Journal of Neurology and Psychology
Download PDF
Review Article
Diabetes is a Complex Neurological, Multisystemic, Multipathological and Polygenomic Disorder: the Use of Strannik Software as an Effective Modality to Illustrate Its Complexity
Ewing GW1* and Parvez SH2
1Mimex Montague Healthcare Limited, Nottingham, UK
2Head of the CNRS Neuroendocrine Unit, Paris
*Address for Correspondence: Ewing GW, Mimex Montague Healthcare Limited, Mulberry House, 6 Vine Farm Close, Cotgrave, Nottingham NG12 3TU, UK; E-mail:
graham.ewing@mmhcl.co.uk
Submission: April 11, 2019;
Accepted: June 03, 2019;
Published: June 05, 2019
Copyright: © 2019 Ewing GW, et al. This is an open access article
distributed under the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited.
Abstract
This paper illustrates that the brain is a biophysical entity in
which both sensory and biological input sustain its biophysical and
computational function. This leads to the conclusion that the brain
works in a multi-level and coherent manner to optimise and/or
regulate the body’s multi-systemic stability and function.
It further illustrates that the ‘optimisation of blood glucose levels’
exhibits the characteristics of a neurally regulated physiological system
in which blood glucose levels are regulated between higher and lower
limits i.e. 4-8 mmol/l blood glucose; that types 1 and 2 diabetes are
comorbidities thereby explaining the inaccuracies reported when
diagnosing diabetes; that under pathological conditions mainly in the
pancreas, but also as a result of pathological onset in adjacent organs
and systems, there is an imbalance between insulin expression and
insulin reactivity which leads to increased or decreased blood glucose
levels, elevated blood viscosity, the onset of free radical reactions,
the subsequent production of complex glycated proteins/lipids and
metabolites, altered colour perception.
Moreover such precise knowledge; which is embodied in
Grakov’s mathematical model of the relationship between sense
perception, brain function, the autonomic nervous system and
physiological systems, and pathological onset; can be applied to
screen the patient’s health (as Strannik Virtual Scanning) and/or as a
neuro modulation type technique (as Strannik Light Therapy) to treat
autonomic dysfunction and the range of comorbidities experienced
by diabetic and obese patients.
Keywords
Strannik; Strannik Virtual Scanning; Strannik Light Therapy;
Autonomic nervous system; Physiological systems; Blood glucose; Diabetes
Abbreviations
SVS: Strannik Virtual Scanning; SLT: Strannik Light Therapy;
LTP: Long Term Potentiation; HGH: Human Growth Hormone;
GABA: Gamma Amino Butyric Acid; CBT: Cognitive Behavioural
Therapy; NLP: Neurolinguistic Programming; IRP2: Insulin Receptor
Protein2; GP: General Practitioner; LGN: Lateral Geniculate Nucleus
Introduction
This paper sets out to provide a coherent explanation for the
phenomena of unstable blood glucose levels taking into account the
complexity of psychological and physiological phenomena which
accompany ‘Diabetes Mellitus’. It considers the influence of sensory
Our relationship with our environment and how we respond to sensory input:
The human is a creature of habit. We can be influenced to do
things and adopt patterns of behaviour which alter and/or simplify
the complexity of our lives e.g. what we eat and drink, how we eat
and drink, where we eat and drink, with whom we eat and drink, how
much we eat and drink, etc.Through our senses we are predisposed to favour particular
experiences, foods, music and fashions often involving colour(s) e.g.
a deep shade of red is known to stimulate appetite and is occasionally
painted on the walls of a savvy restaurant whilst a pastel shade of
green slows heartbeat and is occasionally to be found on the walls of
a cardiac ward in hospital; however our sense perception and colour
preferences change with pathological onset e.g. the onset of diabetes
is accompanied by changes of blue-yellow colour perception.
We are subject to the complex influences of industries which,
through advertising programmes, seek to persuade us to alter our
patterns of behaviour, and hence purchase the products which they
produce, manufacture and sell e.g. red or white meat, acidified and/
or alcoholic beverages, processed foods including sugars and oils,
cereals and carbohydrates, etc.
We make decisions, which are not based upon fact because we
simply do not have the time to examine facts but instead upon our
perception of the facts and how we are expected to behave i.e. whether
we perceive that it is the appropriate thing to do; and we are guided
by the complex opinions which we have built up throughout our lives and which are based upon what we have seen, read, viewed, heard
and/or discussed with our peers. Our sensory experiences sculpt
our neural connectivity and multilevel function by mechanisms,
memories and opinions, which are still to be fully understood or
defined e.g. whether rational or emotional, which are influenced by
the autonomic nervous system. As a result, we are almost powerless
to make a choice in our lives which has not been shaped by vested
interests yet every aspect of the body’s function and our behaviour
is fundamentally biochemical i.e. our physiology, and how the
brain influences, and/or is influenced by, the viscera; is influenced
at different levels, in particular at the psychosomatic level, which
influences our conscious thought patterns; and at the somatic level
which influences our subconscious thought patterns, processes and
mechanisms.
Somehow our psychosomatic and somatic function is the product
of a precise and sophisticated biological and structural relationship,
which includes the reaction kinetics at the molecular level, however
there is not yet a clear accepted understanding of this relationship.
Indeed, such is the complexity of this subject that it has perplexed the
leading minds of our time e.g. Kandel, Brenner, Noble, and others;
who have sought in their published works to explain the fundamental
mechanisms by which the body is organised and regulated [1].
The process of physiological adaptation to our environment:
The sub-division of most medical research into sub-units,
known as reductionism, ensures that there is not any significant
research into the fundamental whole-body mechanisms by which
the body functions and is regulated. Most medical research is not
intended to develop an understanding of how the body functions
but instead to develop techniques which have commercial potential
whereas a precise understanding of how the body functions e.g.
a neurosimulation technique, would conceivably reduce the
complexity and cost of healthcare. Nevertheless there are several
research areas which are devoted to such an approach e.g. neurology
and neuroscience, psychology, sports physiology, systems biology
[2], complementary and alternative medicine, biofeedback/
neurofeedback/neuromodulation.Consider how humans live in different climates, at different
altitudes, and in different environments. Those who live at altitude,
in the Andes or Tibet, have higher levels of red blood cells in order
to transport oxygen around the body, or create more energy using
less oxygen, or have widened blood vessels which improve blood
flow. Those who live in extremely cold regions, the Inuit, have a
diet which is high in meat and fat which enables them to better deal
with low temperatures and, in South-East Asia, the Bajau are able
to dive to the seabed because their bodies produce higher levels of
hemoglobin i.e. there is a neurological mechanism which assesses the
physiological response to environmental parameters, to which the
body is exposed, alters the genetic expression of hemoglobin, and,
through its relationship with long-term memory, enables the body
to adapt to its environment. This is significant because the brain
receives biochemical input from the visceral organs and continuously
regulates the body’s physiological parameters in order to optimize its
systemic stability by continuously adjusting the various metabolic
processes which are involved in the regulation of metabolic rate
and hence maintain a suitable environment in which the brain can function effectively.
Claude Bernard considered that the internal environment of
organism is constant with the existence of control processes to achieve
such ‘homeostasis’ and envisaged future mathematical modeling and/
or neurosimulation simulation applications [3]. Moreover, the body
is such a highly regulated entity that the possibility of mathematical
modeling its function appears to be plausible i.e. if the complex nature
and structure of its function were to be understood.
Every medical condition, without exception, comprises a range of
pathologies which can be defined in terms of its genotype i.e. the rate
at which the genes express particular protein(s); and its phenotype i.e.
the rate at which the expressed protein(s) react with their substrates
which is influenced by stress. In the case of diabetes and obesity this
has overcome our ability to live and sustain a healthy life with the
result that longevity is now declining in the most wealthy economies
[4], fertility throughout the world is in decline [5], and expenditure
on healthcare throughout the world continues to increase i.e. the GP
and their patients needs to be educated in order to make the choices
which enable us to live long, healthy and happy lives.
Accordingly, the aim of this article is to summarise the complex
range of factors which influence the occurrence of diabetes and
diabetic comorbidities and to further elucidate the complex
neurological origins of such conditions.
A Review of The evidence-base Regarding Calorific Intake and Energy Expenditure
Regarding diabetes and obesity, the healthcare professions are in
agreement that the body regulates its calorific intake i.e. if we consume
more energy (via food and drink) than we expend (via exercise) our
weight will increase. There are numerous examples which support
this general and eminently logical conclusion e.g.
• The quantity of food portions is significant -: if we place large
portions on our plate there is an imperative to eat the full allocation
[6]. The Japanese often use the term ‘Hari Hachi Bu’ to direct and/or
advise that we should eat until we are just 80% full.
• How we serve the food is significant -: it influences the rate
at which we digest the food e.g. an emulsified or blended soup is
digested more slowly than an unblended soup [7].
• How we eat the food is significant -: if we eat a calorie-rich meal
in a short period, and/or whether the meal is accompanied by an
acidified or alcoholic beverage [8] - which influences the availability
of essential minerals which are stored in the body, in particular
Mg, Ca and Zn which are often essential catalysts in metabolically
significant processes [8].
• Who we are is significant -: e.g. our genes and or gender/whether
male or female and/or our racial origins [8,9]; whether young or old;
and/or our exposure to gene-altering moieties e.g. viruses and viruslike
particles [10,11]; and/or our exposure to acidity [12-14].
The observation that the genetic profile which is required to
express insulin can differ between racial groups with differing genetic
profiles illustrates that diabetes is a polygenomic indication i.e. that
gene conformation is a more significant factor than the chemical
nature and/or structure of the gene(s) [10].
• How much we consume is significant -: someone who has
an energy intense job/elevated metabolic rate requires greater
sustenance than someone who has a sedentary lifestyle e.g. a
computer programmer, social media consultant, etc. In general, if we
consume more calories than we expend through physical activity and/
or elevated metabolic rate; then our weight will increase [15]. (An
additional ca. 3500 calories leads to ca. 500 grams increased weight
i.e. a standard 51 gram branded snack bar each day can be expected to
increase your weight by up to ca. 1 kg each month).
• What we eat and drink is significant -: if we drink water, or
acidified, alcoholic or caffeinated beverages with a snack or meal [16].
• Diets must include fats -: because some vitamins are fatsoluble
whilst others are water-soluble. Fats and carbohydrates are
both metabolised into energy, by different metabolic processes, and
have different diabetic significance e.g. that a balanced fat/carb diet
(avoidance of high fat and/or high carb diets) is often appropriate in
dietary control [17-19].
• The taste of our food is significant -: the merest thought of
food is often sufficient to make us salivate and produce enzymes
required for early mastication/digestion whilst the taste buds detect
the sweet tastes from foods containing glucose and/or other sugars
and stimulate the neurological process by which the brain initiates the
supply of insulin [20,21].
• The calorie loading of our food is significant -: whether we
consume large quantities of ‘carbs’ e.g. pasta, potatoes, rice, bread,
etc; or whether we consume a vegetarian, vegan or Mediterranean
diet. Large amounts of carbs increase the required levels of insulin
- the body fluctuates between hyperglycaemia and hypoglycaemia -
therefore a balanced diet should include foods which are slower to
digest, require lower levels of insulin, and stabilise blood glucose
levels over longer periods [22].
• Foods which are difficult to digest often require greater levels of digestive acidity.: The production of elevated levels of
digestive acidity may exceed the combined ability of the pancreas and
duodenum to neutralise excess acidity with the result that pH in the
intestines cannot be maintained at indicatively pH 6.5-7.0 and leads
to pathological onset in the digestive tract, altered levels of intestinal
flora, etc [23].
• Where we eat is significant -: if we eat in a fast food outlet we are
likely to eat more rapidly - the calorific load is consumed in a short
period - the consequence being greater fluctuations in insulin and
blood glucose levels i.e. hyperglycaemia followed by hypoglycaemia
[24]; whereas if we eat more slowly, perhaps over an extended period
the relative calorific load is less (the Mediterranean diet). Intriguingly
the colour red, perhaps on the walls of a good restaurant, has been
shown to stimulate appetite.
• Where and how we live is significant -: our exposure to light
stimulates the pituitary gland which in turn stimulates the thyroid
gland and hence influences our metabolic rate; through the pineal
gland the levels of ROS scavengers, the antioxidants melatonin and
serotonin; and via the skin the level of cholecalciferol (vitamin D3)
which influences immune function i.e. exposure to natural sunlight
is essential.
• When we eat is significant -: the body requires a stable series of
mealtimes - typically breakfast, lunch and an evening meal. Eating
carb. rich meals later in the evenings, elevates blood glucose levels,
alters predisposition to sleep and/or the onset and duration of sleep,
and is invariably accompanied by increased weight [25].
• If we sleep later -: (night-owls and/or parents of newborns) or
do not enough good quality sleep it becomes harder to regulate body
weight [26,27].
• Where we sleep is significant -: if our bed is uncomfortable or if
we have issues which prevent is getting good quality sleep e.g. having
hearing problems perhaps from living alongside a noisy road, having
a nasal infection or problem, having a spinal problem.
• If we develop problems in the sexual organs perhaps as a result of a hysterectomy to treat endometriosis -: the body is increasingly
unable to regulate blood glucose levels (non-pancreatic diabetes) [28].
• What and how we exercise -: exercise elevates metabolic rate
and hence our ability to metabolise surplus weight [29,30].
……….and to illustrate the somatic consequences of varying
degrees of hyper indulgence:
• Why do we engage in hyper indulgent behaviour?- eating and
drinking too much of the wrong things over a short/long period
expands the volume of the stomach and digestive tract [31]; and
which, at its extreme, requires corrective bariatric surgery.
• How we regulate our weight by dietary means following periods of weight-gain ?: [31,32] - it takes time for the body to adjust
to lower levels of food intake and adjust to a lower weight.
Nevertheless, despite the immense body of experiential medical
research, there is not yet an accepted recognition of how this plethora
of psychosomatic factors influences the body’s stable function i.e.
at the somatic level; however that the human body is an intensely
regulated organism is not in dispute. Every second in every day for
ca 70-80 years throughout our lives; from birth throughout our many
and various developmental phases until our death; there is a neural
mechanism which continuously receives sensory and biological
data; which regulates body temperature, the circulation of blood,
breathing and/or the supply of oxygen to the brain, blood pressure,
blood glucose, intercellular and digestive pH, digestion, elimination
of toxins and wastes, and all other essential physiological functions.
Cognitive changes, in particular of sense perception have
pathological origins. Perhaps the most convincing explanation to
date has been incorporated in the Strannik technology, which is
based upon the first mathematical model of the relationship between
sense perception, brain function, the autonomic nervous system and
physiological systems [16,33-36], and pathological onset; and how
this can be applied to screen (as Strannik Virtual Scanning) diabetes
and a broad range of other indications [31,40,41], and/or treat (as
the neuro modulation technique Strannik Light Therapy (SLT)) their
autonomic dysfunction [37-41].
The Body is continuously regulated and Functions at Different Levels of Physiological Significance
Our ability to express proteins and other biologically significant moieties declines as we age. By the time we are 75 years we express
as little as 10% of the insulin which we expressed when we were in
our prime but we do not drop dead. It is only when our demand for
insulin exceeds the supply and/or reactivity of insulin (and/or other
physiologically significant proteins) that there is a problem i.e. the
genetic expression of insulin declines to the extent that it is unable to
sustain the required demand for insulin. This illustrates the existence
of a multi-level mechanism, acting at the psychosomatic and somatic
levels, which continuously regulates and adjusts the stable and
coherent function of the autonomic nervous system, physiological
systems and ultimately cellular and molecular biology.
The evidence suggests the involvement of the neuro sensory
pathways, the brain, neural networks and vagus nerve in the body’s
function e.g. (i) the role of neural networks in memory and learning
[42,43], in diabetes [44-46]; (ii) the effect of stimulating the vagus
nerve as a way of regulating blood glucose levels and (iii) that
the magnitude and/or longevity of exposure to a psychological/
psychosomatic or somatic factor(s) influences the body’s function at
different levels of physiological significance i.e. the brain functions in
some ways as a parallel processor e.g. the communication between
the two halves of the brain which appears to influence our emotional
intelligence [47-49]; and in other cases as a serial processor in which
the brain functions at different levels of physiological significance,
perhaps enabling much greater serial processing when freed from
the constraints imposed by emotional processing [50]. Nevertheless,
there is not yet a consensus of opinion re what the brain does and
how it does it.
The physiological significance of the brain-wave states:
The brain-wave states are recognised to be physiologically
significant i.e. the magnitude and/or longevity of exposure to stress
has neurological and visceral significance. The gamma state (ca. 30-
60hz) is associated with subliminal imaging i.e. sensory perception of
our environment [51]; the beta state (ca. 15-30 hz) is associated with
physical activity and/or movement and/or function [52,53]; the alpha
state (ca. 8-15 hz) is associated with sensory input and/or associative
thought [54]; however there are no precedents which illustrate that
these brain wave states function independently i.e. independently
of each other or independently of the theta and delta states which
function throughout each 24 hour cycle. The only exception is that in
cases of severe trauma (coma) the brain will shut down most, if not
all, brain wave activity with the exception of the delta state i.e. the
different EEG frequency states are an interdependent and essential
element of the body’s function [55]. Moreover biochemical changes
e.g. resulting from the administration of pharmacological substances,
alters the EEG states [56]. This illustrates the existence of a dynamic
biophysical relationship which involves the brain’s biology, its
function, and/or the prevailing brainwave (EEG) state(s) e.g. if
we give a stimulant (caffeine, nicotine or adrenaline) or a sedative
(ethyl alcohol).The gamma, beta and alpha states characterise the
psychosomatic state whereas the theta and delta states characterise
the somatic subconscious state. Moreover there are no precedents of
the brain functioning independently of the body in the absence of
the delta state. Accordingly what is the significance of the somatic
state and how is this significant re the diagnosis and/or treatment of
diabetes?The Influence and significance of sleep:
The delta oscillations, without which the body cannot function,
are particularly associated with the function of the autonomic nervous
system. The evidence indicates that the delta (ca. 1-4 hz) and theta
states (ca. 4-8 hz) are implicated in the physiological mechanisms
which are linked to the body’s health, function, stability and survival
e.g. during sleep the majority of time is spent in the delta state and
hence is associated with the body’s complex reparative and regulatory
mechanisms [57].‘Sleeping is the second (after being awake) state of active life.
Accounting for the information which is absorbed during the day;
preparation of the controlling programme for the next day; checkup
of the condition of organs and tissues; correction of controlling
signals’ Grakov IG.
Lack of sleep is associated with declining health [58] and
pathological onset e.g. of diabetes and obesity, and with poorer
fixation and recall of memories thereby implicating the hippocampus
and processes such as Long-Term Potentiation (LTP) which is
associated with fixation of memories [59,60]. This indicates that
sleep performs a physiological significant role and that particular
sleep phases are associated with the transfer of memories from the
hippocampus to the cerebral cortex i.e. from short term memory to
long-term memory, elimination of neurotoxins which is supported
by the observation that the brain shrinks during sleep [61,62], the
production of HGH; the balance of melatonin and serotonin by
the pineal gland; levels of the primary neurotransmitters e.g. gaba,
N-acetyl Choline, Nor-epinephrine, dopamine; and the many and
various secondary neurotransmitters e.g. beta-endorphin, peptides,
secretins, gaseous signalling molecules, amino-acids, etc.
Sleep exhibits the characteristics of a neurally regulated
physiological system [63]. Emergent pathologies in any of the organs
in this system, and often in adjacent systems, influences the quality and
quantity of sleep e.g. in the endocrine glands, spinal cord, ears, nose,
etc. It is characterised by the terms hyper and hypo e.g. hypersomnia
and/or hyposomnia. There is no other way of explaining why the
brain has such immense computing power other than to consider
that the brain functions as a neuro modulator which continuously
emits and receives sensory and biological datahowever this does not
yet define the precise significance of the theta state which appear to
be associated with pain and fixation of memories (LTP) [64], perhaps
as a limiter of extreme function detecting cellular changes prior
to failure.Lack of sleep is accompanied by an increase in levels of
neurotoxins which influence the prevailing brain wave state(s) and
lead to pathological onset [65].
Further reflections upon the body’s multi-level function:
The gamma and beta states are associated with the most basic
experience - perceiving our environment, the alpha state is associated
with the accumulation of memories i.e. of thought or imagination,
the theta state is associated with physiological or psychological ‘pain’
i.e. limits of behaviour/cellular damage which is the most significant
learning state, and the delta state is associated with cellular/organ
damage and/or repair and/or physiological regulation.Consider how someone responds with greater urgency to different, an irritated instruction, an
angry instruction perhaps accompanied by an elevated punishment
e.g. a smack, and an explosion of anger and physical punishment
e.g. tissue damage or even a broken bone. The significance and/or
retention of the memory increases with the degree of the stimulus.
The stress experienced at such levels of stimuli influences our ability
to concentrate and memory, whilst the memory of physical damage
e.g. of a broken leg, is never erased.
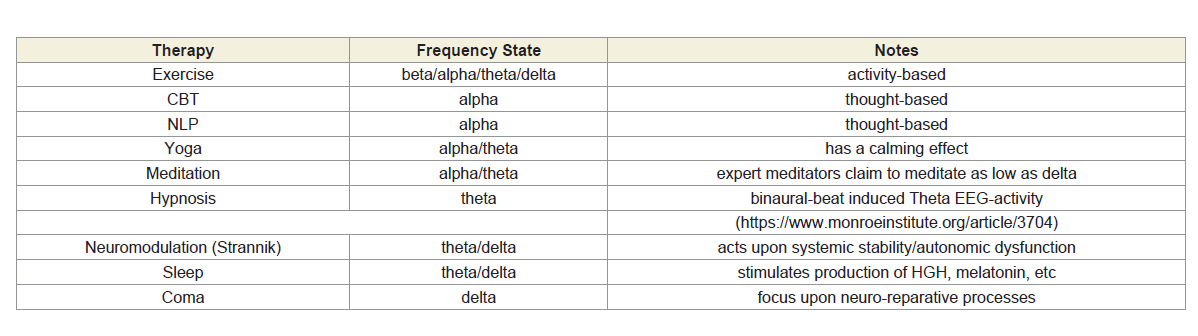
The issues can be illustrated by comparison with therapies (note
1) and/or neurological states and/or precedents e.g. CBT, NLP, yoga,
meditation, sleep, coma (Table 1). Cognitive therapies influence
thought patterns at the cognitive level but have little or no direct
effect upon the subconscious somatic levels, however therapies and
techniques which influence at the deepest somatic level, the delta state,
also influence at the psychosomatic level and have a calming, relaxing
effect upon behaviour whilst lack of sleep leads to increasingly manic
behaviour [66-68].
The delta and theta states are the dominant neurological states.
Traumatic events of varying magnitude or longevity, increased
weight and advancing age, influence the stable and coherent function
of the autonomic nervous system which influences organ function
and is accompanied by changes of cellular and molecular biology e.g.
• Why someone who experiences severe trauma e.g. a
bereavement, divorce, or work-related stress, experiences a range
of pathological ‘symptoms’ e.g. heart conditions, aches and pains,
migraine/headaches, digestive complaints/ulcerative conditions, etc.
The stress is the cause whilst the range of emergent pathologies are
the consequences of the problem and often decline when the patient
comes to terms with their trauma;
• Why someone who eats and drinks too much of the wrong
things becomes diabetic and/or obese e.g. alcoholic [69], acidic [70-72] beverages. The cause of their condition is that they eat and drink
too much of the wrong things, for psychosomatic and/or somatic
reasons, whilst the resulting diabetes and/or obesity (and the level of
HbA1c, blood glucose, etc) is the consequence;
• Stress leads to autonomic dysfunction which leads to changes of
molecular and cellular biology, organ biology, the stable and coherent
function of the physiological systems, and the process by which the
brain regulates and is influenced by changes of autonomic stability;
• But also that blood glucose is a neurally regulated physiological
system in which the brain regulates the coherent function of a network
of organs with the specific purpose of regulating blood glucose level(s) within optimum limits [73], typically between 4-8mmol/litre;
• and how changes of molecular biology influence the function
of the brain and subsequent behaviours e.g. how anti-depressive
medication influences brain biology and function [74].
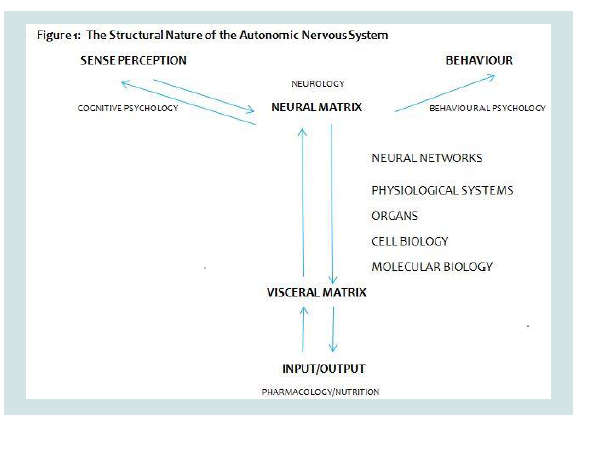
Figure 1 illustrates how biological input, received through the
visceral organs, influences the function of the brain which in turn
influences the stable and coherent function of the neural networks,
physiological systems, organs, and cellular and molecular biology;
how sensory input e.g. as stress, alters this dynamic relationship
leading to pathological onset (genotype and phenotype) and
behavioural change; and how pathological onset leads to changes of
sense perception.
This bidirectional flow of ‘data’ is particularly evident in the
diabetic in whom the hypothalamus activates multiple pathways e.g.
how levels of leptin (Figure 1) [75-77], insulin, fatty acids, and ghrelin,
influence feelings of appetite, hunger, and satiety; and it illustrates
how someone prescribed psychotropic medication will often gain
weight. The genetic expression of pre-pro-insulin, pro-insulin and
insulin (type 1 diabetes) in the pancreas influences brain function and
how we experience hunger yet the availability and, in particular, the
reactivity of insulin is influenced by how the brain manages the stress
response. The elevated levels of acidity arising from exposure to stress
(Note 2) influences the rate at which insulin reacts with its reactive
substrate IRP2 (insulin resistance), the subsequent entrance of blood
glucose into the cell, and its conversion into energy.
Accordingly the therapeutic application of specific EEG states
[78] - as brainwave entrainment, brainwave coherence, neuro
modulation, neuro feedback or biofeedback, and/or vagal nerve
stimulation - has the potential to modulate brain function and hence
improve or recover the stable and coherent function of the autonomic
nervous system, physiological systems, organs, etc.
The influence of sensory and biological input upon brain function and the medical syndrome diabetes mellitus:
The brain receives visual input via the retina (rods and cones)
and optic nerve which transmits visual information to the brain,
in particular to the Lateral Geniculate Nucleus (LGN), and to the
visual cortex in the occipital region at the rear of the brain. It also
transmits information to other thalamic brain regions including the
pretectal nucleus, midbrain nuclei and suprachiasmatic nucleus;
however altered biochemistry(s) e.g. due to the application of drugs
applied to the eye to treat glaucoma and of many medical conditions;
are associated with changes of colour perception. This indicates the presence of a biological/pathological mechanism which alters colour
perception. In addition the brain receives sensory input via the
sensory organs e.g. via the retina, which influences the magnocellular
and parvocellular pathways in the LGN (widely researched in dyslexia
[79-81]) and which has pathological origins [81]. This receipt
of sensory data via the amygdala [82,83], converts stress into its
pathological coordinates; via the hippocampus influencing regulation
of the autonomic nervous system and short-term memory; and the
hypothalamus before forwarding information to the cerebral cortex
(Note 3).
Figure 1: Illustrates how biological input, received through the visceral
organs, influences the function of the brain which in turn influences the
stable and coherent function of the neural networks, physiological systems,
organs, and cellular and molecular biology; how sensory input e.g. as stress,
alters this dynamic relationship leading to pathological onset (genotype and
phenotype) and behavioural change; and how pathological onset leads to
changes of sense perception.
That the magno and parvo-cellular pathways are significant is
evident by noting that loss of vision may occur as a result of brain
damage e.g. when these pathways are damaged or destroyed [84,85],
and due to the effect of drugs, and pathological onset. Almost all
medical conditions, drugs and vaccines influence sense and/or colour
perception. Moreover the mechanism which alters colour perception
incorporates various parameters of the autonomic nervous system
e.g. the ratio of oxyhemoglobin and deoxyhemoglobin in the blood
[86]. This is consistent with sense perception having autonomic
(pathological) origins i.e. which are genetic and non-genetic (lifestylerelated
and/or phenotypic).
Such observations link what we see to the function of the optic
nerve whilst the influence of biological/pathological changes links
how well we see sensory input, in particular colour and visual
contrast, to the presence of pathological factors upon the function of
the amygdala, hippocampus, etc.
Changes of colour perception in the diabetic are therefore linked
to the function of the autonomic nervous systemand, in particular
[87-90], the emission of biophotons being emitted by proteins and
other biologically active and significant moieties as they react with
their reactive substrates e.g. proteins, enzymes [91,92].
The brain is also fed nutritional input from the visceral organs
however it is worth considering whether nutrition can be of value i.e. if the body is short of a particular component this demonstrates
that the body’s physiology is no longer able to retain this component
e.g. a vitamin or mineral. The pathological state becomes the stable
base state. Irrespective, this is significant because of the structural
relationship in which changes of molecular biology i.e. of genotype
and phenotype (note 4) are associated with cellular biology,
organ function, the coherent function of the organ networks (the
physiological/functional systems) and brain function (conceivably
via the neural networks).
This relationship between brain function, the autonomic nervous
system and physiological systems, and cellular and molecular biology
becomes particularly evident in diabetes and obesity - because the
regulation and optimisation of blood glucose is that of a neurally
regulated physiological system. This is significant for reasons outlined
below:
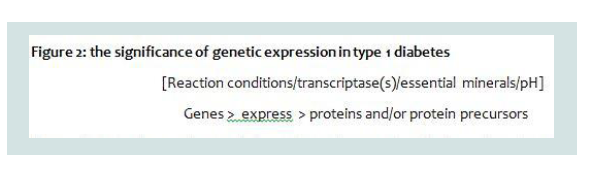
(i) Type 1 diabetes is commonly associated with the coherent
function of >20 genes to express pre-pro-insulin which metabolises
rapidly into ‘insulin’ (the rate is influenced by prevailing pH and
level and bioavailability of essential minerals) however the issue is
complicated by the observation that the spectrum of genes which
express pre-pro-insulin in the Caucasian often differs from the
spectrum of genes which express pre-pro-insulin in different racial
groups i.e. that the chemical profile of the genes is only part of the
mechanism by which the genes express particular proteins (Figure 2)
[10-12,93,94].
Figure 2: Illustrates how under normal circumstances the genes function in
a coherent manner to express a particular protein however this is a chemical
reaction which must be influenced by the prevailing levels and reactivity of
transcriptase(s) which are often dependent upon the prevailing levels of Mg
and Zn. Changes to thegenetic spectrum alters gene conformation [10] and
the prevailing energetics and influences the extent to which the genes will
express a particular protein.
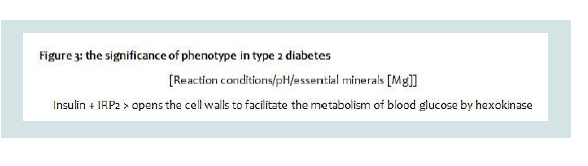
Figure 3: illustrates that the reaction of insulin with its receptor protein IRP2
is a Magnesium dependent reaction which is dependent upon the prevailing
pH, the nature of the acidity, and the level of Mg.
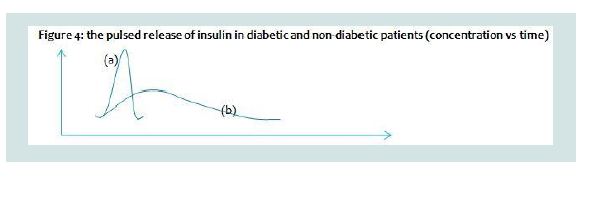
Figure 4: Illustrates how insulin is released in diabetic and non-diabetic
patients e.g. the pulsatile release of insulin in the non-diabetic; (b)the pulsatile
release of insulin in the diabetic. Studies report the pulsatile release of insulin
every 3-5 minutes in the healthy patient and up to 15 minutes in the diabetic
patient.
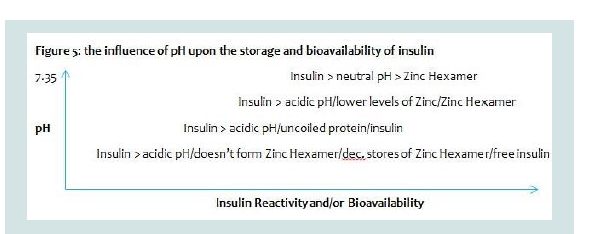
Figure 5: Illustrates how at neutral pH insulin exists in its coiled reactive
state and/or is stored as the Zinc Hexamer. As intercellular acidity increases
the level and bioavailability of Zinc declines, insulin becomes less coiled
and the levels of insulin which are stored as the Zn Hexamer declines. As
intercellular acidity declines still further insulin becomes increasingly uncoiled
and unreactive with the result that stores of Zn Hexamer in the pancreas
decline and need to be supplemented by therapeutic doses of insulin.
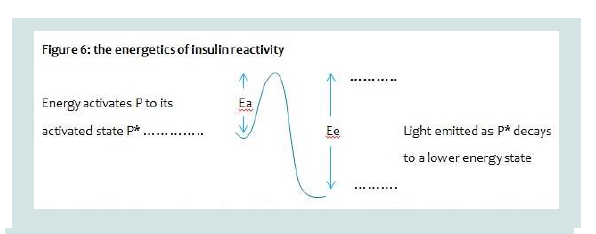
Figure 6: Illustrates how proteins, such as insulin, require to be activated
from their base state to their reactive state by energy before they can react.
Moreover when insulin reacts it releases energy in the form of light as it
decays from its reactive state to its unreactive base state.
Figure 2 illustrates how under normal circumstances the genes
function in a coherent manner to express a particular protein
however this is a chemical reaction which must be influenced by the
prevailing levels and reactivity of transcriptase(s) which are often
dependent upon the prevailing levels of Mg and Zn. Changes to the
genetic spectrum alters gene conformation [10] and the prevailing
energetic and influences the extent to which the genes will express a
particular protein.
(ii) Type 2 diabetes is commonly associated with the rate or level
at which the genetically expressed insulin reacts with its reactive
substrate IRP2. This lack of reactivity is commonly referred to as
‘insulin-resistance’ so what would make insulin ‘resist’ reacting with
its reactive substrate? (Figure 3).
Figure 3 illustrates that the reaction of insulin with its receptor
protein IRP2 is a Magnesium dependent reaction which is dependent
upon the prevailing pH, the nature of the acidity, and the level of Mg.
(iii) This raises two significant issues: (a) type 1 and type 2 diabetes
are considered to be independent of each other yet they are clearly
two consecutive steps in the sequence by which the body metabolises
blood glucose. One follows the other which explains why there is
often misdiagnosis of type 1 as type 2 and vice versa: because type 1
and type 2 are coexistential comorbidities [95,96]; and (b) what are
the factors which could influence the genetic expression of pre-proinsulin,
protein coiling and the reaction of insulin in its coiled state
with the insulin precursor IRP2: because pH influences the prevailing
levels and/or redox states/bioavailability of essential minerals (in
particular of Mg, Zn and Cr) which are essential components in the
etiology of diabetes.
(iv) Many metabolic processes involve the essential minerals Mg
and Zn. In the case of genetic expression, transcriptase enzymes often
require Mg and Zn to be part of their structure and/or to facilitate the
genetic expression of pre-pro-insulin. If there is an insufficiency of
Mg and Zn the rate of genetic expression can reasonably be expected
to decline (Figure 2) [97].
(v) Insulin is a polar entity with -COOH and -NH2 groups at
its extremities therefore its chemical/spatial structure/conformation
i.e. whether coiled and reactive, or uncoiled and un-reactive, must
inevitably be influenced by the prevailing level of intercellular pH.
(vi) Pro-insulin is stored by the pancreatic beta-cells as the
zinc-insulin hexamer. It enables insulin to be released in a pulsatile
manner according to instructions passed by the brain [98-100]. There
is an inverse relationship between the levels of acidity and the storage
of the zinc-insulin hexamer. As acidity increases the pulsatile release
of insulin extends over a longer period (Figure 4).
Figure 4 illustrates how insulin is released in diabetic and nondiabetic
patients e.g. the pulsatile release of insulin in the nondiabetic;
(b) the pulsatile release of insulin in the diabetic. Studies
report the pulsatile release of insulin every 3-5 minutes in the healthy
patient and up to 15 minutes in the diabetic patient.
(vii) The reaction of insulin with its receptor protein is a Mg
dependent reaction therefore lower levels of Mg will reduce the rate
at which this reaction proceeds (Figure 3) [101].
Accordingly, and in order to explain the significance of this
issue it is important to recognise the various dietary and lifestyle
factors which influence the regulation of intercellular acidity/pH and
consequences thereof.
(viii) Elevated levels of intercellular acidity influences the ability
of the pancreas to store insulin as the zinc-insulin hexamer (Figure 5).
Figure 5 illustrates how at neutral pH insulin exists in its coiled
reactive state and/or is stored as the Zinc Hexamer. As intercellular
acidity increases the level and bioavailability of Zinc declines, insulin
becomes less coiled and the levels of insulin which are stored as the
Zn Hexamer declines. As intercellular acidity declines still further
insulin becomes increasingly uncoiled and un-reactive with the result
that stores of Zn Hexamer in the pancreas decline and need to be
supplemented by therapeutic doses of insulin.
(ix) At elevated acidity the levels of free radical reactions
increase and lead to the onset of glycation reactions e.g. of glycated
haemoglobin, insulin, albumin, LDL-cholesterol, etc. There is no
evidence that glycation reactions occur at pH 7.35-7.45 or above
[102];
(x) The body’s inherent bioluminescence is generated by the
absorption and release of biophotons of light by proteins (and/or other bioactive moieties and/or substrates) as they are elevated to their
reactive state and subsequently react with their reactive substrates
and then decay to their less reactive or base state(s) (Figure 6).
Figure 6 illustrates how proteins, such as insulin, require to be
activated from their base state to their reactive state by energy before
they can react. Moreover when insulin reacts it releases energy in the
form of light as it decays from its reactive state to its unreactive base
state.
Such a phenomena, which is recognised in chemistry and
astronomy [73], has both diagnostic and therapeutic significance.
It explains how changes of colour perception accompany the onset
and progression of diabetes [69-75]; how this can be applied to screen
for types 1 and 2 diabetes, and related diabetic comorbidities; and
how light can be applied with therapeutic effect [37,38,41]. It enables
a cognitive diagnostic technique based upon this observation or
principle to track the emergence of type 1 and 2 diabetes from its
presymptomatic origins [33-41]; and conceivably at greater levels of
sensitivity, accuracy and significance than current diagnostic tests
(Note 5).
(xi) When exercising, in order to lose weight, the body consumes
energy from the blood and associated reserves e.g. in the liver and
muscles as glycogen. Depletion of these reserves, because we exceed
the levels stored in the blood and muscles or because we exercise at
a rate which consumes more energy than can be supplied from the
blood, leads to the conversion of stored body fat from adipose or fatty
tissues into fatty acids, or is released as CO2 following its metabolism.
Significantly the metabolism of blood glucose in smooth muscle
is a Cr-dependent reaction therefore the condition/fitness of the
smooth muscle, and the prevailing levels and bioavailability of Cr
is a factor in the conversion of blood glucose into energy (Figure 7)
[103,104].
The metabolism of blood glucose takes place in the smooth muscle.
This is a Cr dependent reaction and hence is dependent upon the
prevailing intercellular pH. Poor muscle tone, elevated intercellular
pH and low levels of essential minerals, often accompanies being
diabetic and overweight, and hence influences the patient’s energy
levels.
(xii) Moreover non-pancreatic forms of diabetes often occurs in
patients who have a range of ailments in other organs e.g. following
a hysterectomy or due to emergent pathologies in the endocrine
organs. The terms hyper/hypo-glycaemia, and acidosis/alkalosis,
suggests that blood glucose and pH exhibit the characteristics of
neurally regulated physiological systems i.e. networks of organs are
regulated by the brain to function coherently and thereby maintain
blood glucose and pH within optimal limits.
(xiii) Protein uncoiling e.g. of insulin ‘resistance’, is not unique to
diabetes and hence to our perception of hunger but is also associated
with other dietary hormones: leptin (leptin-resistance) which is
associated with our feelings of appetite (in the brain), and ghrelin
(ghrelin-resistance) which is associated with feelings of satedness (in
the gut).
(xiv) The consumption of excess amounts of food leads to
expansion of the digestive organs, in particular of the stomach, which influences the levels of ghrelin and feelings of satedness, hence the
use of bariatric surgery to treat those with severely extended stomachs
[31].
In normally healthy patients excess glucose levels are stored as
acyl triglycerides and other complex fatty acids/lipids however the
build-up of such moieties in diabetic patients, in particular omega-6
and saturated fatty acids, are pro-inflammatory and associated with
pathological onset whilst others are less/anti-inflammatory e.g.
eicosapentaenoic acid and docosahexaenoic acid [105].
The pathological significance of pH:
Under acidic conditions free radical/oxidative stress reactions
initiate the conversion of excess glucose and other free sugars (e.g.
fructose, galactose, etc) into glycated metabolites of proteins e.g.
glycated haemoglobin [106], glycated LDL cholesterol, glycated
insulin, glycated albumin, advanced glycation end products, etc.A significant body of evidence links elevated levels of free iron
with the etiology of diabetes [107,108]; free radical reactions occur in
the eye [109]; and, significantly, that antioxidants have a therapeutic
effect [110,111].
Increased blood viscosity arising from elevated levels of blood
glucose, glycated proteins and other viscosity enhancing (thickening)
moieties e.g. elevated blood cell count; influences the ability of the
heart to deliver blood throughout the blood and peripheral blood
vessels [112,113], and hence influence the function of the brain,
lungs, brain, kidneys [1141], liver, etc; and how pathological onset
in any of the visceral organs (in particular the pancreas, pituitary,
thyroid and adrenal glands, heart kidneys, liver, etc) influence the
stable and coherent function of the physiological systems which are
directly implicated in the regulation of blood glucose e.g. sleep, pH,
blood pressure (Figure 1).
Moreover, as each organ is a component in the various organ
networks (physiological systems) which are designed to regulate
key functional parameters, this illustrates the interplay between the
various physiological systems e.g. pH, blood glucose, blood pressure,
temperature, blood cell count [115,116], breathing, sexual function,
blood volume, elimination of toxins and/or wastes, and ultimately
with what we eat and drink. In diabetes, the most significant
physiological systems are the regulation of blood glucose, pH and
sleep [63117-119].
Many medical conditions have a neurological basis or are
influenced by the function of the brain. In scoliosis it is recognised
that the condition often has neurological origins [120]. In cancer
research the study of neuro-oncology is based upon recognition
that the brain plays a role in the onset of cancer. In the study of
diabetes, in particular in neuroendocrinology, there is recognition
of the influence of the brain and the endocrine glands. The brain,
in particular (but not exclusively) the hypothalamus, controls the
secretion of pituitary gland hormones, which influence numerous
interconnections involving the endocrine and nervous system(s).
This illustrates the convergence of the neurological paradigm with
the biomedical paradigm because the brain and endocrines (adrenal,
pituitary and thyroid glands/organs) are component organs in many
of the body’s physiological and/or functional systems.
There is also a relationship between the different physiological
systems and the organs in each system e.g. that patients who undergo
a hysterectomy often have problems regulating blood glucose (nonpancreatic
diabetes); whilst recent research has indicated that glucose
can trigger sleepiness after a meal by triggering neurons in the
hypothalamus which participate in the regulation of sleep [121]. This
illustrates how instability in one physiological system can influence
the stability and function of other physiologically adjacent systems
and/or organs. Moreover the observation that there is a neural
network which connects various areas of the cerebral cortex to the
adrenal gland illustrates the link between brain function [122], the
neural networks, the autonomic nervous system and pathological
onset.
Current research is now exploring the connection between neural
networks and diabetes although restricted to artificial neural networks
which perhaps illustrates an adherence to current etiology rather
than a fundamental consideration, or understanding, of the complex
nature of diabetes however there is now an emerging consensus that
the brain is involved in the management of diabetes, in particular
via the hypothalamus and the autonomic nervous system although
the focus of research appears to be focused upon the changes which
occur as a result of pathological onset rather than considering the
fundamental control mechanism provided by the brain [47,123-125].
The issue is complicated as researchers invariably continue to
seek a ‘magic bullet’ which can be used to provide an immediate ‘fix’
e.g. via a drug, or an electric stimulus via implants which are attached
to the nervous system; and thereby ignore the complex nature of the
body’s function i.e. the neural regulation of the autonomic nervous
system and physiological systems, and how it is naturally influenced
by sensory input.
Strannik Case Studies
The Strannik technology is based upon a precise and sophisticated
neural simulation and/or mathematical model of how the brain
receives sensory input, and how such sensory data sets can influence
brain function and the regulation of the autonomic nervous system,
physiological systems, organs, and cellular and molecular biology.
We report in this paper a series of case studies, reported by medical
doctors at the study clinics, in which diabetic patients have been
screened and treated using the Strannik technology:
In the following case studies Strannik Virtual Scanning was
used, alongside other diagnostic tests and observations by the GP,
to determine the patient’s health before determining the specific
parameters required for a course of Strannik Light Therapy i.e. which
was appropriate for their condition.
Patient: male; 55 y.o.:
Diagnosis: weight 104 kgs, essential hypertension. After forty
sessions of the additional ‘overweight protection’ SLT course the
patient’s weight declined by 21 kilos, cardiovascular indices stabilised,
sleep and work efficiency restored.Patient: female; 65 y.o.:
Diagnosis: weight 93 kgs. The patient was diagnosed with
dyscirculatory encephalopathy, hearing loss, sinusitis, calcium
deficiency, hepatitis A, cholecystitis, pancreatitis, cardiomyopathy, heart arrhythmia, iron deficiency, gastroduodenitis, irritable bowel
syndrome, osteochondrosis with neurological symptoms. The
organism was unable to maintain normal levels of blood glucose,
circulating blood volume and blood pressure. Nine organs were
organically changed. The client was prescribed the ‘anti-aging’ and
the ‘overweight protection’ SLT courses. After a course of SLT the
patient’s condition had improved, the organic changes of the organs
were absent, and weight reduced to 84 kgs, a loss of 9 kgs.Patient: male; 64 y.o.:
Diagnosis: diabetes; diabetic angiopathy; kidney failure. After 14
days of using the SLT program, the cardiologist reduced the dose of
insulin injected from 32 to 22 units.Patient: male; 50 y.o.:
Diagnosis: diabetes. Blood sugar test revealed 8 mmol/liter;
reduced to 6.5 mmol/litre after a course of SLT.Patient: female; 55 y.o.:
Diagnosis: weight 78 kgs. By the 50th day of the anti-aging SLT
course the patient’s weight declined by 5 kgs without any special diet.Patient: male; 53 y.o.:
Diagnosis: weight 85 kgs. The patient complained of heart pain,
headache caused by changes of arterial tension; and infarction of
posterior wall of the left ventricle of the heart. After first month of the
‘anti-aging’ SLT course, vision improved; blood pressure stabilized at
120/75, the patient stopped taking medicine.Patient: female; 53 y.o.:
Diagnosis: weight 87 kgs. The patient complained of excess
weight and essential hypertension. After 20 sessions of SLT course,
the patient’s weight declined by 11 kgs and 12 cms around the waist;
had lack of appetite; arterial tension stabilized.Patient: female; 43 y.o.:
Diagnosis: diabetes, type 2, weight 96 kgs, prescribed insulin.
After the ‘anti-aging’ SLT course, the patient’s weight declined by 5
kgs, working efficiency increased, blood sugar level reduced, sugar
and ketone bodies in urine were absent, diuresis reduced. The patient
stopped taking insulin, now taking antihyperglycemic drugs.Patient: male; 79 y.o.:
Diagnosis: swollen foot (diabetic foot ulcer), type 1 diabetic, lack
of mobility. After 3-6 months of SLT his swollen foot was no longer
swollen and he had fully recovered his mobility.Patient: male; 23 y.o; narcotic dependence.:
Diagnosis: diabetes, 1 type, heavy form, diabetic encephalopathy,
polyneuropathy, microangiopathy, blood glucose at 10-17 mmol/l.
The patient was receiving up to 40 units per day of insulin. After
5 sessions of SLT the level of sugar in the blood was lowered to 5
mmol/l, and was accompanied by hypoglycaemia. It stabilized at 7-8
mmol/l. The insulin dose and drug dependency were decreased.Conclusion
The traditional view or etiology of diabetes is based upon
consideration of the effectiveness of the pancreas to express pre pro-insulin and the reactivity of insulin, commonly referred to as
‘insulin-resistance’however the author suggests in this paper specific
shortcomings with the prevailing etiology of diabetes mellitus:
(i) Diabetes is considered to be a problem which is solely associated
with the function of the pancreas whereas the evidence suggests that it
is a multisystemic, multipathological and polygenomic disorder;
(ii) Diabetes is considered to be a problem of the pancreas whereas
the evidence suggests that it is a problem associated with the neural
regulation of the physiological system which regulates blood glucose
levels and hence that pathological onset in organs and related systems
i.e. other than the pancreas, may influence blood glucose levels;
(iii) Diabetes is considered to be two distinct pathologies in
which impaired genetic expression of insulin and subsequent insulin
reactivity are the most common diabetic symptoms yet the evidence
suggests that in most cases diabetes is a problem of type 1 AND
type 2 diabetes i.e. the two conditions are co-existential morbidities,
thereby illustrating that there is a need for more sophisticated ways of
diagnosing diabetes;
(iv) Understanding the fundamental mechanisms by which the
brain regulates blood glucose levels has significant diagnostic and
therapeutic potential.
An increasing body of evidence illustrates that the brain plays a
fundamental role regulating the function of the autonomic nervous
system [126,127], and its effect upon energy balance and glucose
homeostasis i.e. through its relationship with the physiological
systems, organs and/or tissues. That it involves how the senses function
is clearly evident but it must also include e.g. the role of the amygdala
(receives and processes sensory data), hypothalamus (generates
neuroendocrine output/hormones), brain stem, hippocampus (shortterm
memory) [128], cerebral cortex (long-term memory) [129], and
the transmitting mechanism - the vagus nerve; which are implicated
in this enormously sophisticated process; and hence which play an
immensely significant role in the regulation of blood glucose levels by
the coherent and biodynamic function of the brain with the pancreas,
endocrines, etc. [130-133].
The case studies presented illustrate how such knowledge can be
applied with therapeutic effect to achieve outcomes which appear to be
beyond that which is possible using drugs (which treat the symptoms
and fail to take into account the complexity of the condition) and
which has the potential to enhance how the patient is screened and/
or treated. Examples are presented of how this can be used to treat
weight problems, diabetic foot ulcer, high blood pressure, erectile
dysfunction, mental health issues, and influence cognitive decline
and/or the aging process.
This illustrates the existence of a complex neurally regulated
mechanism - a regulated network of organ networks - which
continuously monitors and adjusts levels of all physiologically
significant parameters including, but not limited to, blood glucose
i.e. that the multilevel function of the brain is the dominant
characteristic which via the senses continuously monitors and adjusts
our nutritional requirements (that under normal non-pathological
conditions that the brain is able to exert an extraordinarily fine level
of control of calorific intake); yet is continuously influenced at the psychosomatic level by the effect of stress upon brain function and
the autonomic nervous system, and by emergent pathologies (of
genetic and/or non-genetic origins) in the visceral organs in this and
other physiological systems.
Moreover the rate of supply of food is as critical to the flow of
energy as the rate of supply of insulin, perhaps more so. If the supply
of calories increases significantly this stimulates the supply of insulin
whereas under acidic conditions normal or elevated levels of insulin
will be accompanied by feelings of appetite and hunger. The issues
are complicated by variations of acidity which alter protein reactivity,
in particular (but not solely) of leptin, insulin and ghrelin which
influence our feelings of appetite, hunger and satedness; and the
emergence of pathological onset in other organs and systems e.g.
explaining the phenomena of non-pancreatic diabetes in which the
patient e.g. following a hysterectomy, has problems regulating blood
glucose levels.
In light of the issues reviewed in this paper the author makes the
following conclusions and/or recommendations e.g.
• Insulin is supplied mainly by the pancreas but also to a lesser
extent by other endocrine organs therefore the focus upon the
pancreas can only be part of the etiology of diabetes;
• The pancreas is only one of the organs in the physiological
system which regulates blood glucose levels therefore pathological
onset in other organs within this system must also contribute to
variations in blood glucose levels;
• The brain is intimately involved in the regulation of blood
glucose levels and dysfunction of this mechanism is experienced as
diabetes and comorbidities in other organs and systems;
• Problems of blood glucose regulation (diabetes) may occur in
patients with a normally functioning pancreas;
• When considering diabetes from the current perspective, in
particular the genetic expression of insulin and ‘insulin resistance’,
type 1 and type 2 diabetes are co-existential comorbidities;
• Protein reactivity e.g. of leptin, insulin and ghrelin (and hence
our feelings of appetite, hunger and satedness) - is influenced by the
prevailing level of intercellular pH;
• Sleep exhibits the characteristics of a physiological system and
hence that lack of good quality sleep influences brain function and
autonomic control;
• The brain plays a fundamental role regulating and optimising
blood glucose levels, and levels of all the body’s essential functional
parameters;
• The brain uses a complex mechanism involving frequency and
light to regulate the body’s autonomic stability and function;
• Knowledge of how the brain functions, which is incorporated in
the mathematical model developed by Grakov IG, can be used with
significant diagnostic and therapeutic effect, and achieve therapeutic
outcomes which are comparable with what can be achieved by
biomedicine and in some circumstances are better than can be
achieved using drugs
• Improved autonomic control influences sense perception e.g.
feelings of appetite, hunger and satedness;
• The different brain wave states are associated with different
levels of cellular and molecular biology;
• Instability in other, apparently unrelated, physiological systems
may lead to problems of blood glucose regulation i.e. as the brain
seeks to optimise the body’s physiological stability.
Conflicts of Interest:
The author is Chief Executive of Mimex Montague Healthcare, a
company which is devoted to the commercialisation of the Strannik
technology developed by Dr Igor Gennadyevich Grakov.Notes
[1] many/various techniques have been developed which claim/
provide their therapeutic effect by providing stimulation at various
EEG frequencies e.g. HeartMath, Strannik Light Therapy, Brightstar
Learning, AddBrain, etc; an industry of estimated value USD10-
20BN pa (Table 1).
[2] In this paper stress is considered in a wider context than the
more usual psychological context i.e. to include the stress of excess
weight.
[3] The limbic structure; including the thalamus, hypothalamus,
etc; is associated with emotional changes e.g. are widely considered to
be associated with hunger, aversion, sexuality, extremes of pleasure
and displeasure, aggressiveness, fear, etc.
[4] This paper uses the terms genotype and phenotype to define (i)
genotype: the rate and extent to which the genes express a particular
protein or other biologically active moiety and (ii) phenotype: the
non-genetic component by which the environment and/or stress
inhibits the rate at which a particular protein or other biologically
active moiety reacts with its reactive substrate (the autonomic
response).
[5] The eyes respond to as little as 7*10^2 biophotons per second.
Acknowledgement
The lack of understanding of how the whole body functions
rather than the separation of research into component parts
(reductionism) often leads to contradictory conclusions with the
result that some research is favoured over others. With this in mind
we thank the many researchers who, through their work, have
indirectly contributed to this paper.
References
33. Ewing GW, Parvez SH (2008) Systemic regulation of metabolic function.
Biogenic Amines 22: 279-294.
101. Barbagallo M, Dominguez LJ (2015) Magnesium and type 2 diabetes. World
J. Diabetes 6: 1152-1157.