Journal of Neurology and Psychology
Download PDF
So what might be the
Review Article
*Address for Correspondence: N Sanjay Kumar Rao, MBBS, MD, FRCPsych, MBA, Head of Psychiatry, Annapolis Valley Health and Associate Professor of Psychiatry, Dalhousie University, 5909 Veterans’ Memorial Lane, 8th floor, Abbie J. Lane Memorial Building, QEII Health Sciences Centre, Halifax, Nova Scotia B3H 2E2, Canada, Tel: 902-365-1701 ext 2865; Fax: 902-679-1766; E-mail: nskrao@gmail.com
Citation: Sanjay Kumar Rao N. Managing Depression as a Long Term Condition. J Neurol Psychol. 2014;2(2): 7.
Copyright © 2013 Rao Sk. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology and Psychology | ISSN: 2332-3469 | Volume: 2, Issue: 2
Submission: 06 February 2014 | Accepted: 05 March 2014 | Published: 10 March 2014
Reviewed & Approved by: Dr. Ivandro Soares Monteiro, Founder & Director, ORASI Institute and EME Clinic, Portugal
Managing Depression as a Long Term Condition
N Sanjay Kumar Rao*
- Department of Psychiatry, Dalhousie University, Abbie J. Lane Memorial Building, QEII Health Sciences Centre, Halifax, Nova Scotia, Canada
*Address for Correspondence: N Sanjay Kumar Rao, MBBS, MD, FRCPsych, MBA, Head of Psychiatry, Annapolis Valley Health and Associate Professor of Psychiatry, Dalhousie University, 5909 Veterans’ Memorial Lane, 8th floor, Abbie J. Lane Memorial Building, QEII Health Sciences Centre, Halifax, Nova Scotia B3H 2E2, Canada, Tel: 902-365-1701 ext 2865; Fax: 902-679-1766; E-mail: nskrao@gmail.com
Citation: Sanjay Kumar Rao N. Managing Depression as a Long Term Condition. J Neurol Psychol. 2014;2(2): 7.
Copyright © 2013 Rao Sk. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology and Psychology | ISSN: 2332-3469 | Volume: 2, Issue: 2
Submission: 06 February 2014 | Accepted: 05 March 2014 | Published: 10 March 2014
Reviewed & Approved by: Dr. Ivandro Soares Monteiro, Founder & Director, ORASI Institute and EME Clinic, Portugal
Introduction
Depression is a ubiquitous term which is used to denote a wide variety of mental conditions. In common language people use the term depression to refer to an experience of undesirable or negative emotions. However, in mental health practice, the term depression is used to refer to a specific syndrome characterized by a cluster of phenomena [1]. It is important to make this distinction as there has been valid concerns about the increase in antidepressant prescribing [2], which may be related to over diagnosis of depression [3]. The syndrome of depression is associated with changes in mood, biological functions, cognitive dysfunctions, and loss of pleasure [1]. All health care practitioners should be aware that such a syndrome and its variants can assume a chronic course. Therefore, strategies and very importantly-services to manage the condition with a chronic perspective are important.Amongst the lay public chronic is often assumed to be irremediable, therefore use of the phrase long term condition may be more acceptable. It is important to consider that health education may be necessary to portray a long term approach as feasible and effective in the public’s mind.
Chronicity and Depression
The national co-morbidity study replication showed that the 12 month prevalence of major depression is 6.7% and about one third of these are in the severe category [4]. Severity of depression is an important predictor of chronicity [5,6]. Major depression is a remittent and recurrent condition with 80% chance of recurrence and an average of four life-time episodes [7]. Yet other estimates report 50% chance of recurrence after the first episode and 80% probability of recurrence after the second episode [8]. Recurrence by itself may does not imply long term treatment (for example certain types of migraine do not need ongoing treatment), but recurrence in depression is associated with cycle acceleration and increase in severity [9]. Antidepressant treatment reduces relapse rates in depression [10]. The number needed to treat to prevent a relapse with second generation antidepressants is 5 [11], with close to 70% reduction in relapse risk over 12 months of continuation antidepressant treatment [12].Both biological and psychological evidence shows that recurrent depression is associated with enduring changes. Right hippocampal volume reduction has been associated with recurrence of depression [13]. Subtle neurocognitive deficits, seen in euthymic patients' with major depression [14-16]. Even in the absence of depressive mood, patients may have reduced emotional reactivity to positive and negative affect [17] and increased cognitive reactivity [18]. Subsyndromal and minor depression symptoms were the most common mood state in a longitudinal study of patients with unipolar depression [19], yet again highlighting the persistent nature of the disturbance.
All of the above facets of depression are arguments for a longitudinal affliction rather than a phenomenon of isolated acute episodes.
Association of Depression with Chronic Disease
9% to 23% of chronic disease sufferers have depression and association of depression with a physical disease leads to highest illness burden [20] as shown by data from 60 countries. Depression is also associated with an increased number of symptoms in chronic diseases [21]. Patients are less likely to comply with medical treatments in presence of depression [22]. Depression has a bidirectional relationship with chronic illness and can increase the cost of care of medical illnesses [23].Depression and type 2 diabetes have a well-known reciprocal relationship [24]. Glycaemic control is impaired in the presence of depression in type 1 and type 2 diabetes [25]. Obesity increases the odds of depression and vice versa; being overweight increases the risk of depression [26]. Metabolic syndrome, a precursor of diabetes, can preceed or follow depression [27]. Smoking is not only associated condition but is also linked with depression in adolescents [28]. Not surprisingly mental health improves with smoking cessation [29]. The risks for a range of cardiovascular illnesses increase with depression. It not only increases the risk of cardiac mortality post myocardial infarction (MI), but it also increases all-cause mortality post MI, after adjusting for cardiac disease severity [31]. This association has not changed over 25 years [32]. Presence of depression in chronic obstructive pulmonary disease is strongly associated with mortality [33] and affects the outcome of pulmonary rehabilitation [34].
The association of inflammation in depression may explain at least some of its links with chronic illnesses [35]. A recent metaanalysis showed a beneficial effect of celecoxib, a non steroidal antiinflammatory drug, on depression [36].
This association of depression with long term conditions adds to the burden of illness and indicates that depression is not just a mental illness but a complex phenomenon which affects physical and mental health.
Disability is a Part of Depression
Depression is a disabling condition. Data from the World Health Organization shows that it is one of the most disabling health condition particularly in Europe & Americas [37]. A recent systematic review shows depression as the second most important cause of disability [38]. This review also showed that depression contributes to mortality in physical health conditions like ischemic heart disease.Only 5% of clinical trials report functional outcomes in depression [39] since there is no regulatory requirement to report functional improvements. Therefore treatments for depression have not focused on disability. Functions appears to recover with symptom improvement in depression [40] but in a 3 year follow up there were persistent deficits in social and physical functioning [41]. Depression, its sequelae or inadequate treatment for both may contribute to disability which may be chronic or intermittent. There is an overall long term impact of depression beyond the episode of depression.
The Play of Heritability and Environmental Factors in Depression
At 50 to 70% heritability, depression is a highly heritable illness [42] with estimates similar or more than chronic conditions like type 2 diabetes, cholesterol levels [41] and hypertension [43]. Whilst this is not an evidence for chronicity, it does indicate an enduring underlying predilection similar to other long term conditions.So what might be the role of environmental factors in predicting the outcome of depression? Given that many chronic conditions with similar heritability have onset or outcomes affected by sociodemographics and life style factors, something similar could be expected of depression. This indeed appears to be the case. Similar to other chronic conditions the prognosis of depression is affected by adversity [44] and influences the treatment response [45]. Childhood adversity in particular has been linked with chronicity in depression [46]. This opens avenues for nonclinical interventions, which could reduce risk factors for development of depression. Such interventions do not have to be psychological or biological but may rest on improving sociodemograhic conditions. A systematic review of befriending showed reduction in depressive symptoms and stress [47] in the community. At least one randomized controlled trial showed the beneficial effect of befriending in chronic depression in women [48] but more studies are needed to validate these findings.
Do Current Treatments Consider Long Term Depression Management?
The arguments marshalled so far indicate an enduring diathesis and potential chronicity in the course of depression. If such be the case do the treatment approaches and service delivery match the long term nature of depression?Many national recommendations suggest acute, continuation and maintenance phases of antidepressant treatment [49,50]. As mentioned earlier, long term treatment with antidepressants is worthwhile for improving treatment outcomes in depression. Amongst evidence based psychological treatments for depression cognitive behavioural therapy (CBT), behavioural activation therapy (BAT) and interpersonal therapy (IPT) have been devised as acute treatments of depression [51-53]. At least two studies have shown equivalence of BAT to antidepressant treatment [54,55].
The relapse prevention effect of psychological treatment particularly CBT, can be realized through acute and continuation phase interventions [56]. A one year follow up of patients in acute treatment randomized controlled trial of BAT, cognitive therapy and antidepressant treatment showed that the psychological therapies were equivalent to antidepressants in preventing relapse [57]. There is some evidence that IPT treatment also has a relapse prevention effect in depression particularly in combination with antidepressant treatment [52]. Mindfulness based cognitive therapy (MBCT) is yet another modality for preventing relapse which is delivered in the remittent phase of depression and has been found to be effective [59]. An 18 month follow up study of MBCT showed equivalent effectiveness to antidepressants in relapse prevention [60]. Interestingly both cognitive and mindfulness approaches seem to be effective for relapse prevention for those patients who have experienced more than 3 episodes of depression [58]. However, there remain several unanswered questions: How long does the relapse prevention effect of acute psychological treatment last? What is the value of inter episode psychological treatment in preventing relapse? Can the effect of psychological treatment be prolonged through regular booster sessions over a number of years? Does psychological treatment also improve long term functional outcomes? Even if psychological treatment turns out to be as effective as medication treatment, the real challenge is to train therapists both in right quality and quantity to supply these treatments effectively.
Pharmacotherapy has convergent evidence on chronic treatment for depression and psychological therapies have emerging evidence in this area. Depression education has undue emphasis is on acute treatment rather than maintenance, relapse prevention and long term treatment [61,62]. Thus, the depressed client may not have expectation of a long term treatment strategy. Compare this to chronic conditions like diabetes where adherence education is integral to the treatment approach. Perhaps this partly explains why the antidepressant discontinuation rates in depression are very high at 50% [63] and surpass the figures for treatment non adherence in other common chronic conditions like diabetes and hypertension [64].
Do current Service Provision Systems Reflect Long Term Management of Depression?
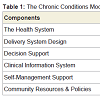
Since the literature guiding depression treatment has clearly justified long term treatment, is this reflected in practice and health care systems?Study of diabetes revolutionized the management of chronic conditions and created the chronic care approach [65]. The central premise of this approach is to create a patient centered connected health care approach which provides a continuum of care to sufferers of these conditions. This is managed through networks of care which could be collaborative and matched to suit the clinical intensity of the condition. Table 1 summarises the components of this system.
Self-care is an integral component and effective component of chronic conditions management [66]. At the clinical level good information systems are needed for operational effectiveness and decision supports systems are needed to embed evidence in practice [67]. Stepped care and collaborative in depression has borrowed heavily from this approach. Collaborative care -as defined by the use of nonmedical specialists to enhance depression management in primary care- has meta-analytic level evidence for short term and long term (up to 5 years) outcomes in depression [68]. A meta-regression analysis of collaborative care in depression showed that the ingredients determining effectiveness were: case managers with mental health background and specialist supervision [69]. Disease management programmes [70] based on principles of chronic care model also showed significant benefit in depression. Such an approach improves treatment adherence, long term outcome, patient and professional’s satisfaction [71]. It does increase the cost of medical care which is more than compensated by decrease in societal and disability costs. However such services are not routinely available. The improving access to psychological therapies (IAPT) is probably the largest service based stepped care intervention for common mental health disorders and the initial findings are promising [71]. However this service is focused on acute phase treatment with stepped psychological interventions.
Routine services in mental health do not provide provision do management based consistent with the chronic care model even though such an approach has robust evidence. Whereas in physical health problem like diabetes there is an implicit step down approach from specialist clinic to care in the community, all the stepped care pathways in depressions are really ‘step up’ approaches to treatment. Post recovery from acute episode routine follow up or discharge may ensue. Active monitoring of depression resurgence with early response system is conspicuously absent in routine services providing treatment for depression. Self-care post recovery is not clearly conceptualized as compared to chronic disease management in physical health.
Vexing Problems and Potential Solutions
Public health education issuesDepression and ensuing disability is a problem of significant magnitude and public health education must be crafted to capture the long term perspective of managing depression. Current health education works towards stigma reduction, early detection, acute treatment and recovery. These are all valuable goals. A strong focus on long term management which covers maintenance, relapse prevention, symptoms monitoring and ways to access relevant clinical services is crucial. Reduction of risk factors and encouragement of protective factors require further thought. For example exercise may be highlighted as a protective and therapeutic factor influencing mood [72,73].
Diagnostic and early detection issues
Diabetes can be diagnosed entirely based on simple repeatable laboratory investigations. This is not the case for depression. Diagnostic interviews are the gold standards but the reliability of gold standard interview also fluctuates considerably [74]. This is of serious concern, more so because these results are based on rigorous structured interviews whereas routine clinical encounters may have even less stringent standards.
One of the most commonly used scales in primary care PHQ-9, which is highly sensitive for detection of depression [75] has been called the ‘lab test’ for depression. However, PHQ-9 may not have a high positive predictive value for a current episode of major depression [76]. Screening for depression is not routinely recommended [77] due to high false positive rates and as it does not appear to change outcomes [78]. This can be partially explained by the fact that if services to manage depression are not available screening does not make a difference and if they are available screening is no longer necessary.
There are no simple answers to these issues. One potential solution could be to target recurrent depression with vigour. If recurrence be considered, it probably will increase diagnostic specificity and identify depression which is suitable for long term management.
Treatment issues
The availability of antidepressant medications is not an issue, as a large number of generics exist in the market in most economies. An inadequate treatment and antidepressant discontinuation rate is a problem in recurrent depression. However this may not be the only problem with pharmacological (or for that matter psychological) treatments. The Sequenced Treatment Alternatives to Relieve Depression (STAR*D) trial showed that treatment non response is fairly high in depression with remission rates of just around 50% after two sequential treatment steps and with remission rates of less than 25% in the third and fourth step [79]. This is hardly an encouraging scenario.
There may be a case for early combined treatment of depression with medications and psychotherapy [5280] to improve acute and long term outcomes.
Research literature has paid particular attention to persistent sub threshold symptoms of depression [81]. These require due consideration as they can be linked with relapse. A combined treatment approach may well be more applicable here. The recent literature on mindfulness based cognitive therapy for depression has the potential for addressing this gap [59]. Routine psychological interventions do not have a conceptual approach to subsyndromal mood cycling whereas mindfulness approaches for depression are adapted to address this.
With psychopharmacological treatments it is easier to apply results of clinical trial to practice but fidelity to psychological treatment may be a challenge in routine practice. This may affect outcomes such that they may be inferior to that achieved in clinical trials [82].
Given the rising evidence base for guided selfhelp in mild to moderate depression [83], there is opportunity to make this available cheaply and with high fidelity.
Co-morbidity issues
Rise in life expectancy is increasing the burden of chronic illness and therefore the spectre of co-morbidity is growing [84]. Physical chronic conditions already have well established evidence based pathways for treatment however there is a glaring gap of guidelines where co-morbid chronic diseases are concerned [85].
Depression’s co-morbidity with anxiety can affect treatment outcomes [86]. However detection of anxiety may provide the scope to integrate evidence based psychological intervention like CBT early. The co-morbidity with alcohol and substance use can be problematic. The good news is that depression in co-morbid conditions also responds to standard treatment [87,88]. Co-morbidity with physical health problems is another concern as it has reciprocal effect on outcomes of both depression and physical health conditions as discussed earlier.
A systematic approach to target co-morbidity in depression is needed. The term systematic refers here to a health system priority, given that depression contributes highest to the burden of disability. Such an approach would require interconnection and liaison between services create to enhance the treatment of depression.
Post treatment issues
This is contradiction in terms as there is no post treatment phase for a long term condition. It is really a matter of continuity of treatment. In current practice maintenance antidepressants, routine follow ups and recognizing early warning signs is the best we have. There are many more options.
A systematic approach to management of the inter episode periods is largely missing in depression management even though there are interventions which have been researched. Mindfulness approaches can be used for relapse prevention. Since it is a group intervention, the cost is likely to be low. Early detection is critical and routine depression questionnaire with high sensitivity may be advantageous in identifying recurrence. Targeted booster CBT may also be considered and research into delivering this as low cost, easily disseminated guided self-help is sorely needed. Finally the key issue of antidepressant medication adherence must be addressed by a variety of means like patient and family education, telephone and text message reminders, self help programmes and connection to peer support groups. More research is needed to enhance adherence in long term conditions as a systematic review of interventions showed inconsistent effectiveness [89].
System issues
Long term condition management is -truly speaking –not just a clinical approach but also a systems approach. This requires an efficient network of relevant information which is easily accessible to inform decision making. Current patient health record systems are designed to replace paper notes or serve the purpose of governance and documentation as their primary goal. This needs to change. The primary goal of health care records should be to track clinical and functional outcomes such that management of those conditions is improved. Documentation, event monitoring, billing and scheduling are merely operations to achieve healthcare outcomes and not goals in themselves.
With specific reference to depression (and in fact most chronic conditions) the system must accommodate patient self-monitoring and tracking as this is key to detecting early relapse. Smart phone assisted technology is available to enhance chronic conditions management [90] but not yet integrated in healthcare systems. We already have technology delivered guided psychological treatments through such devices [91].
Recurrent depression registers which provide a unique code for healthcare management and communication may offer yet another way to track outcomes and provide treatment based on evidence based algorithm in primary care and specialist settings. This can also be combined with depression decision support systems to guide practitioners choose effective interventions.
Effective communication between healthcare providers especially with respect to critical health events changed the landscape of chronic disease management. A red flag approach for depression relapse is also feasible.
Summary
Major depression has high likelihood of being a recurrent condition and as such requires a long term strategy for management. Disability due to depression can also persist in the long term. Chronic conditions management has made large strides in the last decade and clinical trials of this approach in depression are also effective. Whilst pharmacological recommendation for treatment of depression adopts a more long term treatment approach, the public education on depression is focused on acute treatment. This has to change. Non adherence to medication is very high in depression and health services do not offer a systematic approach to symptom monitoring and medication adherence. Psychological treatments are beginning to focus on the longitudinal course of depression rather than immediate symptom reduction. This is good news. A systems approach involving use of current technology can offer very promising directions in long term management of depression.References
- (2013) Diagnostic and statistical manual of mental disorders 5th ed. Arlington, VA: American Psychiatric Association.
- Spence D (2013) Are antidepressants overprescribed? Yes. BMJ 346: f191.
- Mojtabai R (2013) Clinician-identified depression in community settings: concordance with structured-interview diagnoses. Psychother Psychosom 82: 161-169.
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, et al. (2005) Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 62: 593-602.
- Holma KM, Holma IA, Melartin TK, Rytsala HJ, Isometsa ET (2008) Long-term outcome of major depressive disorder in psychiatric patients is variable. J Clin Psychiatry 69: 196-205.
- Keller MB, Lavori PW, Mueller TI, Endicott J, Coryell W, et al. (1992) Time to recovery, chronicity, and levels of psychopathology in major depression. A 5-year prospective follow-up of 431 subjects. Arch Gen Psychiatry 49: 809-816.
- Judd LL (1997) The clinical course of unipolar major depressive disorders. Arch Gen Psychiatry 54: 989-991.
- Burcusa SL, Iacono WG (2007) Risk for recurrence in depression. Clin Psychol Rev 27: 959-985.
- Maj M, Veltro F, Pirozzi R, Lobrace S, Magliano L (1992) Pattern of recurrence of illness after recovery from an episode of major depression: a prospective study. Am J Psychiatry 149: 795-800.
- Geddes JR, Carney SM, Davies C, Furukawa TA, Kupfer DJ, et al. (2003) Relapse prevention with antidepressant drug treatment in depressive disorders: a systematic review. Lancet 361: 653-661.
- Hansen R, Gaynes B, Thieda P, Gartlehner G, Deveaugh-Geiss A, et al. (2008) Meta-analysis of major depressive disorder relapse and recurrence with second-generation antidepressants. Psychiatr Serv 59: 1121-1130.
- Kaymaz N, van Os J, Loonen AJ, Nolen WA (2008) Evidence that patients with single versus recurrent depressive episodes are differentially sensitive to treatment discontinuation: a meta-analysis of placebo-controlled randomized trials. J Clin Psychiatry 69: 1423-1436.
- Videbech P, Ravnkilde B (2004) Hippocampal volume and depression: a meta-analysis of MRI studies. Am J Psychiatry 161: 1957-1966.
- Huang CL (2009) Residual cognitive deficit in adults with depression who recovered after 6-month treatment: stable versus state-dependent markers. J Clin Med Res 1: 202-206.
- Behnken A, Schoning S, Gerss J, Konrad C, de Jong-Meyer R, et al. (2010) Persistent non-verbal memory impairment in remitted major depression - caused by encoding deficits? J Affect Disord 122: 144-148
- Paelecke-Habermann Y, Pohl J, Leplow B (2005) Attention and executive functions in remitted major depression patients. J Affect Disord 89: 125-135.
- Barr VJ, Robinson S, Marin-Link B, Underhill L, Dotts A, et al. (2003) The expanded Chronic Care Model: an integration of concepts and strategies from population health promotion and the Chronic Care Model. Hosp Q 7: 73-82.
- Scher CD, Ingram RE, Segal ZV (2005) Cognitive reactivity and vulnerability: empirical evaluation of construct activation and cognitive diatheses in unipolar depression. Clin Psychol Rev 25: 487-510.
- Judd LL, Akiskal HS, Maser JD, Zeller PJ, Endicott J, et al. (1998) A prospective 12-year study of subsyndromal and syndromal depressive symptoms in unipolar major depressive disorders. Arch Gen Psychiatry 55: 694-700.
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, et al. (2007) Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 370: 851-858.
- Katon W, Lin EH, Kroenke K (2007) The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen Hosp Psychiatry 29: 147-155.
- DiMatteo MR, Lepper HS, Croghan TW (2000) Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med 160: 2101-2107.
- Katon W, Lin EH, Kroenke K (2007) The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen Hosp Psychiatry 29: 147-155.
- Wagner G, Icks A, Albers B, Abholz HH (2012) Type 2 diabetes mellitus and depressive symptoms: what is the cause of what? A systematic literature review. Dtsch Med Wochenschr 137: 523-528.
- Lustman PJ, Anderson RJ, Freedland KE, de Groot M, Carney RM, et al. (2000) Depression and poor glycemic control: a meta-analytic review of the literature. Diabetes Care 23: 934-942.
- Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, et al. (2010) Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry 67: 220-229.
- Pan A, Keum N, Okereke OI, Sun Q, Kivimaki M, et al. (2012) Bidirectional association between depression and metabolic syndrome: a systematic review and meta-analysis of epidemiological studies. Diabetes Care 35: 1171-1180.
- Chaiton MO, Cohen JE, O'Loughlin J, Rehm J (2009) A systematic review of longitudinal studies on the association between depression and smoking in adolescents. BMC Public Health 9: 356.
- Taylor G, McNeill A, Girling A, Farley A, Lindson-Hawley N, et al. (2014) Change in mental health after smoking cessation: systematic review and meta-analysis. BMJ 348: g1151.
- Van der Kooy K, van Hout H, Marwijk H, Marten H, Stehouwer C, et al. (2007) Depression and the risk for cardiovascular diseases: systematic review and meta analysis. Int J Geriatr Psychiatry 22: 613-626.
- Meijer A, Conradi HJ, Bos EH, Anselmino M, Carney RM, et al. (2013) Adjusted prognostic association of depression following myocardial infarction with mortality and cardiovascular events: individual patient data meta-analysis. Br J Psychiatry 203: 90-102.
- Meijer A, Conradi HJ, Bos EH, Thombs BD, van Melle JP, et al. (2011) Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis of 25 years of research. Gen Hosp Psychiatry 33: 203-216.
- Cuijpers P, Vogelzangs N, Twisk J, Kleiboer A, Li J, et al. (2014) Comprehensive meta-analysis of excess mortality in depression in the general community versus patients with specific illnesses. American J Psychiatry.
- Hornikx M, Van Remoortel H, Demeyer H, Marcal Camillo CA, Decramer M, et al. (2013) The influence of comorbidities on outcomes of pulmonary rehabilitation programs in patients with COPD: a systematic review. BioMed Res Int 2013: 146148.
- Howren MB, Lamkin DM, Suls J (2009) Associations of depression with C-reactive protein, IL-1, and IL-6: a meta-analysis. Psychosom Med 71: 171-186.
- Na KS, Lee KJ, Lee JS, Cho YS, Jung HY (2014) Efficacy of adjunctive celecoxib treatment for patients with major depressive disorder: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry 48: 79-85.
- WHO (2011) Health statistics and health information systems: Regional estimates for 2000-2011-Disease Burden Geneva: World Health Organisation.
- Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, et al. (2013) Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med 10: e1001547.
- Lam RW, Filteau MJ, Milev R (2011) Clinical effectiveness: the importance of psychosocial functioning outcomes. J Affect Disord 132: S9-S13.
- Buist-Bouwman MA, Ormel J, de Graaf R, Vollebergh WA (2004) Functioning after a major depressive episode: complete or incomplete recovery? J Affect Disord 82: 363-371.
- Rhebergen D, Beekman AT, de Graaf R, Nolen WA, Spijker J, et al. (2010) Trajectories of recovery of social and physical functioning in major depression, dysthymic disorder and double depression: a 3-year follow-up. J Affect Disord 124: 148-156.
- Uher R, McGuffin P (2008) Genetics of Mental Ill-health in Children and Adults and Interaction of Genes with Social Factors. London, UK: The FORESIGHT Institute.
- Almgren P, Lehtovirta M, Isomaa B, Sarelin L, Taskinen MR, et al. (2011) Heritability and familiality of type 2 diabetes and related quantitative traits in the Botnia Study. Diabetologia 54: 2811-2819.
- Gilman SE, Trinh NH, Smoller JW, Fava M, Murphy JM, et al. (2013) Psychosocial stressors and the prognosis of major depression: a test of Axis IV. Psychol Med 43: 303-316.
- Brown GW, Harris TO, Kendrick T, Chatwin J, Craig TK, et al. (2010) Antidepressants, social adversity and outcome of depression in general practice. J Affect Disord 121: 239-246.
- Angst J, Gamma A, Rossler W, Ajdacic V, Klein DN (2011) Childhood adversity and chronicity of mood disorders. Eur Arch Psychiatry Clin Neurosci 261: 21-27.
- Mead N, Lester H, Chew-Graham C, Gask L, Bower P (2010) Effects of befriending on depressive symptoms and distress: systematic review and meta-analysis. Br J Psychiatry 196: 96-101.
- Harris T, Brown GW, Robinson R (1999) Befriending as an intervention for chronic depression among women in an inner city. 1: Randomised controlled trial. Br J Psychiatry 174: 219-224.
- Lam RW, Kennedy SH, Grigoriadis S, McIntyre RS, Milev R, et al. (2009) Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults. III. Pharmacotherapy. J Affect Disord 117: S26-S43.
- APA (2010) Practice guideline for the treatment of patients with major depressive disorder, 3rd ed. Arlington (VA): American Psychiatric Association (APA) pp: 152.
- Butler AC, Chapman JE, Forman EM, Beck AT (2006) The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clin Psychol Rev 26: 17-31.
- Cuijpers P, Geraedts AS, van Oppen P, Andersson G, Markowitz JC, et al. (2011) Interpersonal psychotherapy for depression: a meta-analysis. Am J Psychiatry 168: 581-592.
- Cuijpers P, van Straten A, Warmerdam L (2007) Behavioral activation treatments of depression: a meta-analysis. Clin Psychol Rev 27: 318-326.
- Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, et al. (2006) Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. J Consult Clin Psychol 74: 658-670.
- Moradveisi L, Huibers MJ, Renner F, Arasteh M, Arntz A (2013) Behavioural activation v. antidepressant medication for treating depression in Iran: randomised trial. Br J Psychiatry 202: 204-211.
- Vittengl JR, Clark LA, Dunn TW, Jarrett RB (2007) Reducing relapse and recurrence in unipolar depression: a comparative meta-analysis of cognitive-behavioral therapy's effects. J Consult Clin Psychol 75: 475-488.
- Dobson KS, Hollon SD, Dimidjian S, Schmaling KB, Kohlenberg RJ, et al. (2008) Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the prevention of relapse and recurrence in major depression. J Consult Clin Psychol 76: 468-477.
- Beshai S, Dobson KS, Bockting CL, Quigley L (2011) Relapse and recurrence prevention in depression: current research and future prospects. Clin Psychol Rev 31: 1349-1360.
- Chiesa A, Serretti A (2011) Mindfulness based cognitive therapy for psychiatric disorders: a systematic review and meta-analysis. Psychiatry Res 187: 441-453.
- Segal ZV, Bieling P, Young T, MacQueen G, Cooke R, et al. (2010) Antidepressant monotherapy vs sequential pharmacotherapy and mindfulness-based cognitive therapy, or placebo, for relapse prophylaxis in recurrent depression. Arch Gen Psychiatry 67: 1256-1264.
- (2014) Depression Treatment: Black Dog Institute.
- NIMH (2014) Depression: National Institute of Mental Health.
- Sansone RA, Sansone LA (2012) Antidepressant adherence: are patients taking their medications? Innov Clin Neurosci 9: 41-46.
- Fischer MA, Stedman MR, Lii J, Vogeli C, Shrank WH, et al. (2010) Primary medication non-adherence: analysis of 195,930 electronic prescriptions. J Gen Intern Med 25: 284-290.
- Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, et al. (2001) Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 20: 64-78.
- Brady TJ, Murphy L, O'Colmain BJ, Beauchesne D, Daniels B, et al. (2013) A meta-analysis of health status, health behaviors, and healthcare utilization outcomes of the Chronic Disease Self-Management Program. Prev Chronic Dis 10: 120112.
- Epping-Jordan JE, Pruitt SD, Bengoa R, Wagner EH (2004) Improving the quality of health care for chronic conditions. Qual Saf Health Care 13: 299-305.
- Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ (2006) Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med 166: 2314-2321.
- Bower P, Gilbody S, Richards D, Fletcher J, Sutton A (2006) Collaborative care for depression in primary care. Making sense of a complex intervention: systematic review and meta-regression. Br J Psychiatry 189: 484-493.
- Neumeyer-Gromen A, Lampert T, Stark K, Kallischnigg G (2004) Disease management programs for depression: a systematic review and meta-analysis of randomized controlled trials. Med Care 42: 1211-1221.
- Katon WJ, Seelig M (2008) Population-based care of depression: team care approaches to improving outcomes. J Occup Environ Med 50: 459-467.
- Cooney GM, Dwan K, Greig CA, Lawlor DA, Rimer J, et al. (2013) Exercise for depression. Cochrane Database Syst Rev 9: CD004366.
- Salmon P (2001) Effects of physical exercise on anxiety, depression, and sensitivity to stress: a unifying theory. Clin Psychol Rev 21: 33-61.
- Uher R, Payne JL, Pavlova B, Perlis RH (2013) Major depressive disorder in dsm-5: implications for clinical practice and research of changes from DSM-IV. Depress Anxiety [Epub ahead of print].
- Kroenke K, Spitzer RL, Williams JB (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16: 606-613.
- Inoue T, Tanaka T, Nakagawa S, Nakato Y, Kameyama R, et al. (2012) Utility and limitations of PHQ-9 in a clinic specializing in psychiatric care. BMC psychiatry 12: 73.
- Bland RC, Streiner DL (2013) Why screening for depression in primary care is impractical. CMAJ 185: 753-754.
- Gilbody S, Sheldon T, House A (2008) Screening and case-finding instruments for depression: a meta-analysis. CMAJ 178: 997-1003.
- Huynh NN, McIntyre RS (2008) What are the implications of the STAR*D trial for primary care? A review and synthesis. Prim Care Companion J Clin Psychiatry 10: 91-96.
- Keller MB, McCullough JP, Klein DN, Arnow B, Dunner DL, et al. (2000) A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression. N Eng J Med 342: 1462-1470.
- Judd LL, Schettler PJ, Akiskal HS (2002) The prevalence, clinical relevance, and public health significance of subthreshold depressions. Psychiatr Clin North Am 25: 685-698.
- Shafran R, Clark DM, Fairburn CG, Arntz A, Barlow D, et al. (2009) Mind the gap: Improving the dissemination of CBT. Behav Res Ther 47: 902-909.
- National Collaborating Centre for Mental Health (UK) (2010) Depression: The treatment and management of depression in adults (updated edition) London, UK: National Institute of Clinical Excellance, England, CG90.
- Manton KG (1988) The global impact of noncommunicable diseases: estimates and projections. World Health Stat Q 41: 255-266.
- Lugtenberg M, Burgers JS, Clancy C, Westert GP, Schneider EC (2011) Current guidelines have limited applicability to patients with comorbid conditions: a systematic analysis of evidence-based guidelines. PloS One 6: e25987.
- Fava M, Rush AJ, Alpert JE, Balasubramani GK, Wisniewski SR, et al. (2008) Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report. Am J Psychiatry 165: 342-351.
- Davis LL, Wisniewski SR, Howland RH, Trivedi MH, Husain MM, et al. (2010) Does comorbid substance use disorder impair recovery from major depression with SSRI treatment? An analysis of the STAR*D level one treatment outcomes. Drug Alcohol Depend 107: 161-170.
- Lejoyeux M, Lehert P (2011) Alcohol-use disorders and depression: results from individual patient data meta-analysis of the acamprosate-controlled studies. Alcohol Alcohol 46: 61-67.
- Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X (2008) Interventions for enhancing medication adherence. Cochrane Database Syst Rev CD000011.
- Boulos MN, Wheeler S, Tavares C, Jones R (2011) How smartphones are changing the face of mobile and participatory healthcare: an overview, with example from eCAALYX. Biomed Eng Online 10: 24.
- Ly KH, Carlbring P, Andersson G (2012) Behavioral activation-based guided self-help treatment administered through a smartphone application: study protocol for a randomized controlled trial. Trials 13: 62.
So what might be the