Journal of Geriatrics and Palliative Care
Download PDF
Review Article
*Address for Correspondence: Huai Cheng, Division of General Medicine, Geriatrics, andPalliative Care, Department of Medicine, University of Virginia, PO Box 800901, Charlottesville, VA 22981, USA, Tel: 434-924-1685; Fax: 434-977-0581; E-mail: hyc9j@hscmail.mcc.virginia.edu
Citation: Cheng H, Haight T. Prescribing Antidepressants in Depressed Nursing Homes Residents with Dementia: Is it Evidence-based? J Geriatrics Palliative Care 2013;1(1): 5.
Copyright © 2013 Cheng et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.Journal of Geriatrics and Palliative Care | ISSN 2373-1133 | Volume: 1, Issue: 1
Prescribing Antidepressants in Depressed Nursing Homes Residents with Dementia: Is it Evidence-based?
Huai Cheng* and Taylor Haight
- Division of General Medicine, Geriatrics, and Palliative Care,Department of Medicine, University of Virginia, USA
*Address for Correspondence: Huai Cheng, Division of General Medicine, Geriatrics, andPalliative Care, Department of Medicine, University of Virginia, PO Box 800901, Charlottesville, VA 22981, USA, Tel: 434-924-1685; Fax: 434-977-0581; E-mail: hyc9j@hscmail.mcc.virginia.edu
Citation: Cheng H, Haight T. Prescribing Antidepressants in Depressed Nursing Homes Residents with Dementia: Is it Evidence-based? J Geriatrics Palliative Care 2013;1(1): 5.
Copyright © 2013 Cheng et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.Journal of Geriatrics and Palliative Care | ISSN 2373-1133 | Volume: 1, Issue: 1
Abstract
Depression and dementia are common comorbidities among Nursing Home (NH) residents. Antidepressants are widely used in this vulnerable population. However, the evidence for anti-depressant use, including from randomized controlled trials, systematic reviews, and evidence-based clinical practice guidelines, is inconsistent and conflicting. Additionally, antidepressants are associated with multiple adverse effects. Long-term care providers often need to deal with requests from patients’ families, nursing staff, and colleagues to prescribe antidepressants, while following recommendations from pharmacists and regulations from the Center for Medicare and Medicaid Service (CMS) and Federal Drug Administration (FDA) not to prescribe or to discontinue antidepressants. It is difficult for long-term care providers to decide whether they should prescribe antidepressants and meet regulations and quality of care standards based on the few Randomized Controlled Trials (RCTs). A large randomized control study to examine the efficacy of antidepressants among depressed NH residents with dementia is urgently needed. We propose a practical step-wise approach to prescribe antidepressants for this vulnerable population.Keywords
Depression; Dementia; Antidepressant; Nursing homeAbbreviations
AD: Alzheimer’s Disease; CMS: Center for Medicare and Medicaid Service; CSDD: the Cornell Scale for Depression in Dementia; DSM: Diagnostic and Statistical Manual of Mental Disorders; FDA: Federal Drug Administration; NH: Nursing Home; RCT: Randomized Controlled TrialIntroduction
Long-term care providers often see the following scenario at NH. This is a patient, Ms. Smith, is 85 years old. She is on multiple medications for her hypertension, diabetes mellitus, arthritis, urinary incontinence, constipation, cataract, and insomnia. She often requires assistance from nursing staff for medication administration as well as her activities of daily living such as bathing and toileting. She was diagnosed with advanced dementia several years ago. She is only oriented to person. However, she follows simple commend slowly. She looks sad, anxious, and is sometimes tearful. The nursing staff also notices that she has significant apathy and tires easily. At night, she wanders and often needs medication to sleep. Due to her poor appetite, she has lost 10 pounds within the last 6 months. Additionally, Ms. Smith is easily annoyed and agitated. Sometimes she yells, curses, and hits the nursing staff. Based on the above observation and brief assessment for depression, both the nursing staff and I agree that that Ms. Smith has depression. The nursing staff suggests prescription of an antidepressant and antipsychotics as well (which would be another topic) for this patient. The patient’s family also thinks she is depressed and asks whether I could prescribe an antidepressant to improve her depression and quality of life. Because the FDA and CMS have strict regulations on antidepressants [1,2], the pharmacist often asks me to reduce the dose of antidepressants or discontinue antidepressants as a result of regularly scheduled patient medication reviews. This is a challenging situation which I am sure other providers experience as well. The goal of this minireview is to promote the use of evidence-based practice guidelines in prescribing antidepressants for this vulnerable geriatric population. In this review, we examine the therapeutic evidence for prescribing antidepressants in this population using randomized controlled trials (RCTs), systematic reviews, and evidence-based clinical practice guidelines. The potential adverse effects of antidepressants will be briefly reviewed. Finally, we propose a practical step-wise approach to prescribing antidepressants for depressed NH residents with dementia.Evidence of Antidepressants to Treat Depression in Depressed NH Residents with Dementia
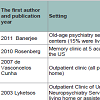
Depression and dementia are common and often co-exist in older NH residents [3-8]. For example, a recent study based on 2,564,687 participants in the MDS (Minimum Data Set) among 5,445 U.S. facilities showed that as many as 50% NH residents with dementia had major depression or depressive symptoms [7]. Depression is associated with impaired physical function, poor quality of life, suffering, disability, increased mortality and health care utilization [3,9,10], and increased use of psychotropic drugs such as antidepressants [5,6,8]. One recent study found that the use of antidepressants for depressed NH residents with dementia significantly increased from 69% in 1999 to 81% in 2007 [7]. Perhaps, this widely use of anti-depressants is because general reviews [3,11-20] and guidelines [21-24] recommend that antidepressants are effective to treat depression in NH residents with dementia. However, the evidence of effectiveness of antidepressants in this vulnerable population is inconsistent and conflicting. First, no systematic review focuses on the use of antidepressants to treat depression in depressed NH residents with dementia based on our recent preliminary search of PubMed and Cochrane reviews; Second, four systematic reviews [9,25-27] on the use of antidepressant were not specific to depressed NH residents with dementia. For example, one systematic review included depressed NH patients with or without dementia [25]. Other three systematic reviews included depressed patients with dementia at NH and non-NH setting [9,26,27]. Two systematic reviews suggested a modest effect of antidepressants on depressed older adults with dementia [9,25]. In contrast, another two systematic reviews based on RCTs using antidepressants as primary intervention and placebo as control came to the opposite conclusion [26,27]. Our recent preliminary literature review suggests that the use of antidepressants to treat depressions in depressed older adults with dementia is less effective based on eight RCTs [28-35] listed on Table 1. RCTs are considered the gold standard for therapeutic intervention. Among four previous systematic reviews [9,25-27] and other two reviews [36,37], only one published RCT tested the efficacy of an antidepressant (Sertraline) for depressed NH residents with dementia [34]. This study was a randomized, placebocontrolled, double blind trial designed to test the efficacy of Sertraline in thirty one depressed female NH patients with dementia (intervention group=17, placebo group=14). Mean ages in the intervention and control groups were 88 and 90 years old, respectively. In this trial, the National Institute of Neurological and Communicative Diseases and Stroke-Alzheimer’s Disease and Related Disorders Association (NINCDS/ADRDA) criteria for probable or possible Alzheimer’s disease (AD) were used to diagnose dementia. The subjects in this study had late-stage Alzheimer’s disease. The Cornell Scale for Depression in Dementia (CSDD) was used to assess depression. Only 10% of participants met the criteria for “definite†major depression (CSDD ≥ 10 on a scale 0-38). The Gestalt scale (GS), Facial Behaviors, Cohen-Mansfield Agitation Index (CMAI), Aversive Feeding Behavior Scale (AFBS), Knit-brow face and sad face were used as secondary outcomes. 497 subjects were screened (the recruitment fraction was 6%). 101 of them were eligible (the eligible fraction was 20%). Thirty-one participants were enrolled in this study (the enrollment fraction was 31%). Twenty-seven participants completed the trial (the completion rate was 87%). In this eight week trial, Sertraline was first given at 25 mg/day for two weeks, then at 50 mg/day during the third and fourth week and finally at 100 mg/day for the last four weeks. This study reported randomization method and allocation concealment, used intention-to-treat analysis, and had a low drop rate (13%), which indicates excellent internal validity of the study. The mean CSDD scores in the intervention and placebo groups were 3.53 and 4.43, respectively, on a scale of 0-38 (0=no depression, 38=worst depression). Sertraline did not significantly reduce depression severity. Exclusion criteria in this study included participants who were on antipsychotics or antidepressants, or had a history of cancer within the past 5 year, a history of stroke, or other severe medical problems that could interfere with participation, which indicates poor external validity. Very low recruitment rate (6%) also suggests poor external validity. Despite the limitations of this RCT, it was cited 72 times since it was published in 2000 based on Web of Science [38]. Conducting a large RCT to test effectiveness of antidepressants at NH setting is urgently needed.Because of insufficient RCTs in the NH setting, it merits to examining results from RCTs that test the efficacy of antidepressants in depressed older patients with dementia in other clinical settings. Eight RCTs including only RCT at NH [28-35], are listed on Table 1. Seven out of eight RCTs were conducted in outpatient clinic settings. Two out of eight RCTs showed a statistically significant effect of reducing depression severity with antidepressants among depressed older patients with dementia. The other six RCTs didn’t show any difference in depression severity between the placebo and antidepressant groups.
In the era of evidence-based medicine, health providers often use evidence-based guidelines to guide their clinical practice. We used PubMed and the National Guideline Clearinghouse to search clinical practice guidelines based on the following two simple criteria: 1) the guidelines focused on depressed NH residents with dementia; 2) the guidelines provide at least two components i.e., quality of the evidence (level of evidence) and strength of the recommendation (grade or class). Our literature search didn’t find any clinical practice guideline that met our inclusion criteria. Nevertheless, we found two Expert Consensus papers and two guidelines which might help make an extrapolation-based decision. The first Expert Consensus paper [21] focused on management of depressed NH residents with dementia. It included a list of RCTs with levels of evidence for the recommendations. This expert consensus recommended that pharmacological interventions were effective in NH residents with major depression (level I evidence). For residents who met criteria for minor depression, alternative treatments including nonpharmacological interventions, antidepressants, and watchful waiting were recommended (level IV evidence). These recommendations, however, were not graded. In the 2nd Canadian Expert Consensus Conference on Dementia, seven RCTs were selected, reviewed, and used as supporting evidence to treat depression in depressed patients with dementia [22]. The use of antidepressants or a mood stabilizer to treat patients who are demented and suffer from disturbing emotional liability or pathological laughing and crying was determined to be a Grade B recommendation with Level 3 evidence [22]. However, this expert consensus was not specific to depressed NH residents with dementia. Two other guidelines on treating depression at NH setting recommended antidepressants, but did not provide the evidence from RCTs, levels of evidence, or grades of their recommendations [23,24]. In 2011, the American Medical Director Association (AMDA) developed a guideline to treat depression with or without dementia in the long-term care setting and was collected in National Guideline Clearinghouse. It stated “the practitioners should discuss the rationale for adding pharmacotherapy to the patient’s regimen with team members as well as with the patient and his or her family” [23]. Unfortunately, the evidence from RCTs, grades of recommendation, and levels of evidence were not provided in this guideline [23].
Taken together, the current literature suggests that the evidence of prescribing antidepressants to treat depression in depressed NH residents with dementia is inconsistent and conflicting. Thus, longterm care providers are forced to make prescribing decisions based on only negative RCT and in consistent evidence from seven RCTs at non-NH settings.
Potential Adverse Effect of Antidepressants
A recent large cohort study of 60,746 patients aged 65 to 100 years old showed that antidepressants were significantly associated with hyponatremia, increasing mortality, attempted suicide or selfharm, myocardial infarction, stroke, upper gastrointestinal bleeding, epilepsy or seizure, road traffic accidents, adverse drug reactions, falls, and fractures [39]. Perioperative use of selective serotonin reuptake inhibitors (SSRIs) was associated with increasing inpatient mortality, bleeds, and 30-day readmission in another recent large cohort study of 530,016 subjects [40]. Antidepressants were also associated with increasing bone absorption and potentially increasing fracture risk in older patients [41]. NH residents often have multi-morbidity [42] and polypharmacy [43,44]. Adding antidepressants in this vulnerable population could significantly increase drug-drug and drug-disease interactions thus further increasing the risk of polypharmacy. Not surprisingly, antidepressants are on the Beers’ list of medications that should be prescribed cautiously in geriatric population [45].Proposed Practical Approach in Prescribing Antidepressants
Antidepressants are widely prescribed to treat depressed NH residents with dementia [5,6,8] despite lack of the evidence from RCTs, systematic reviews, and evidence-based clinical guidelines. In our opinion, many depressed NH residents with dementia might not need antidepressants. Ideally, patient families, pharmacists, nursing staff, and long-term care providers at NH could work together to decide on antidepressant use and to meet the FDA and CMS regulations [1,2]. All stakeholders need to balance the limited benefits and multiple potential risks associated with antidepressants. Here, we propose a practical step-wise approach to prescribing antidepressants at NH setting for long-term care providers.First, long-term providers should share with the patients’ families, nursing staff, and other colleagues that there is little evidencebased support for antidepressant use. Engaging patients’ families, pharmacists, and nursing staff is critical for making good decisions on the use of antidepressants; Second, long-term care providers should look for potential medical causes of the depression and treat them accordingly. An example is to treat uncontrolled chronic pain; Third, long-term care providers should assess the severity of the patient’s depression i.e., differentiating between depressive symptoms versus major depression following DSM-IV [46]. Depressive symptoms or minor depression often do not require antidepressants; Fourth, long-term care providers should try non-drug therapies first such as physical activity [47] and a structured multidisciplinary approach [48] before prescribing any antidepressant. The use of pleasant events and activity participation has been studied as alternative approach to improving depression [49,50]. Group activities, oneone visit, religious service, and family visit could have positive affect in depressed NH residents; Fifth, as a last resort, the use of tricyclic antidepressants (TCAs) or SSRIs, or other types of antidepressants, if non-drug therapy approaches fail. Close monitoring for adverse effects should be in place if antidepressants are prescribed. A recent small study showed that discontinuation of antidepressants could result in rebound depressive symptoms [51]. Thus, discontinuation should be done slowly and carefully; Sixth, referral to a psychiatrist may be in order, especially a geriatric psychiatrist. Many geriatric psychiatrists have expanded their practices to the NH setting; lastly, consider tapering the patient off of the antidepressants if pharmacotherapy does not prove beneficial.
We now return to the patient described in the beginning. We decided not to prescribe an antidepressant and, after discussions with her family, suggested that palliative care should be included in her treatment goals. Several non-drug therapies were employed to attempt to alleviate the patient’s agitation and depression. For example, the nursing staff would often hold her hand and assist her to participate in simple exercise and musical events in activity room. Regular family visits were encouraged.
Conclusion
Depression and dementia are common and often co-exist among NH residents. The use of antidepressants is epidemic in this vulnerable population. However, the evidence for the efficacy of antidepressants in depressed NH residents with dementia is inconsistent and conflicting. Antidepressants are associated with multiple adverse effects. We believe that the use of antidepressants should be reduced in this population. We propose a practical step-wise approach to prescribing antidepressants for this vulnerable population in the absence of good evidence. A large RCT to test the effectiveness of antidepressants in depressed NH residents with dementia is urgently needed.Acknowledgements
We would like to thank Dr. Carol Manning, Ph.D. ABPP-CN for her critical review and input on this manuscript. Dr. Manning is Director Memory Disorders Clinic, Vice Chair for Faculty Development, Associate Professor of Neurology, Department of Neurology Box 800394, University of Virginia, Charlottesville, VA 22908References
- FDA (2013) Medication guide “antidepressant medicines, depression and other serious mental illness, and suicidal thoughts or action”.
- Long Term Care Professional Leadership Council, American College of Health Care Administrators, American Medical Directors Association, American Society of Consultant Pharmacists, National Association Directors of Nursing Administration/Long Term Care (2008) Use of antidepressants in nursing home residents-a joint statement of the member of the long-term care professional leadership council (LTCPLC). Consult Pharm 23:231-234.
- Peskind ER (2003) Management of depression in long-term care of patients with Alzheimer’s disease. J Am Med Dir Assoc 4: S141-S145.
- Zuidema S, Dersksen E, Verhey F, Koopmans RT (2007) Prevalence and neuropsychiatric symptoms in a large sample of Dutch nursing home patients with dementia. Int J Geriatr Psychatry 22: 632-638.
- Zuidema S, Koopmans R, Verhey F (2007) Prevalence and predictors of neuropsychiatric symptoms in cognitively impaired nursing home patients. J Geriatr Psychiatry Meuro 20: 41-49.
- Seitz D, Purandare N, Conn D (2010) Prevalence of psychiatric disorders among older adults in long-term care homes: a systematic review. Int Psychogeriatr 22: 1025-1039.
- Gaboda D, Lucas J, Siegel M, Kalay E, Crystal S (2011) No longer undertreated? Depression diagnosis and antidepressant therapy in elderly long stay nursing home residents, 1999 to 2007. J Am Geriatr Soc 59: 673-680.
- Hanlon JT, Wang X, Castle NG, Stone RA, Handler SM, et al (2011) Potential underuse, overuse and inappropriate use of antidepressants in older veteran nursing home residents. J Am Geriatr Soc 59: 1412-1420.
- Thompson S, Herrmann N, Rapoport MJ, Lanctot KL (2007) Efficacy and safety of antidepressants for treatment of depression in Alzheimer’s disease: a metaanalysis. Can J Psychiatry 52: 248-255.
- Kales HC, Blow FC, Copeland LA, Bingham RC, Kammerer EE, et al (1999) Health care utilization by older patients with coexisting dementia and depression. Am J Psychiatry 156: 550-6.
- Harris MJ, Gierz M, Lohr JB (1989) Recognition and treatment of depression in Alzheimer’s disease. Geriatrics 44:26-30. Geriatrics. 44: 26-30.
- Jones BN, Reifler BV (1994) Depression coexisting with dementia: evaluation and treatment. Med Clin N Am 78: 823-840.
- Knesper DJ(1995) The depressions of Alzheimer’s disease: sorting, pharmacotherapy, and clinical advice. J Geriatr Psychiatry Neurol 8: S40-S51.[PMID: 8561843]
- Alexopoulos GS (1996) The treatment of depressed demented patients. J Clin Psychiatry 57 Suppl 14:14-20.
- Boland RJ (2000) Depression in Alzheimer’s disease and other dementias. Current psychiatry Report 2: 427-433.
- Lee HB, Lyketsos CG (2003) Depression in Alzheimer’s disease: heterogeneity and related issues. Biol Psychiatry 54: 353-362.
- Lyketsos CG, Lee HB (2004) Diagnosis and treatment of depression in Alzheimer’s disease: a practical update for the clinician. Dement Geriatr Cogn Disord 17: 55-64.
- Starkstein SE, Mizrahi R, Power BD (2008) Depression in Alzheimer’s disease: phenomenology, clinical correlates and treatment. Int Rev of Psychiatry 20: 382-8.
- Wilkins CH, Mathews J, Sheline YI (2009) Late life depression with cognitive impairment: evaluation and treatment. Clin Intervention in Aging 4: 51-57.
- Modrego PJ (2010) Depression in Alzheimer’s disease. Pathophysiology, diagnosis, and treatment. J Alzheimer’s Disease 21: 1077-1087.
- American Geriatrics Society, American Association for Geriatric Psychiatry (2003) Consensus statement on improving the quality of mental health care in U.S. nursing homes: management of depression and behavioral symptoms associated with dementia. J Am Geriatr Soc 51: 1287-1298.
- Thorpe L, Groulx B, Canadian Centres for Clinical Cognitive Research (2001) Depressive syndromes in dementia. Can J Neurol Sci 28: S83-S95.
- American Medical Director Association (2011) Depression in the long term care setting.
- Kaldyand J, Tarnove L (2003) A clinical practice guideline approach to treating depression in long-term care.J Am Med Dir Assoc 4: S60-S68.
- Boyce RD, Hanlon JT, Karp JF, Kloke J, Saleh A, et al (2012) A review of the effectiveness of antidepressant medications for depressed nursing home residents. J Am Med Dir Assoc 13: 326-31.
- Nelson JC, Devanand DP (2011) A systematic review and meta-analysis of placebo-controlled antidepressant studies in people with depression and dementia. J Am Geriatr Soc 59: 577-85.
- Bains J, Birks JS, Dening TR (2002) The efficacy of antidepressants in the treatment of depression in dementia. Cochrane Database Syst Rev.
- Banerjee S, Hellier J, Dewey M, Romeo R, Ballard C, et al (2011) Sertraline or mirtazapine for depression in dementia (HTA-SADD): a randomized, multicenter, double-blind, placebo-controlled trial. Lancet 378: 403-411.
- Rosenberg PB, Drye LT, Martin BK, Frangakis C, Mintzer JE, et al (2010) Sertraline for the treatment of depression in Alzheimer disease. Am J Geriatr Psychiatry 18: 136-1345.
- de Vasconcelos Cunha UG, Lopes Rocha F, Avila de Melo R, Alves Valle E, de Souza Neto JJ, et al (2007) A placebo-controlled double-blind randomized study of venlafaxine in the treatment of depression in dementia. Dement Geriatr Cogn Disord 24: 36-41.
- Lyketsos CG, DelCampo L, Steinberg M, Miles Q, Steele CD, et al (2003) Treating depression in Alzheimer disease: efficacy and safety of sertraline therapy, and the benefits of depression reduction: the DIADS. Arch Gen Psychiatry 60: 737-46.
- Petracca GM, Chemerinski E, Starkstein SE (2001) A double-blind, placebo-controlled study of fluoxetine in depressed patients with Alzheimer's disease. Int Psychogeriatr 13: 233-240.
- Reifler BV, Teri L, Raskind M, Veith R, Barnes R, et al (1989) Double-blind trial of imipramine in Alzheimer's disease patients with and without depression. Am J Psychiatry 146: 45-49.
- Magai C, Kennedy G, Cohen CI, Gomberg D (2000) A controlled clinical trial of sertraline in the treatment of depression in nursing home patients with late-stage Alzheimer's disease. Am J Geriatr Psychiatry 8: 66-74.
- Roth M, Mountjoy CQ, Amrein R (1996) Moclobemide in elderly patients with cognitive decline and depression: an international double-blind, placebo-controlled trial. Br J Psychiatry 168: 149-157.
- ChengHY (2009) A pilot study of assessing the quality of evidence from randomized, controlled drug and nutritional supplement trials conducted among nursing home residents between 1968 and 2004: what can we learn? J Am Med Dir Assoc 10: 28-35.
- Rhodes-Kropf J, Cheng H, Castillo EH, Fulton AT (2011) Managing the patient with dementia in long-term care. Clin Geriatr Med 27: 135-152.
- (2013) Web of Science.
- Coupland C, Dhiman P, Morriss R, Arthur A, Barton G, et al (2011) Antidepressant use and risk of adverse outcomes in older people: population based cohort study. BMJ 343: d4551.
- Auerbach AD, Vittinghoff E, Maselli J, Pekow PS, Young JQ, et al (2013) Perioperative use of selective serotonin reuptake inhibitors and risks for adverse outcomes of surgery. JAMA Intern Med 173: 1075-1081.
- Shea ML, Garfield LD, Teitelbaum S, Civitelli R, Mulsant BH, et al (2013) Serotonin-norepinephrine reuptake inhibitor therapy in late-life depression is associated with increased marker of bone resorption. Osteoporosis Int 24: 1741-1749.
- Moore KL, Boscardin WJ, Steinman MA, Schwartz JB (2012) Age and sex variation in prevalence of chronic medical conditions in older residents of U.S. nursing homes. J Am Geriatr Soc 60: 756-764.
- Onder G, Liperoti R, Fialova D, Topinkova E, and Tosato M, et al (2012) Polypharmacy in nursing home in Europe: results from the SHELTER study. J Gerontol A Biol Sci Med Sci 67: 698-704.
- Dwyer LL, Han B, Woodwell DA, Rechtsteiner EA (2010) Polypharmacy in nursing home residents in the United States: results of the 2004 National Nursing Home Survey. Am J Geriatr Pharmacother 8: 63-72.
- American Geriatrics Society Beers Criteria Update Expert Panel (2012) American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 60: 616-631.
- American psychiatric association, Washington DC (2000) Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV).
- Potter R, Ellard D, Rees K, Thoroggod M (2011) A systematic review of the effects of physical activity on physical functioning, quality of life and depression in older people with dementia. Int J Geriatr Psychiatry 26: 1000-1011.
- Leontjevas R, Gerritsen DL, Smalbrugge M, Teerenstra S, Vernooij-Dassen MJ, et al (2013) A structural multidisciplinary approach to depression management in nursing-home residents: a multicenter, stepped-wedge cluster-randomized trial. Lancet 381: 2255-2264.
- Meeks S, Young CM, Looney SW (2007) Activity participation and affect among nursing home residents: support for a behavioural model of depression. Aging Ment Health 11: 751-760.
- Meeks S, Shah SN, Ramsey SK (2009) The Pleasant Events Schedule - nursing home version: a useful tool for behavioral interventions in long-term care. Aging Ment Health 13: 445-455.
- Bergh S, Selbæk G, Engedal K (2012) Discontinuation of antidepressants in people with dementia and neuropsychiatric symptoms (DESEP study): double blind, randomised, parallel group, placebo controlled trial. BMJ 344: e1566.