Journal of Geriatrics and Palliative Care
Download PDF
Research Article
An Initiative of a Nursing Home Outreach Counseling to Improving Palliative Care in Eastern of Saxony-Anhalt, Germany
Behrendt D*, Richter N and Sumngern C
Städtisches Klinikum Dessau, Auenweg 38, 06847 Dessau-Rosslau, Germany
*Address for Correspondence: Daniel Behrendt, Städtisches Klinikum Dessau, Auenweg 38, 06847 Dessau-Rosslau, Germany. E-mail: daniel.behrendt@klinikum-dessau.de
Submission: 19 September, 2023
Accepted: 10 October, 2023
Published: 13 October, 2023
Copyright: © 2023 Behrendt D, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Advance Care Planning; Case Management; Nursing Home; Outreach Counseling; Palliative Care
Abstract
Outreach programs have been usually designed to strengthen institutional services. Counseling plays an important role in palliative care for people with life-limiting conditions through building relationships between staff, patients, and families. This study aimed to initiate a nursing home outreach counseling in palliative care based on the combination of Case Management and Advance Care Planning concepts, and to pilot the implementation of developed nursing home outreach counseling for residents. Phase Model recommended by Peipe was applied for this development. Comprehensive palliative care, waiting time for initial counseling, and cost-benefits were evaluated. Descriptive and frequency statistics were used for data analysis. This article reports the initiative of nursing home outreach counseling in palliative care by two case managers at five nursing homes in the eastern Saxony-Anhalt. Multidiscipline collaboration played a crucial role in outreach counseling in palliative care for the residents.
There were three significant documents for outreach counseling in palliative care for nursing home residents:
(1) Palliative Care Pass
(2) PalliDoc® in palliative
(3) Counseling Performing Checklist.
The findings from initial small-scale study (n = 47), nursing home outreach counseling indicated the effectiveness on the comprehensive palliative care and also decreased waiting time for initial counseling services. The initial counseling service was provided for 59.6 % of the residents within three days and for 34 % between four to six days (n = 16, 34 %). This counseling did not greatly indicate the benefits of financial organizations.
(1) Palliative Care Pass
(2) PalliDoc® in palliative
(3) Counseling Performing Checklist.
The findings from initial small-scale study (n = 47), nursing home outreach counseling indicated the effectiveness on the comprehensive palliative care and also decreased waiting time for initial counseling services. The initial counseling service was provided for 59.6 % of the residents within three days and for 34 % between four to six days (n = 16, 34 %). This counseling did not greatly indicate the benefits of financial organizations.
Nursing home outreach counseling was beneficial in providing palliative care for the residents and families to meet the important aspects of death with dignity. This counseling model enhanced the ease of care management in palliative care for nursing home staff and decreased the affects of delayed receiving counseling. However, a larger confirmatory study is needed for further researches.
Introduction
The amount of nursing homes has been increasing in Germany regarding to providing support for the elderly in long-term care to ensure a dignified care and respect preferences of care at the end-of-life
[1,2]. Health insurance is mandatory in Germany and plays important roles influencing QOL among the instituted elderly [3]. However, older people prefer to live at home with their loved ones as long as possible, consequently, they often admit to nursing homes with a high age. This means, they have short length of stay in nursing home for being prepared for their dying process. Therefore, care management in the individual context of the elderly among care teams and networks for dignified living is one of practical-theoretical- and ethical challenges for residential care facilities.
Palliative care was defined by World Health Organization (WHO) as an approach improving the quality of life of individuals and their families who are facing problems associated with life-threatening illness, whether physical, psychological, social, or spiritual [4]. Furthermore, essential attributes of ageing-based palliative care models identified by policy were communication and coordination between providers, skill enhancement, and capacity to respond rapidly to individuals’ changing needs and preferences over time [5]. Nursing home deaths and Advance Care Planning (ACP) provided advance directive care have been concerned especially during Covid-19 and beyond to promote an appropriate death with meaningful as possible for both the elderly and the family members [6].
ACP has been confirmed as a crucial intervention in improving communication, and care satisfaction as well as reduced staff distress through decision-making proceses [7,8]. Certainly, ACP strengthens the iterative process of discussion, decision-making, and documentation related to end-of-life [9]. Thus, ACP has been confirmed for improving quality of end-of-life care and patient and family satisfaction, and reduces stress, anxiety, and depression in surviving relatives [10]. Besides, Case Management (CM) was the element consistently reported in palliative care models for studies provided evidence for effectiveness on health outcomes [5,11]. CM has been shown the benefits on providing counseling and palliative care[12,13]. Integrating CM into palliative care is a logical, feasible, and effective strategy to improve the care of seriously ill patients [14]. Regarding literature, case managers under CM concept, as patient advocates, are perfectly positioned to facilitate the necessary palliative care or end-of-life care conversation, including advance care planning, and securing the essential legal documents that clearly note the patient and support system wishes and care goals [13].
Counseling is one of the most common components providing psycho-social support for individuals in palliative care [15]. The counseling profession needs to engage in interdisciplinary
collaboration, and counseling techniques obtain an effective
communication for buiding the relationships between staff, residents,
and families [16]. Counseling services in long-term care with a
variety of counseling purposes have been established in Germany to
support care recipients and their relatives [17]. As well, the outreach
counseling service has been confirmed as a practical care model in
certain situations of palliative care which gives a great support for
care receivers and caregivers [18].
This study was developed regarding the quality improvement and
the national health policies aimed at improving ambulant palliative
care services for long-term care facilities in eastern Saxony-Anhalt. By
German policies, the individuals with severe advanced life-limiting
illnesses and high, complex symptom burdens have right to receive
the specialized outpatient palliative care (SAPV) which provides by
multi-professional team with heterogeneous organizational structures
in cooperation with primary care givers
[19]. Therefore, nursing home
outreach counseling service based on the combination of ACP and
CM concepts should be practical and beneficial in providing palliative
care for the residents and families to meet the important aspects of
death with dignity. This counseling model should also enhance the
ease of care management in palliative care for nursing home staff and
decrease the affects of delayed receiving counseling.
Objectives
This study aimed to initiate anursing home outreach counseling
in palliative care based on the combination of Case Management and
Advance Care Planning concepts, and to pilot the implementation of
developed nursing home outreach counseling for the residents living
in the eastern Saxony-Anhalt, Germany.
Methods
Study designs:
Phase Model recommended by Peipe version 2015 was applied
for planning the project management in this study
[20]. This
model provides guideline phases to manage the organizational
project including initial phase, definition phase, planning phase,
implementation phase, and closing phase.In this study, work plan
structurewas discussed and finaly divided into two phases and four
workplans (WPs) [Figure 1].Phase 1: planning and concept development, which included
WP-1: situation and demand analysis and WP-2: design of revised
counseling modeland
Phase 2: performing the initial small-scale study of the
implementation of nursing home outreach counseling, this phase
included WP-3: implementation of revised counseling model, and
WP-4: finding dissemination.
Phase-1:
Collaborative work among healthare providers was performed
for establishing a nursing home outreach counseling in palliative care
based on the combination of CMand ACP. Before performing the
revision of counseling service, counseling situations were discussed
among palliative care team concerning the government policies,
the possibility to access nursing home outreach counseling, and
the residents´needs and unmet needs in palliative care. In WP-2,
the developed model of outreach counseling in palliative care and
related documents were designed to providing care for nursing home
residents and families. The comprehensive palliative care, waiting
time for initial counseling, and cost-benefit were considered as study
outcomes.Phase 2:
The initial small-scale study of nursing home outreach counseling
in palliative care was conducted in five nursing homes located in
Dessau-Rosslau, eastern Saxony-Anhalt, Germany.Participants:
With our limitations to reach populations in our study, purposive
sampling was performed. During the study period, fourty-seven
residents with inclusion criteria of being 65 and older years old,
living in nursing homes, and receiving the prescriptions from their
physicians for palliative care participated in this study.Case managers were selected from Palliative Care Center with
inclusion criteria of
(1) Educating in health and social science.
(2) Having counseling experiences at least one year.
(3) Having competences in cooperation, communication, and awareness of responsibility.
(4) Being able to complete the study.
(1) Educating in health and social science.
(2) Having counseling experiences at least one year.
(3) Having competences in cooperation, communication, and awareness of responsibility.
(4) Being able to complete the study.
Data collection:
Data were gathered from the residents´ charts and the palliative care records of healthcare providers. Data included residents´characteristics: age, gender, marital status, primary
diagnosis, and care grade were collected. Besides, waiting time for
initial counseling, duration of receiving nursing home outreach
counseling service were recorded by counting the number of days
from the date of registration. The cost benefit of nursing home
outreach counseling service and the needs of advice for residents
and/or families regarding advance directive or living wills, decision making
authority/ power of attorney, and the symptoms in the initial
assessment were identified. Data were anonymously organized and
calculated by using program Excel of the Microsoft Office version
2010.Data Analysis:
Data were presented as means with standard deviation for age,
waiting time for initial counseling, and duration of receiving nursing
home outreach counseling service. Numbers and percentages were
used for reporting for gender, marital status, primary diagnosis, care
grade, present symptoms, and needs of advice for residents and/or
families. In addition, the cost of providing nursing home outreach
counseling in palliative care were reported the summary of income,
expenses, and net balance in Euro (EUR).Ethical Considerations:
This study was approved for developing the palliative care model
by a multidisciplinary team aimed at a quality improvement of
palliative care, Palliative Care Center, eastern Saxony-Anhalt,
Germany. The requests for permission to conduct the study in
nursing homes were made by Palliative Care Center. Considering
recognized standards and the Declaration of Helsinki, informed
consent was obtained from individual residents or the legally
authorized representative prior to participation in the small-scale
implementation study. Data were gathered from the residents´ charts
and the palliative care records of healthcare providers and processed
anonymously in an Excel database.Results
Phase-1 Results:
In this phase, the needs and situations to starting a nursing home
outreach counseling in palliative care, designs of counseling services,
and critical documents were analyzed and discussed among healthcare
providers from Palliative Care Center and representative staff
from nursing homes. In WP-1, we found the challenges to improve
palliative care through the nursing home outreach counseling in
palliative care for the residents regarding their needs of palliative care
and the integrated care agreement between the SAPVandthe AOK
Saxony-Anhalt in accordance with § 140a ff SGB V in conjunction
with § 132d, § 37b SGB V.Design of nursing home outreach counseling:
In WP-2, nursing home outreach counseling in palliative care
based on the combination of CM and ACP concepts was designed.
The revised model was created tincluding the details of nursing
home outreach counseling services which well-defined palliative
care assessment, eligibility criteria for the target group, and
registration system. Case manager was assigned to taking leader
roles on the collaborative work among Palliative Care Center (PCC),
SAPV, ambulant hospice service in Saxony-Alhalt, and nursing
homes. Nursing home staff were informed and well prepaired for
understanding the nursing home outreach counseling care model.
They understood the eligibility criteria for the target group-specific
counseling service, and registration procedure. After registration,
an initial counseling was planned to provide within four weeks and
service should be completed for all key domains of palliative care
within three months.In registration step, nursing home staff was assigned to assess the
residents´care needs by using five care grades defined long-term care
needs, the classification of the type and severity of the impairment
by long-term care insurance regulated by law in the Eleventh Book
of the German Social Code (SGB XI)
[21]. Following the indication
of long-term care grades guided by Federal Ministry of Health,
Germany, an individual care need is determined and weighted based
on impairments of independence in six modules:
Module 1: Mobility (10%)
Module 2: Mental and communication-related abilities (15%)
Module 3: Behaviour and psychological issues (15%)
Module 4: Self care (40%)
Module 5: Independent handling of requirements and challenges
associated with illness or therapy – and their management (20%)
Module 6: Everyday life and social contacts (15%).
The weighted rerults are valued in range from 0 to 100 points, and
then the values are divided into five grades of care need. The five care
grades are stepped: from minimal impairment of independence or
ability (care grade-1) to the most serious impairment of independence
or ability, which places special demands on the provision of longterm
care (care grade-5).
Significant documents:
The three significant documents were developed for using in
nursing home outreach counseling services including (1) Palliative
Care Pass [Palliativpass], (2) PalliDoc® in palliative, (3) Counseling
Performing Checklist.Regarding to Palliative Care Pass, this legal document indicates
the residents´ living wills of self-determination at the end of their
life or in health emergencies, whereas PalliDoc® in palliativeis
anonlined documents available in platforms of PalliDoc® for sharing
information of counseling services among the palliative care team.
According to the quality of care, Counseling Performing Checklist
[Evaluation der Informationsbedarfe SAPV] was used for measuring
the comprehensive palliative care for an individual.Counseling
Performing Checklist, derived from SAPV-Palliative Care Assessment,
was developed by palliative care team to gain information of the
residents and their contact persons and/or networks that involve in
caring for the residents at the end of their life. The records included
demographic data, and general information related to health
insurerances and/or sources of payment, the residents´ diagnosises
and their present symptoms. Needs of counseling were categorized
into three main themes:
(1) Treatment and medicine use
(2) Psychosocial aspects i.e., self-management, family problems
with taking care for the residents, etc.,
(3) Plan for their end-of-life, especially about preparing the
legal documents such as giving authority of decision making, and
redidents´s directives.
Study outcomes:
Following the benefits related to three key components of study triangle
by Peipe published in 2015 [22], symbolically including
service, time, and cost were used for evaluating the advantages of the
implementation of the nursing home outreach counseling.Service: receiving an individual comprehensive palliative
care using the Counseling Performing Checklist for the service
evaluation.
Time: waiting time from the date of registration until the date of
receiving the first counseling.
Cost: Net balance for providing outreach counseling service of
Palliative Care Center.
Phase-2: results:
The initial small-scale implementation study of nursing home
outreach counseling in palliative careThe nursing home outreach counseling services were provided
by two case managers into five nursing homes for fourty-seven
residents. There were fifty-three registered residents for palliative
care consultation to the PCC. There were five residents who refused
to participate in the study, and one died before performing the
counseling based on ACP in palliative care. Finally, data from fourtyseven
residents and their families were analyzed.
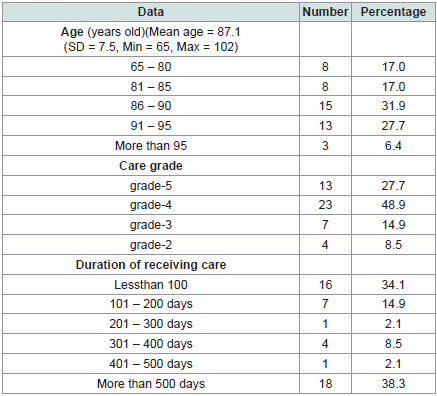
The implementation of nursing home outreach counseling was
carried out with residents and/or their families from five nursing
homes. The demographic data were reported [Table 1] , the results
depicted mean age of 87.1(SD = 7.5, Max = 102, Min = 65). Of these,
there were 82% over 80 years old (n = 39), 78.7% female (n = 37),
and 97.9% widow (n= 46). More than half of the residents (59.6%,
n = 28) received countinum care services from nursing home
outreach counseling team after registration for up to one year, and
40.4 % of them (n = 19) for more than one year. The stay in service
was in a wide-range from 2 days to 1,435 days (Mean = 487.2, SD
= 467.8).We also found that dementia was the highest number of
primary diagnosis (46.8%, n = 22) followed by carcinoma (27.7%,
n = 13), stroke (8.5%, n = 4), heart failure (8.5%, n = 4), and kidney
disease (8.5%, n = 4).
The results indicated a high percentage of residents with
severe impairments, care grade-4, which described the most severe
impairments of residents in need of care, dominates with 48.9
(n = 23). Care grade-5 was documented for 27.7% (n = 13) of residents.
This is also classified as having the most severe impairments, and
special requirements are placed on the nursing care profile. Care
grade-3 was represented by 14.9% (n = 7), and care grade-2 by 8.5%
(n = 4) of the residents.
Thirty residents received counseling being accompanied by
their relatives (63.8%), for eight residents with caring nursing staff
(17%), and five residents with legal guardians (10.6%), and four
residents without accompanied person (8.5%). We found 72.3%
(n = 34) of the residents´underlying diseases that did not relate
to diseases in oncology, whereas there were 27.7% (n = 13) of the
residents diagnosed with having cancer.
There were 38 residents (80.9%) able to provide documents of
power attorney. Five residents (10.6%) had documents indicating
their legal guardian as their legal representative. The non-existence of
written power of attorney was found by three residents (6.4%).
In this pilot study, the results depicted a mean waiting time of 3.4
days (SD = 2.3, Min = 1, Max = 14). The first outreach counseling in
palliative care could be performed in nursing homes for twenty-eight
residents within three days (n = 28, 59.6%), and for sixteen residents
between four to six days (n = 16, 34%). Only three residents waited
for the services more than seven days (6.4%) due to working overload
of case managers. Considering the time use of counseling, palliative
care staff spent 50 – 120 minutes (Mean = 64.3, SD = 12.6) for giving
advice to each resident with/ without family in the first counseling.
More than half of residents (n = 25, 53.2%) received yearly palliative
care assessment.
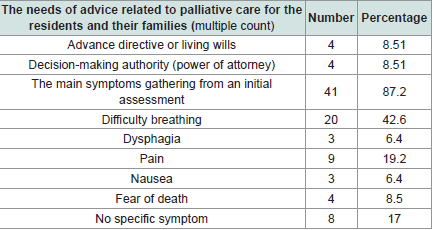
Results from using the Counseling Performing Checklist for
palliative care assesmnet, the residents and their families needed
advice and information support related to palliative care included
advance directive (N = 4, 8.5%), and decision-making authority
(power of attorney) (n = 4, 8.5%). The residents and/or families
received counseling about how to manage their present symptoms
[Table 2] including difficulty breathing (n = 20, 42.6%), dysphagia
(n = 3, 6.4%), pain (n = 9, 23.4%), nausea (n = 3, 6.4%), and fear of
death (n = 4, 8.5%). All participants received palliative care plans and
handbooks.
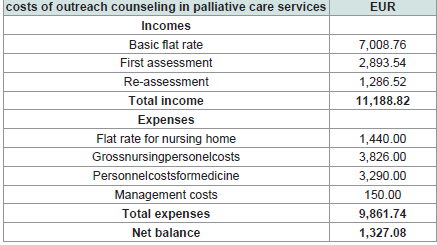
Concerning the cost of outreach counseling recording by
Palliative Care Center [Table 3] , the findings indicated the little cost-
Table 1: The report of demographic data among the residents and duration of
receiving care from nursing home outreach counseling in palliative care (N =47).
benefits as positive of net balance from this small-scale pilot study
with 1,327.08 EUR.
During the study period, a total 47 residents, there were 38.5% of
residents (n = 13) that required emergency treatments in emergency
room in hospital, and eight of them needed to be admitted in hospital.
At the end of this study, 70.2% of participants (n = 33) died in nursing
home. Whereas 38.3% of participants (n = 18) were transferred to the
hospice center due to deterioration in their state of health and 29.8%
of participants (n = 14) continued receiving services from deliverly
counseling team.
Discussion
Nowadays, health insurance is mandatory in Germany, namely,
most German senior citizens are covered by statutory health
insurance (SHI) system or by choosing private health insurance
(PHI) [3]. A comprehensive insurance obligation enacted in § 140a ff
German Social Code, Book V (SGB V), German Social Code, Book V in
conjunction with § 132d, § 37b SGB V, German Social Code, Book XI
(SGB XI) applies for everyone who needs long-term care
[21]. Those
with statutory insurance are automatically enrolled in social longterm
care insurance and privately insured persons must purchase
private long-term care insurance. Additionally, based on framework
of hospice and palliative care, it is obligatory for the health insurance
to provide individual counseling services for those affected and
their relatives [23].
According to palliative care, chronic diseases are at the focus of
care for nursing home residents [24,25]. They need support from
health professionals to decrease their physical and mental health
problems for maintaining their functions and human diginity
until their end-of-life [2]. Quality of life and the well-being of both
residents and staff have been mentioned as sensitive indicators
related to maintianing a standard quality of care in nursing homes
[26]. In addition, death with dignity in in nursing home has
been increasing concerned. The published results from narrative
interviews in nursing homes, the author concluded the persepectives
of residents´perspectives on dying that they concerned death with
dignity in the meaning of death at the right time with the aspects of
(1) Being active to the very last,
(2) Respecting one’s will and being allowed to die,
(3) Not being in pain, and
(4) Being amongst persons close to one [2].
Counseling services for the elderly in Germany in the past were
organized by a wide range of different actors, such as insurance
funds, public service, non-profit organization, and service providers
[27]. Consequently, the uncoordinated counseling services and the
difficulties establishing continuous case management services were
discussed for improving care services.
Concerning integrated care agreements regarding the German
policies and quality improvement of palliative care, the outreach
counseling was developed in this study as a service in a right
circumstance for the nursing home residents. The model focused on
individual needs and multidisciplinary approach in palliative care to
meet the important aspects of death with dignity in nursing home.
This nursing home outreach counseling was intended to provide
low-barrier access to palliative care services and to offer instituted
elderly anticipatory therapy and treatment planning among the
nursing homes residents. The basic prerequisite for this was that all
those involved in the treatment were aware of the patient’s wishes and
that the information could be accessed and retrieved at any time for
palliative care team.
In the literature, CM has been mentioned as a key component
in the care of seriously ill persons with complex needs and provides
guidelines for case managers to deliver palliative care [14]. CM has
been integrated in palliative care for improving symptoms, quality
of life, patient- and family satisfaction with care [28]. In addition,
ACP is a well-known concept for quality improvement and providing
shared decision-making for end-of-life for the nursing home residents
[8,29-32]. Although ACP benefits on improving individual autonomy
and communication in the context of anticipated deterioration
and end-of-life care, nursing home staff ther are little refections in
practices [33]. As a report of the study in Norwegian nursing homes,
the findings indicated approximately two-thirds reported that they
always or usually undertook ACP and only one-third of them had
written guidelines [29]. The study in settings from long-term care
facilities in Germany reported that ACP consultation in palliative
care was offered to 46 % residents [32].
In this study, nursing home outreach counseling in palliative
care was structured based on the combination of CM and ACP. This
revised counseling service has resulted in the adjustment of roles and
procedures of providing palliative care for the nursing home elderly.
In way of outreach counseling service, case managers from Palliative
Care Center were 24/7 on-call availability. They took leader roles
of offering an ACP for the instituted elderly of providing outreach
counseling for an individual concerns, including physical and
psychological support, and/or treatments for discomforts in health
conditions at the endof their life. They identified the residents´needs
and connected the residents with palliative care networks, and
with the resident´ s family and friends for providing physical and
psychological care and services directly at nursing homes. In addition,
case managers focused on empowering the residents and their families
by counseling services and providing skill development to manage
their symptoms and difficult situations at the end of their life. This
agrees with the definition of case managers as patient advocates, they
are perfectly positioned to facilitate the necessary palliative care or
end-of-life care conversation, including advance care planning, and
securing the essential legal documents that clearly note the patient
and support system wishes and care goals [13].
Palliative care has been directed by WHO to recognise the need
for developing palliative care that targets all age groups of patients
and families suffering from diseases or conditions in need of palliative
care [34]. According to the statistical report, the needs of palliative
care for the residents at the end of life in German long-term care
facilities have been increasing [32]. Nowadays, other diagnoses such
as dementia, stroke, Parkinson’s, heart failure, kidney, liver, and lung
diseases come into focus instead of cancers or tumors in palliative
care and counseling services in nursing homes [19,25]. In this study,
we also found that dementia was the highest number of diagnoses for
almost half of the residents among the others including carcinoma,
stroke, heart failure, and kidney disease. Palliative care for the
dementia people has been a special challenge because of limitations
of identifying their needs, consequently they are being unfortunately
still disadvantaged in palliative care for them [25].
It is noted that the elderly, especially in middle-old and oldest old
groups with physical and/or mental deterioration need different
concerns for providing palliative care from the younger people. The
topics related to developing a deliberate policy for the elderly who
wish to finish their life have been carefully discussed. The study in the
Netherlands depicted the phenomina of ready to give up life among
the elderly from the reflective lifeworld reseach design
[35]. These authors also presented a compassion understanding of the elderly
who feel life is completed and no longer worth living and opointed the
concerning of the differences between death wishes and depression.
According to the Long-Term Care Insurance Act (German
Social Code – SGB XI), care is required by those persons who – due
to an illness or disability – are permanently in need of help to a
substantial degree [36]. Since 2015, five long-term care gradeshave
been used to classify the type and severity of impairment in physical,
mental, and/or psychological. Palliative care coverage is provided
care for persons with all care grades through social or private longterm
care insurance. In this study, almost all residents (76.6%) were
determined their care needs as care grade-4, and care grade-5 which
described the most severe impairments of residents in need of care
which documented in their profiles. The results also found 17.9% of
residents with care grade-3 and 8.5% of residents with care grade-2.
These groups of residents could possiblily continue their active life
in variety activites in nursing homes. However, elderly people often
are more susceptible to health problems than other younger people.
Thus, elderly may rapidly transform their health status from active
into dependency or incapability. Thiel, et al. (2021) ephasized the use
of counseling for promoting physical activity among the residents
with the individual-level assessment as a maximum level of care with
care grade-4 (out of 5) in German healthcare system [37].
The results from our study also indicated that residents and their
families needed advice related to end of life care which included
topics not only about medications and socio-psychological support,
but also about living wills, power of attorney (decision-making
authority), and place of death. It was noted by Gjerberg, et al. that
the conversations among the professionals and residents was seldom,
because the primarily conversations normally took place when the
patient’s health condition deteriorated, when the patient entered the
last phase of life, or in connection with the admission interview [29].
Thus, hospitalisation, pain relief and cardiopulmonary resuscitation
(CPR) were the most frequent topics that pofessionals most often did
coversation with next of kin. Meanwhile, Cagle et al. concluded their
study related to caring for dying patients in the nursing homes that
the dying perspectives of residents at their end of life were identified
including received good care, not being alone, suffering ended with
death, hospice involved in pain and symptom management, and
being physically intellectually, and emotionally prepared [38].
Likewise, an explorative study in German nursing homes focusing
on living, not dying, those residents described their needs in palliative
care as:
(1) Being recognised as a person
(2) Having a choice and being in control
(3) Being connected to family and the world outside
(4) Being spiritually connected
(5) Physical comfort [26].
These concerns reflected the importance of early integration of
counseling in palliative care for maintaining the quality of life until
the last breath of the residents.
Even though only 6.4% (n = 3) of residents and their families did
not perform the power of attorney document in this study, it also
affected the quality of care for the residents in nursing homes. In these
cases, the residents and the legally authorized representative received
suppor services to manage and complte a written power of attorney.
Generally, appropriate care plans and supportive documents are
important for providing decent services for the instituted elderly.In
this study, Palliative Care Pass, PalliDoc® in palliative, and Counseling
Performing Checklist were developed and mainly used by palliative
care team for nursing home-based counseling services. Because
of concerning on these significant documents, initial medical care
was possibly initiated in nursing homes for symptom management
based on the wishes of residents and families in cases of crisis and/ or
emergency situations at the end of their life. Literatures cited that an
increasing age of the elderly related to high rates of hospital admission
and death [39]. The collaborative services were planned and provided
by palliative care team and nursing home staff. Moreover, it may be
advisable to involve the palliative care team in the further course to
avoid so-called revolving door effects in the sense of unnecessary and
recurrent hospital admissions and/or emergency department visits.
Thus, high percentages (70.2%) of received nursing home outreach
counseling residents peacefully died in their familiar nursing home
environment. The recent study review reported about documentation
of older people´s end-of-life care in the context of specialized palliative
care that the most common clinical notes in older people’s patient
records concerned interventions (mostly related pharmacological
interventions), problems (pain being the most frequent, followed
by circulatory, nutrition, and anxiety problems), people’s wishes
and wellbeing-related details [40]. This report also indicated that
symptom assessment tools, except for pain assessments, were rarely
used.
Data sharing has been developed and used among healthcare
providers in long-term care facilities aiming to increase quality of
care, better evidence practice and more robustly inform regional and
national policies [41]. Using technology benefits on palliative care, it
enables the remote connections among patients, providers, and the
care team in palliative care [42]. In this study, PalliDoc® in palliative
was created; this on-line platform is useful and practical for providing
a continuum of palliative care by the palliative care team. Counseling
support as a continuous process, re-assessment was at least yearly
performed regularly among the others, all significant information
related palliative care such as needs of residents and family members,
declarations of intention, and personal information were updated and
recorded in PalliDoc® in palliative. This information sharing platform
data can be used only among members of palliative care team with
personal codes.
The findings from using Counseling Performing Checklist in
this study presented that many aging the common symptoms at the
end of life was the main topic that the residents and their families
wanted to know and understand. It is interesting that nursing home
residents and their families indicated only 8.5% related to their need
of counsulting about living wills or advance directive in this study.
As well, Walther et al. reported their descriptive cross‑sectional study
from 363 records that a written advance directive was available for
47% of the residents in long-term care facilities in Germany [32].
Literature confirmed that ACP is a systematic approach leading to
the creation of advance directives in palliative care with potential
relevance to medical decision-making in German nursing homes
[43]. Thus, providers included this topic in consultations in this study
and the residents´ living wills were also recorded among the others in
resident´s Palliative Care Pass.
Principles of advance directives and good death were important
theme of counseling in palliative care. Ekberg et al. reported
their review of studies that the findings identified the providers
provided the opportunities for patients or family members to raise
illness progression or end of life matters to discuss [44]. Early
communication increases the opportunity to respect the patient’s
and family’s needs and preferences [8]. Thus, these themes should
be early concern for providing counseling for the elderly living in
nursing homes. In this way of practice, the elderly´s QOL have been
possibly concerned to maintain since they are admitted to nursing
homes until the end of their life by potential palliative care team. The
concept of good dead has been recommended for applying in nursing
homes. Vanderveken et al. reported their study that support of family,
respect for the patient as an individual, being able to say goodbye, and
euthanasia in case of unbearable suffering were important themes for
a good death [45]. The authors also pointed that being able to discuss
impending death with the patient and close relatives can be a great
relieve for them and it is very important for healthcare providers to
offer customized care for the patient.
Concerning updated palliative care needs of the residents and
their family, the palliative care assessment was designed in the
Phase-1 (WP-2) and was planned to perform the assessment every
year. Because of limitations related to personal resourece and corona
pandemic, only half of residents could be yearly assessed in this study.
The assessment included essential core elements for identifying care
and treatment needs, particularly for the last stages of life. The initial
assessment was completed with the issuing stated in the Palliative
Care Pass.Reassessments were required during the care processes and
were yearly carried out. In the reassessment, all necessary documents
were reviewed again. The previous planning, future treatment
strategies and wills were revised with the participating residents and/
or authorized representatives.
As early palliative care benefitson symptoms improvement,
quality of life, mood, and satisfaction [46]. Providing palliative
care based on the combination of CM and ACP, early consultation
about the needs related to physical- and sychological symptoms
and advance directive among the others has been concerned for the
residents and their families. In geropalliative care, high-quality end of-
life communication between healthcare professionals, patients
and/or their family caregivers improves quality of life and reduces
non-beneficial care at the end of life [47].
End-of-life communication contributes to palliative-oriented
care in nursing homes by three machanisms:
(1) Promotion of family carers’ understanding about their family
member’s health condition, prognosis, and treatments
available
(2) Fostering of shared decision-making between healthcare
professionals and residents/family carers
(3) Using and improving knowledge about residents’ preferences
[48]. Although, persons with psychosocial distress, especially
from their serious health problems perceived that supportive services
including palliative care could alleviate their suffering, they often
decline and/or avoid the services because of lack of understanding
[49]. Literatures concluded that patients with incurable illness
receiving early palliative care including counseling had better quality
of life, less intensive medical care, improved quality outcomes, and
cost savings at the end of life [50-52]. However, waiting time for
counseling, receivers has been commonly perceived that it takes long
time until becoming the services. The early palliative care consultation
has been varying defined. For instance, Bakitas et al. defined the early
initiation of concurrent palliative oncology care including in-person
counsultation as within 30 to 60 days of diagnosis [53]. Whereas
Robbins et al. defined early palliative care consultation timing as
more than 90 days before deathin their retrospective cohort
study [54]. The counseling service should be carried out promptly and
without a long waiting time. In this pilot study, 93.6 % of the residents
received the first counseling within six days and 59.6 % within
three days after registration to the case managers of the outreach
counseling service. This result confirms the effects of nursing home based
counseling on decreasing the waiting time of the counseling
for the residents. In addition, counseling in palliative care generally
needs time for giving advice. In this outreach counseling, the
counselors spent 50-120 minutes for giving the first service to each
resident with/ without family in this study. Hickman, et al. concluded
that the robust ACP implementation in nursing homes needed time
and resources [30].
This implementation of outreach counseling in palliative care
reflects the positive effects of healthcare policies which made practice
for care and cost management easier than in the past. In last two
decade, the establishment of independent units with specific service
offers ultimately led to a rise in the cost of services, which at that time
were not covered by the insurance benefits in care services for the
elderly in Germany [27]. In our study, outreach counseling did not
greatly indicate the benefits on financial evaluation of organizations
related to providing palliative care. This is similar with the sudy in
Turkey that did not find the advantage regarding health costs from
the intervention the case management model in the palliative care
[28]. However, the outreach conseling made the budget management
easier than the traditional one for residents and nursing homes in
this pilot study.
It was also noted that, even though nursing homes did not pay for
the counseling services outside homes in the traditional counseling
services, but the expenditures and barriers of service managements
related to resouce utilization of nursing homes such as persons
and times were highly concerned. In this study, the counseling was
provided by palliative care team organized by case managers from
Palliative Care Center. They co-operated with outsourcing palliative
care providers such as staff from SAPV and Saxony-Anhalt Hospice
Service for providing ambulant services in nursing homes. These
outsourcing staff and the cooperating networks received standard
rate by law of the selective contract from the long-term care system.
Thus, the regulations related to the payment from healthcare
insurance system made cost-transparency possible because the
cooperating organizations could receive a defined flat rate for each
service of counseling.
Palliative care is concerned not only with all aspects of the
patient’s needs, but also with the needs of the family and of the
health-care provider [34]. Palliative care is a professional discipline
that is well positioned to work together with the care team to support
the physical, emotional, social, spiritual, informational, and decisionmaking
needs [34,55]. As well, counselors working in places where
providing new way of service, they need to engage in interdisciplinary
collaboration [56]. In Germany, the report of care services for elderly in
nearly past two decades indicated that social workers are mainly active
within the area of counseling of the care dependent elderly and their
relatives or are responsible for development and implementation of
quality management approaches [27]. Interprofessional collaboration
among palliative care networks has been concerned for strengthening
nursing home outreach counseling service. It is interesting that the
report of a previous pubished study in 2022, the residents´records
from long-term care facilities in Lower Saxony, Germany indicated
only 6% of residents in long-term facilities got involved in caring
from a specialized palliative care team and 14% from hospice service
[32]. In this study, case managers were palliative care nurses from
Palliative Care Center. They took roles in all processes of performing
counseling services. They managed for outreachdecent care for the
residents and families providing by palliative care networks such as
professionally trained nursing staff, social workers, spiritual carers,
and staff from Specialized Ambulatory Palliative Care [Spezialisierten
Ambulanten Palliativversorgung (SAPV)], and Saxony-Anhalt
Hospice Service [Hospizdienst Sachsen-Anhalt].
Fulfiling palliative care needs of the residents and their families;
counseling services need the persons with special trianing in palliative
care and also need nursing home staff for service cooperation, which
possible impact on daily working load among staff. Nursing homes
have been long time persistent encountered with staff shortages,
especially especially in the Covid-19 pandemic. It is noted from a
recent study that, the number of staff hours in nursing homes did not
decrease, but the perception of shortages has been driven by increased
stresses and demands on staff time due to the pandemic [57]. As
well, specialist palliative care alone cannot provide comprehensive
palliative care covering the needs of residents and families, especially
in the Covid-19 pandemic [44]. Supportive persons and/or networks
play important roles in fulfilling the needs of instituted elderly in
palliative care. Non-professional or informal care givers have been
considered for solving this problem [58,59]. Integrated counseling
into routine work and getting support from other professionals
and supportive staff should promote effective palliative care for the
residents in nursing homes. In our study, case managers organized to
performing outreach counseling service from collaborative networks
such as physicians, professionally trained nursing staff, social services,
spiritual care, or hospice employees.
In summary, this outreach counseling was designed for providing
services inside nursing homes; it is practical and covenient in view
of management. Case managers could organize and plan services
with palliative care networks both from nursing home, and from
out-source organizations. The resource utilization of such personals
and time were decreased. It is noticed that the cooperative staff for
outreach counseling may not need to obtain the high qualification in
a crisis of staff-shortage, but they should have good compentencies
of responsibility, communication, organization among residents,
palliative care team, instututes, and out-source services/ networks. As
well as they should organize the related information and important
documents by law and policies well. According to palliative
care for ageing population needed essential elements related to
communication and coordination between providers (including
primary care), skill enhancement, and capacity to respond rapidly
to individuals’ changing needs and preferences over time [5]. The
corona pandemics and/or other crisis situations principally impact
on both care recipients and care providers. Thus, this outreach
counseling is a practical care model for nursing home that promotes
staff´s commitment in the goal of best possible palliative care for the
residents and families.
Conclusions
This nursing home outreach counseling based on the combination
of CM and ACP showed the benefits on the ease of care
management in palliative care, a decresing waiting time for initial
counseling and a comprehensive palliative care for the residents and
families to meet the important aspects of death with dignity. Nursing
home based-counseling is feasible in nursing homes even in times
of a crisis situation due to COVID-19 pandemic and staff shortages.
Nursing home outreach counseling could ensure the efffective
advance directives for the residents and their family memebers. It
is noted that strengthening the collaborative work of nursing home
outreach counseling could be designed through the combination
of CM and ACP concepts, significant documents and available
staff sharing platform, and relationship management among care
receivers and care providers from Palliative Care Center, Palliative
Care Networks, and nursing homes. However, this small-scale study
was performed to testing the revised counselling in palliative care
services; a larger confirmatory study and the two-group pretestposttest
design with random assignment are recommended for
further researchs.
Authors’ contributions:
Daniel Behrendt, Nico Richter conceptualised and developed the
study design. Nico Richter performed and processed the study under
supervision of Daniel Behrendt. Chommanard Sumngern and Daniel
Behrendt prepared the drafts of the manuscript. All authors critically
commented on the draft versions and approved the final manuscript.
Daniel Behrendt is guarantor who accepts full responsibility for the
finished work and the conduct of the study, had access to the data,
and controlled the decision to publish.Acknowledgements:
We wish to thank Städtisches Klinikum Dessau, Spezialisierten
Ambulanten Palliativversorgung (SAPV), and Hospizdienst Sachsen-
Anhalt for giving us possibilities to extend knowledges with the
growth in nursing profession. We also extend special thanks to Mr.
Sebastian Max and our colleagues from Städtisches Klinikum Dessau
for their support and cooperation. We are also grateful to Dr. Saranya
Sirikunsaruta, St Theresa International College, Thailand, for revising
the English language of this manuscript.