Medicine & Critical Care
Download PDF
Copyright: © 2017 Fernandez AB, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Short Commentary
High Flow Nasal Cannula Oxygen Therapy for Acute Pulmonary Oedema Post-Cesarean Sectionin Severe Preeclampsia
Ana Belen Fernandez* and Amelia Gonzalez
- Department of Anesthesiology, Hospital Universitario Nuestra Señora de Candelaria, Spain
Address for Correspondence: Ana Belen Fernandez, Department of Anesthesiology, Intensive Care and Pain Treatment, Nuestra Sra de Candelaria University Hospital, Carretera del Rosario nº 115. C.P. 38010 Tenerife Canary Island, Spain, Tel: 0034 922019154; E-mail: anabfp@gmail.com
Citation: Fernandez AB, Gonzalez A. High Flow Nasal Cannula Oxygen Therapy for Acute Pulmonary Oedema Post- Cesarean Section in Severe Preeclampsia. 2017;3(1): 2
Journal of Emergency Medicine & Critical Care | ISSN: 2469-4045 | Volume: 3, Issue: 1
Submission: 03 October, 2017| Accepted: 16 October, 2017 | Published: 24 October, 2017
Submission: 03 October, 2017| Accepted: 16 October, 2017 | Published: 24 October, 2017
Acute dyspnea with accompanying hypoxemia in post-surgical patients is a major problem in the intensive care unit. A oxygen therapy is an essential supportive treatment to correct these issues. High-Flow nasal cannula (HFNC) oxygen therapy has been an innovative and effective alternative respiratory support for critically ill patients, because of its physiological advantages compared with other standard oxygen therapies [1]. However evidence is uneven because the reports cover various subjects with diverse underlying conditions. Even so, across the diversity, many published reports suggest that HFNC decreases breathing frequency and work of breathing and reduces the need for respiratory support escalation [2]. Carlucci A et al. (2001) determined in their study with respect to non-invasive ventilation (NIV): “poor tolerance is a risk factor of NIV failure” [3]. Despite the fact that NIV can produce significant clinical improvement, patients often reject it or fail to use it appropriately. Correctly use of NIV is crucial, given that adherence to medication decreases over time and is inversely related to the number of drugs prescribed. Clinical experience suggests that patients with psychological alterations, such as anxiety and depression are less likely to accept and comply with NIV regimes [4]. Pre- and post-surgical stress and the obstetric patient because of their particular conditions clearly influence the rejection of NIV. According to the most recent literature, there is only one case of use of non-invasive ventilation in a critically ill obstetric patient with non-cardiogenic pulmonary oedema (during cesarean and later ICU) and good tolerance [5].
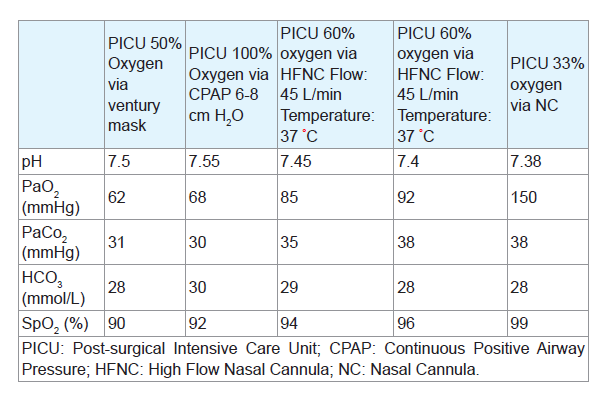
A 33-year-old primigravid woman was referred to our clinic with severe preeclampsia at 28 weeks of gestation. She has a clinical history of asthma in childhood, currently asymptomatic. During her stay in hospital she develops hypertension with difficult control, proteinuria, ascites and mild orthopnea. On post-admission day 10, a cesarean section was indicated under general anesthesia for severe preeclampsia and HELLP syndrome. The surgery is successful and the patient is transferred to the Post-surgical Intensive Care Unit (PICU) in spontaneous ventilation with adequate oxygen saturation. Blood transfusion is not performed.
12 hours later the patient began with increased dyspnea and accessory muscle use. Pulse oximetry reading was 90% despite oxygen 15 L/min by face mask. Arterial blood gas analysis showed pO2 59 mmHg, pCO2 25, HCO3 23 and pH 7.52. Chest auscultation revealed bilateral crackles and decreased breath sounds and chest X-ray showed a bilateral “butterfly like” alveolar pattern with bilateral pleural effusion. Lung ultrasound showed bilateral B-lines with normal echocardiography. We started medical treatment with diuretics, morphine and clevidipine intravenous infusion at 4-8 mg/hr. A right pleural drainage tube was placed. Boussignac Continuous Positive Airway Pressure (CPAP) system with an inspired oxygen concentration (FiO2) 0.6-0.8 and 7-9 cm H2O was applied. Despite treatment with sedative drugs the patient begins with anxiety, intense psychomotor agitation, profuse sweating and sinus tachycardia (HR 140 beats/min) rejecting therapy. After an adequate psychological approach to explain to the patient the need for oxygen therapy and to participate in its improvement, we started to HFNC 45 L/ min FiO2 60% and 37 °C for 4 hours per shift/24H, and O2 nasal cannula 5 L/M. Patient improved over the next 36 hours with arterial pO2 120-140, pCO2 40 and pH 7.45. Sedative drugs were withdrawn. The patient was discharged to the Obstetric Department to complete her recovery on the 4th post-cesarean section day.
HFNC is a new device that deliver totally conditioned gas (37 °C containing 44 mg H2O/L (100% relative humidity) using a heated humidifier and a heated inspiratory circuit) through a wide bore nasal cannula at very high flow (up to 60 L/min) at a predetermined constant oxygen concentration (21 to 100%). The continuous insuflation of a high-flow gas mixture facilitates oxygenation and CO2 clearance through gaseous mixing. HFNC is a non-invasive respiratory support that does not increase dead space, with an oxygen mask, especially at low flow, CO2 is rebreathed. NIV interfaces also increase dead space, and volume is added by hood-type CPAP system. This device can provide some PEEP (5-7 cm H2O and mouth closed) that may help to improve oxygenation and counteract the effects of intrinsic PEEP on work of breathing and that may act by washing out oropharyngeal dead space. It may also help to reduce inspiratory resistance and facilitate secretions clearance from humidified gas. A touted advantage is comfort, probably a result of the combination of the physical characteristics of the device, and a reduction in desiccation commonly associated with the cold, dry air flow of conventional oxygen therapy [6-10].
At the moment, we cannot speak of absolute indications for HFNC, nor defined criteria to starting, stopping nor indications for treatment escalation. It seems certain that according to recent scientific reviews, HFNC is a useful and effective non-invasive ventilation modality that providing a greater degree of comfort and better adaptation to ventilation, which is crucial for critical patients and with diverse underlying diseases. The patient obstetrical and critical post-surgical patients have a high level of stress that can lead to situations of extreme anxiety, fear and psychomotor agitation with poor adherence and collaboration with treatments, especially non-invasive ventilation with facial mask, worsening if there is also a major acute respiratory failure.
In our opinion, it´s necessary psychological support teaching these patients to manage stress to minimize their negative effects and to be an active part in the recovery of their functions: proper respiration and oxygenation, decrease the level of catecholamines for adequate tissue and organ perfusion...and who knows if we will be able to avoid endotracheal intubation due to failure of respiratory support in the year 2020.
References
- Rittayamai N, Tscheikuna J, Praphruetkit N, Kijpinyochai S (2015) Use of high-flow nasal cannula for acute dyspnea and hypoxemia in the emergency department. Respir Care 60: 1377-1382.
- Nishimura M (2016) High-flow nasal cannula oxygen therapy in adults: physiological benefits, indication, clinical benefits, and adverse effects. Respir Care 61: 529-541.
- Carlucci A, Richard JC, Wysocki M, Lepage E, Brochard L, et al. (2001) Noninvasive versus conventional mechanical ventilation. An epidemiologic survey. Am J Respir Crit Care Med 163: 874-880.
- Volpato E, Banfi P, Pagnini F (2017) A psychological intervention to promote acceptance and adherence to non-invasive ventilation in people with chronic obstructive pulmonary disease: study protocol of a randomised controlled trial. Trials 18: 59.
- Fernández A, Dominguez D, Delgado L (2011) Severe non-cardiogenic pulmonary oedema secondary to atosiban and steroids. Int J Obstet Anesth 20: 189-190.
- Carratalá JM, Llorens P, Brouzet B, Albert Jiménez AR, Fernández-Cañadas JM, et al. (2011) High-flow therapy via nasal cannula in acute heart failure. Rev Esp Cardiol 64: 723-725.
- Hernández G, Roca O, Colinas L (2017) High-flow nasal cannula support therapy: new insights and improving performance. Crit Care 21: 62.
- Frat J-P, Thrille AW, Mercat A, Girault C, Ragot S, et al. (2015) High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med 372: 2185-2196.
- Mauri T, Turrini C, Eronia N, Graselli G, Volta CA, et al. (2016) Physiologic effects of high-flow nasal cannula in acute hypoxemic respiratory failure. Am J Respir Crit Care Med 195: 1207-1215.
- Lee CC, Mankodi D, Shaharyar S, Ravindranathan S, Danekers M, et al. (2016) High flow nasal cannula versus conventional oxygen therapy and non-invasive ventilation in adults with acute hypoxemic respiratory failure: a systematic review. Respir Med 121: 100-108.