Journal of Oral Biology
Download PDF
Review Article
Problem Solving Guidelines for Aesthetically Compromised Maxillary Anterior Implant Restorations
Shalin Vinayak*, Lara Ceballos, Carlos Diaz-Mauriño, Stephen Chi and Yung Cheng Paul Yu
- Department of Periodontology and Implant Dentistry, New York University, USA
*Address for Correspondence: Shalin Vinayak, Department of Periodontology and Implant Dentistry, New York University, Clinic 5W, 345 E 24th St, New York, NY 10010, USA, Tel: +1 (212)-992-7040; E-mail: sv1506@nyu.edu
Citation: Vinayak S, Ceballos L, Diaz-Mauriño C, Chi S, Yu YCP. Problem Solving Guidelines for Aesthetically Compromised Maxillary Anterior ImplantRestorations. J Oral Biol. 2018; 5(1): 7.
Copyright: © 2018 Vinayak S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Oral Biology | ISSN: 2377-987X | Volume: 5, Issue: 1
Submission: 15 January, 2018 | Accepted: 30 April, 2018 | Published: 06 May, 2018
Keywords
Dental implants; Patient satisfaction; Complications; Complaints; Aesthetic failures
Abstract
The objective of modern implant dentistry is to provide a long lasting restoration that harmoniously replicates the contours of the neighbouring hard and soft tissue. Improvements in implant designs, materials, surfaces and surgical techniques have allowed for osseointegration to be achieved predictably. However, dimensional differences between the implant and the extracted tooth, as well as biological limitations at the site make aesthetics of the restoration the greater challenge. Over the years, several methods of assessing the aesthetics of an implant restoration using various visual analogue scales have been proposed, though they have mostly been used as a means for clinicians to assess the outcome of their restoration. Nevertheless, the final aesthetic outcome depends on the patient’s satisfaction of their restoration. Based on clinical findings and a review of the literature, a guideline has been proposed highlighting the common complaints a patient has towards their implant supported restoration, and several methods of addressing these complaints have been discussed.
Introduction
Implantology has made great advances in recent decades [1]. Improvements in implant designs, materials, surfaces, and surgical techniques along with a better understanding of the biology allow for osseointegration to be achieved predictably [2,3]. This has led to the widespread adoption of implants as a viable treatment option to restore masticatory function. However, the primary concern for many patients is not only to restore function, but to restore aesthetics, particularly in those with missing teeth in the maxillary anterior region [4].
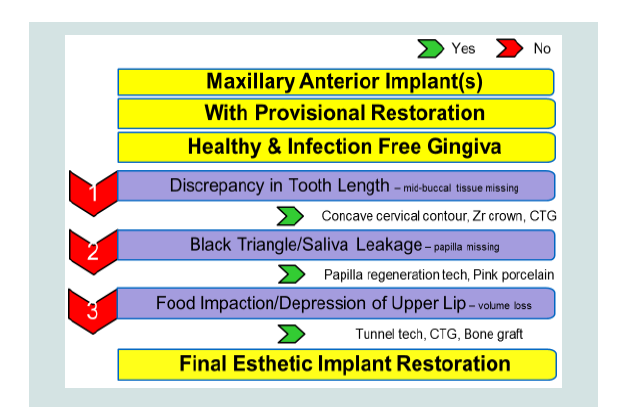
The goal of treatment is to provide a restoration that harmoniouslyreplicates the normal contour of neighbouring dental hard and softtissues and to be indistinguishable from its adjacent teeth (Figures 1A and 1B). This presents a challenge because individuals have different aesthetic demands. In addition to the difference in perception between patients, there are differences in evaluation of an aesthetic outcome between clinicians and patients, and between clinicians themselves [5,6]. Clinicians evaluate aesthetics by quantifying certain parameters, such as when using the Pink Esthetic Score (PES) and White Esthetic Score (WES) assessments, to numerically score individual aspects of the restoration and soft tissues to determine if they have achieved a clinically acceptable level of aesthetics. However, for a restoration to truly be considered a success, the patient must be satisfied with theaesthetic outcome [7,8].
Figure 1: A: A 28 year old female patient presented with a fractured maxillary right central incisor (No. 8) as well as a chipped lateral incisor (No. 7), and a chief complaint of wanting restoration of aesthetics and function. B: Implant supported provisional restoration of the maxillary right central incisor that achieves the goal of harmoniously replicating the contours of neighbouring hard and soft tissues along with restoring function. Composite was applied to the adjacent lateral incisor to restore symmetry to the contralateral side.
Potential aesthetic shortcomings of implant therapy can be identified by the clinician early in the course of treatment. Horizontal and vertical defects, a high smile line or a thin tissue biotype along with unrealistic patient expectations may be assessed during treatment planning and alert the clinician to the degree of difficulty in delivering an aesthetic restoration [9]. Other factors that can impact the aesthetic outcome may be noticed at uncovery, such as deviations from the planned implant position [10]. The patient can begin to appreciate the aesthetics when the provisional restoration is inserted, and it is usually at this stage that most concerns arise. Complaints regarding crown length, the presence of black spaces between adjacent crowns, the seepage of saliva through them, and a depression of the upper lip can be attributed to a discrepancy of the gingival tissues, the underlying bone or prosthetic design. Complaints regarding colour, texture or translucency of the crown imply a discrepancy in the restoration itself, perhaps due to a lack of communication between the dentist and the laboratory. The clinician must be aware of the patient’s remarks and complaints regarding aesthetics when restoring an implant so that the best treatment options can be provided for them. Few articles in the literature focus on the patient’s perception of their implant supported restoration [11,12].
While the purpose of this report is to describe techniques to improve the aesthetic outcome of an already restored or provisionalized implant, extensive treatment planning must be done prior to implant placement to identify and address aesthetic risk factors to minimize any future shortcomings. A thin soft tissue biotype or thin facial plate of bone should be augmented before or at the time of implant placement to minimize facial recession. The level of the interproximal bone at adjacent sites must be evaluated to predict the level of the future papillae, and the patient must be made aware of realistic outcomes of treatment. The contour of the facial plate of bone must be assessed and any undercuts should be addressed before or at the time of implant placement to provide adequate lip support and prevent food impaction following restoration. Recently, techniques that involve keeping the labial portion of the anterior tooth root and placing the implant in a position lingual to this have been described [13,14]. They have the potential to maintain the level of the buccal tissues however these techniques should be applied with caution due to the limited evidence available.
Materials and Methods
A search of the literature was performed on common aesthetic shortcomings related to implant supported restorations focusing on the opinions of patients and clinicians alike. Clinical data in this study was obtained from the anonymous Implant Database (ID) at the Ashman Department of Periodontology and Implant Dentistry at the New York University College of Dentistry. This data was extracted as de-identified information from the routine treatment of patients. The ID was certified by the Health Insurance Portability and Accountability Act (HIPAA) and approved by the University Committee on the Activities Involving Human Subjects (UCAIHS). A computer search of electronic database from MEDLINE and PUBMED at the Waldman Library at the NYUCD was performed. Keywords such as “dental implants”, “patient satisfaction”, “complications”, “complaints”, “aesthetic failures”, were used, alone and in combination, to search the databases. Non-English language publications were excluded. The search was limited to studies involving human subjects. Restrictions were not placed regarding the type of study design.
Result
The aesthetic shortcomings and complaints discussed in this study are based on clinical findings and a review of the literature. These are compiled and presented in Table 1. Patient’s remarks and complaints regarding aesthetics when restoring an implant should be part of the overall considerations to provide better treatment options. The techniques described allowed us to improve patient satisfaction in some cases however unrealistic expectations or improper treatment planning can lead to compromised outcomes.
Discussion
The clinician is faced with several limitations when attempting to restore aesthetics, particularly in the maxillary anterior region. The physiologic resorption after tooth loss along with the establishment of an implant biologic width contributes towards a hard and soft tissue discrepancy at the site. Furthermore, there are differences in size and shape between the implant and the tooth being replaced. These include a flat implant shoulder versus a scalloped cement enamel junction, a round cross section of the implant compared to a triangular cross section of an anterior tooth, as well as the smaller circumference of the implant in relation to the natural tooth at the same level [15]. These differences require the implant to be placed subcrestally and palatally to allow sufficient room for the restoration emergence to compensate for the variations [5]. It is therefore a challenge to achieve aesthetic harmony with the contralateral side, and the clinician must be prepared to manage patient complaints towards the implant restoration. The following are techniques that can be employed in an attempt to improve the aesthetics based on commonly encountered patient complaints.
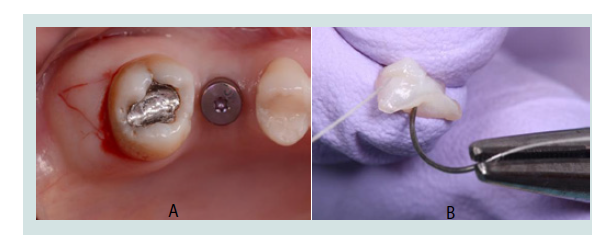
Chief complaint 1: My implant tooth is longer than the other teeth
A discrepancy in tooth length of the implant supported crown is not an unusual occurrence (Figure 2). Chang M et al. reported that clinical crowns supported by implants were an average of 1 mm longer than the clinical crowns of adjacent teeth. This discrepancy arises due to the bone loss that occurs following extraction, or after insertion of the implant crown and establishment of biologic width [16]. Despite precautions to preserve or augment this region prior to implant placement, the patient may still be unsatisfied when the provisional restoration is inserted and would complain about the crown appearing too long.
Figure 2: A successfully osseointegrated implant in the maxillary right central incisor position has been fitted with a longer clinical crown than the adjacent central incisor due to an apical position of the mid-buccal tissues.
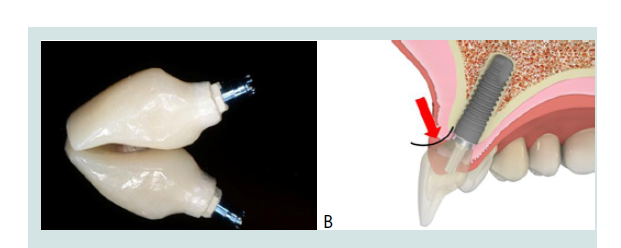
Design of the provisional restoration has an influence on the level and form of the mid-buccal tissues. An ideal contour of the abutment and crown is required to maintain the form of the marginal soft tissue. Excessive pressure from an over contoured restoration negatively affects the blood supply to the mid-facial tissues, causing recession. Under contouring the cervical portion of the provisional abutment and crown to create a concave emergence profile has been shown to exert minimal pressure on the facial tissue which minimizes recession and may allow for an increase in soft tissue volume, in the absence of periodontal disease (Figures 3A and 3B). This technique is particularly indicated in implants placed slightly labially. However, an excessively under contoured restoration is difficult to clean effectively and may not support the marginal tissues, resulting in a flattened or rolled appearance [17].
Figure 3: A: A minimally under-contoured provisional restoration to establisha concave emergence profile. B: The ideal emergence profile should be concave to avoid excessive pressure on the soft tissues while still being cleansable.
If prosthetic modification alone cannot achieve the desired aesthetic result, an improvement may be attainable through soft tissue surgical procedures. A wedge of connective tissue can be harvested from specific keratinized intraoral sites and grafted around the periimplant tissues to increase thickness of the mid-facial and papillary tissues. This donor tissue can be harvested from the palate however precautions should be taken to avoid traumatizing the greater palatine artery and nerve [18,19]. Another donor site for the Connective Tissue Graft (CTG) is distal to the most posterior tooth in the maxilla, in the tuberosity region. The tissue in this region is firm, thick and safely away from major Vessels and nerves (Figures 4A and 4B) [20]. The advantages of the CTG compared to allogenic grafts thin facial tissues are its predictable level of success and its high chance of survival if a portion of it gets exposed.
Figure 4: A: An incision is made in the tuberosity region to obtain a wedge of connective tissue. B: The harvested connective tissue from the tuberosity region was deepithelialized extra-orally and secured with a holding suture (Vicryl 5-0) in preparation for grafting.
It has been shown that the various restorative materials elicit different levels of soft tissue response [22]. The favourable physical and aesthetic properties of zirconia abutments and crowns have been published by several authors [23,24]. Additionally, studies have shown that zirconia accumulates less plaque than titanium [23,25]. A recent study by Kajiwara N et al. showed significantly greater blood flow was maintained around zirconia abutments compared with metal abutments [20]. Therefore the use of zirconia abutments and crowns to restore an implant may have a beneficial influence on the long term maintenance of periimplant tissue health.
The gingiva in some patients may be hyperplastic or have an irregular topography. A delicately performed gingivectomy or gingivoplasty of the adjacent natural teeth can create a more ideal soft tissue contour and may reduce the appearance of a crown length discrepancy on the implant restoration (Figures 5A and 5B). However, the biologic width around the natural teeth must be respected in order to maintain long term stability of the margin. Therefore, the underlying bone level determines the amount of tissue that can be excised.
Figure 5: A: Maxillary left central incisor implant supported restoration hasa longer clinical crown than the contralateral central incisor due to facial recession caused by excessive labial placement of the implant. Note the hyperplastic nature of the tissues surrounding the adjacent teeth. B: Outcome after gingivectomy of the adjacent central incisor in an attempt to minimize the asymmetry between the two teeth and improve tissue topography.
Chief complaint 2: I don’t like the black space next to my implant crown and saliva spills through it when I speak
The presence of an interdental papilla is necessary to achieve an aesthetic restoration that is harmonious with the scalloped gingival contour of the adjacent teeth, however it is not always possible to achieve this clinically. The loss of interproximal tissues in the aesthetic zone is of particular concern as comparisons to the contralateral side highlight the asymmetry of the gingival contours and give prominence to the deficiency. In addition to the unesthetic black triangle, the interproximal space allows for the seepage of saliva through it during speech, which can predispose the patient to embarrassing social situations. The space further promotes food impaction and requires greater oral hygiene measures to keep free of plaque.
A study by Tarnow DP et al. showed that when the distance fromthe contact point to the crest of bone around natural teeth was 5 mmor less, the papilla was present almost 100% of the time. When thedistance was 6 mm, the papilla was present 56% of the time, and whenthe distance was 7 mm or more, the papilla was present in only 27% ofcases [26]. When there is a tooth adjacent to the implant, it has beenshown that the height of bone around the natural tooth, and not thelower level around the implant, influences the papilla [27]. Prostheticalteration of the crown to lower the contact point reduces the distancefrom the bone peak and may allow for papillary fill and a less visibleinterproximal space. This may improve the aesthetic outcome of asingle implant restoration. However, it is very unlikely to improvewhen performed between adjacent implants. Tarnow DP et al. furthershowed that the average inter-implant papilla height from the crest ofthe bone peak is 3.5 mm due to the establishment of biological widtharound each implant. This is 2 mm shorter than that seen betweenhealthy teeth [28]. This difference can pose an aesthetic problem forpatients that have an average or high smile line displaying the cervicalportions of teeth and gingiva. Prosthetically lowering the contactpoint between adjacent implant restorations can be done withoutimpacting the aesthetic outcome only when the implants are in the central incisor positions. Despite changing the shape of the crowns,symmetry is maintained as they are located on either side of themidline (Figure 6) [29].
Figure 6: The contact point was made longer to reduce the size of the black triangle between adjacent implants in the maxillary central incisor positions. The patient was pleased with the outcome, despite changing the shape of the crowns, due to symmetry achieved on either side of the midline.
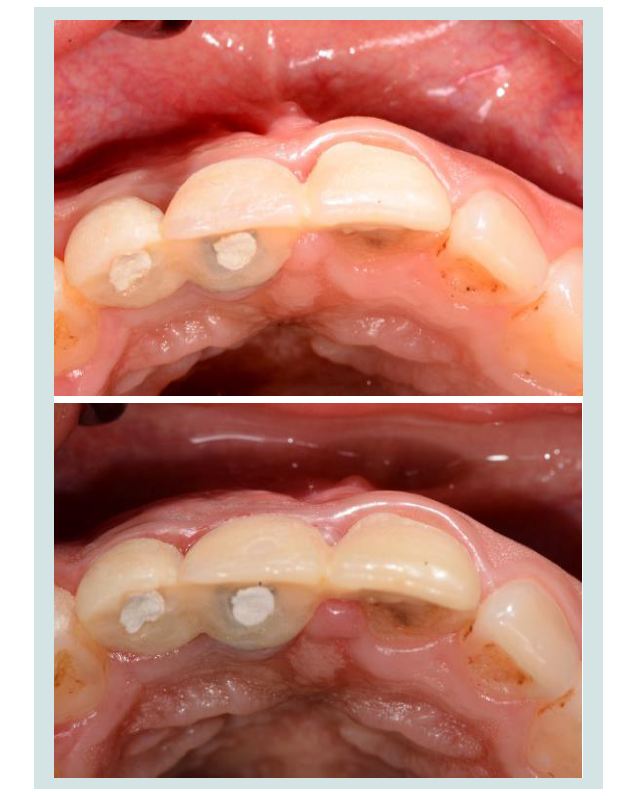
When it is not possible to establish the papilla by altering the contact point, surgical procedures and papilla regeneration techniques can be considered. Several flap techniques have been proposed to recreate the missing papilla such as the palatal striding slip flap, U-shaped incision and Pallaci’s 90 degree flap rotation. Froum and colleagues presented a technique to create a mucoperiosteal tunnel from the buccal to the palatal aspect of the deficient site and insert a connective tissue graft (Figures 7A-7D) [21]. The desired result of these surgical techniques is an increase in soft tissue thickness in the papillary region, which can then be sculpted by the provisional restoration.
Figure 7: A: An unesthetic black triangle in the maxillary anterior regionbetween an implant supported crown and an irregularly shaped lateral incisor. B: Creation of a mucoperiosteal tunnel from the buccal to the palatal aspect underneath the deficient papilla, and preparation of the maxillary left central incisor for a full coverage crown. C: Occlusal view showing the connective tissue graft sutured in place through the mucoperiosteal tunnel. D: A successfully restored papilla that was achieved using a combination of papilla regeneration techniques and a restoration with a lowered contact point.
Pink porcelain and pink composite are options to prosthetically augment sites of soft and hard tissue defects, such as black triangles and apically located mid-buccal tissue, to mask the defects and restore contour (Figures 8A,8B and Figure 9). The advantages are that further surgery to address the defect may be avoided and an immediate solution is provided. However, these prosthetically augmented regions require a high level of oral hygiene and regular maintenance to prevent accumulation of plaque and debris, particularly when extended over the buccal tissues in a ridge-lap design. Additionally, pink composite is prone to staining and abrasion and requires regular maintenance to retain its aesthetic value [30].
Figure 8: A: A 29 year old patient with severe discrepancy of mid-facial tissues around her implanted supported maxillary right central incisor. Patient was unsatisfied with the appearance of the longer clinical crown. B: Pink porcelain was added to the cervical portion of the implant supported crown in an attempt to establish a harmonious contour with the adjacent soft tissues. While the patient preferred it to the long crown, she was not completely satisfied.
Chief complaint 3: There is a depression in my upper lip, and food gets stuck under this area
A common complication that arises after dental implant placement is a facial concavity of the periimplant tissues, particularly when the facial bone or overlying soft tissues are thin (Figure 10) [31]. This presents an aesthetic and functional problem for the patient when located in the maxillary anterior region. The form of the upper lip is determined by its musculature as well as by the support of the underlying hard and soft tissues. A large concavity in the facial region can lead to a collapse of the overlying tissues causing a depression of the lip. From a functional perspective, this intraoral depression promotes food impaction, plaque retention around the teeth and tissue irritation. Depending on the size of this defect, it can be masked to a limited degree prosthetically using pink porcelain as previously discussed, or it can be managed surgically through soft tissue grafts and bone grafts.
Figure 10: A 34 year old patient with an implant placed in the maxillary right central incisor position. The severely resorbed ridge resulted in a buccal defect. Patient complained about food getting trapped in the defect as well as a collapse of her upper lip.
Several surgical techniques have been advocated to improve the contour of a facial defect in the aesthetic zone. These procedures include various flap designs, inlay or onlay grafts, or the use of acellular dermal matrix alone or in combination with bone grafts to augment the site. The tunnel technique is a type of flap design that can be effectively applied to gain access and create a site for placement of a soft or hard tissue graft to augment this facial defect (Figures 11A and 11B). There is no recession of the crestal tissues as the periosteum of that region is not reflected. Additionally, vestibular depth is maintained as tension free closure can be achieved without having to coronally reposition the tissues [32].
Figure 11: A: Patient complained of food getting stuck in the defect labial totwo adjacent implants in the maxillary anterior region. B: A connective tissue graft on the facial aspect was inserted using the tunnel technique to augment the site. The patient was satisfied with the increased tissue thickness that resulted.
A soft tissue graft alone cannot restore the contour when the facial defect is large. In these cases, a bone graft can be considered to rebuild the defect (Figures 12A and 12B). The tunnel technique is indicated to gain access to the site, particularly when the implant has already been placed, as it maintains the blood supply to the vital crestal bone [32]. A particulate xenograft is advantageous as it has a very low rate of resorption and can maintain the rebuilt contours at the site for a longer period of time [33]. The placement of a membrane over the graft can help maintain the stability of the graft particles and blood clot under the influence of muscular action. A connective tissue graft may be considered prior the placement of the bone graft to thicken the tissues and aid in achieving tension free closure.
Figure 12: A: A prominent buccal depression in the region apical to themaxillary right central incisor. In this case, the patient’s primary concern was food constantly getting trapped in the defect. B: A substantial increase in bucco-lingual width of the deficient ridge was achieved with a bone graft at the site. The defect was eliminated and the patient was pleased with the outcome.
Summary
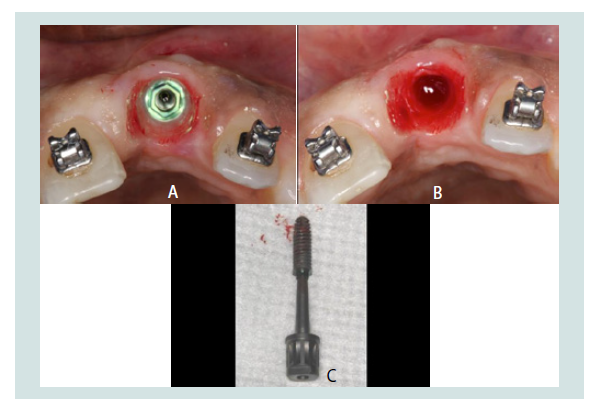
Aesthetic shortcomings in the final restoration can arise from discrepancies in the soft tissues, the underlying hard tissues, or a combination of both. They may also be the result of a poorly contoured prosthetic component. The patient’s comments can help determine which of the above aspects must be addressed. The clinician must be aware that aesthetics of a restoration can only be modified to a certain degree at the provisional stage. If an adequate result cannot be attained using the techniques discussed, more invasive procedures may be required. In an extreme scenario, the implant may need to be removed for placement in a more suitable position with or without hard and soft tissue grafts (Figures 13A-13C).
Figure 13: A: Outcome of the case mentioned in Figure 5. Excessive labialpositioning resulted in thinning and recession of the facial tissues and an aesthetic problem that could not be improved by surgical or prosthetic measures. B: The implant was removed and it was planned for placement in a more suitable position after healing to achieve a satisfactory aesthetic result. A: Outcome of the case mentioned in Figure 5. Excessive labial positioning resulted in thinning and recession of the facial tissues and an aesthetic problem that could not be improved by surgical or prosthetic measures. B: The implant was removed and it was planned for placement in a more suitable position after healing to achieve a satisfactory aesthetic result. C: The failed implant. Despite having osseointegrated successfully, it was considered a failure as it did not provide an aesthetic, harmonious result to satisfy the patient and clinician. It was reverse torqued, with minimal trauma to the patient.: The failed implant. Despite having osseointegrated successfully, it was considered a failure as it did not provide an aesthetic, harmonious result to satisfy the patient and clinician. It was reverse torqued, with minimal trauma to the patient.
The ultimate aesthetic outcome depends on the patient’s satisfaction of their restoration. It is important to discuss limitations of the procedures when formulating the treatment plan with the patient so that they have realistic expectations prior to commencement of treatment.
Acknowledgements
Special thanks to Dr’s. Sofia A. Lopez, and Abdullah S Alodadi for their contribution of clinical cases and revision of the manuscript.
References
- Jimbo R, Albrektsson T (2015) Long-term clinical success of minimally and moderately rough oral implants: a review of 71 studies with 5 years or more of follow-up. Implant Dent 24: 62-69.
- Pjetursson BE, Asgeirsson AG, Zwahlen M, Sailer I (2014) Improvements in implant dentistry over the last decade: comparison of survival and complication rates in older and newer publications. Int J Oral Maxillofac Implants 29 Suppl: 308-324.
- Coelho PG, Granjeiro JM, Romanos GE, Suzuki M, Silva NR, et al. (2009) Basic research methods and current trends of dental implant surfaces. J Biomed Mater Res B Appl Biomater 88: 579-596.
- Higginbottom FL (2005) Implants as an option in the esthetic zone. J Oral Maxillofac Surg 63 (9 Suppl 2): 33-44.
- Tettamanti S, Millen C, Gavric J, Buser D, Belser UC, et al. (2016) Esthetic evaluation of Implant crowns and peri-implant soft tissue in the anterior maxilla: comparison and reproducibility of three different indices. Clin Implant Dent Relat Res 18: 517-526.
- Jones AR, Martin W (2014) Comparing pink and white esthetic scores to layperson perception in the single-tooth implant patient. Int J Oral Maxillofac Implants 29: 1348-1353.
- Fürhauser R, Florescu D, Benesch T, Haas R, Mailath G, et al. (2005) Evaluation of soft tissue around single-tooth implant crowns: the pink esthetic score. Clin Oral Implants Res 16: 639-644.
- Belser UC, Grütter L, Vailati F, Bornstein MM, Weber HP, et al. (2009) Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria: a cross-sectional, retrospective study in 45 patients with a 2-to 4-year follow-up using pink and white esthetic scores. J Periodontal 80: 140-151.
- Elian N, Ehrlich B, Jalbout ZN, Classi AJ, Cho SC, et al. (2007) Advanced concepts in implant dentistry: creating the “aesthetic site foundation”. Dent Clin North Am 51: 547-563.
- Basten CH (1995) The use of radiopaque templates for predictable implant placement. Quintessence Int 26: 609-612.
- Derks J, Håkansson J, Wennström JL, Klinge B, Berglundh T (2015) Patient-reported outcomes of dental implant therapy in a large randomly selected sample. Clin Oral Implants Res 26: 586-591.
- Locker D (1998) Patient-based assessment of the outcomes of implant therapy: a review of the literature. Int J Prosthodont 11: 453-461.
- 13.Siormpas KD, Mitsias ME, Kontsiotou-Siormpa E, Garber D, Kotsakis GA (2014) Immediate Implant placement in the esthetic zone utilizing the “root-membrane” technique: clinical results up to 5 Years postloading. Int J Oral Maxillofac Implants 29: 1397-1405.
- Gluckman H, Toit JD, Salama M (2015) The socket-shield technique to support the buccofacial tissues at immediate implant placement. Int Dent 5: 1-7.
- Chandki R, Kala M (2012) Natural tooth versus implant: a key to treatment planning. J Oral Implantol 38: 95-100.
- Chang M, Wennström JL, Ödman P, Andersson B (1999) Implant supported single-tooth replacements compared to contralateral natural teeth. Crown and soft tissue dimensions. Clin Oral Implants Res 10: 185-194.
- Steigmann M, Monje A, Chan HL, Wang HL (2014) Emergence profile design based on implant position in the esthetic zone. Int J Periodontics Restorative Dent 34: 559-563.
- Langer B, Langer L (1985) Subepithelial connective tissue graft technique for root coverage. J Periodontol 56: 715-720.
- Reiser GM, Bruno JF, Mahan PE, Larkin LH (1996) The subepithelial connective tissue graft palatal donor site: anatomic considerations for surgeons. Int J Periodontics Restorative Dent 16: 130-137.
- Jung UW, Um YJ, Choi SH (2008) Histologic observation of soft tissue acquired from maxillary tuberosity area for root coverage. J periodontol 79: 934-940..
- Froum S, Lagoudis M, Rojas GM, Suzuki T, Cho SC (2016) New surgical protocol to create interimplant papilla: the preliminary results of a case series. Int J Periodontics Restorative Dent 36: 161-168.
- Kajiwara N, Masaki C, Mukaibo T, Kondo Y, Nakamoto T, et al. (2015) Soft tissue biological response to zirconia and metal implant abutments compared with natural tooth: microcirculation monitoring as a novel bioindicator. Implant Dent 24: 37-41.
- Gargari M, Gloria F, Cappello A, Ottria L (2010) Strength of zirconia fixed partial dentures: review of the literature. Oral Implantol (Rome) 3: 15-24.
- Rimondini L, Cerroni L, Carrassi A, Torriceni P (2002) Bacterial colonization of zirconia ceramic surfaces: an in vitro and in vivo study. Int J Oral Maxillofac Implants 17: 793-798.
- Scarano A, Piattelli M, Caputi S, Favero GA, Piattelli A (2004) Bacterial adhesion on commercially pure titanium and zirconium oxide disks: an in vivo human study. J Periodontol 75: 292-296.
- Tarnow D, Elian N, Fletcher P, Froum S, Magner A, et al. (2003) Vertical distance from the crest of bone to the height of the interproximal papilla between adjacent implants. J Periodontol 74: 1785-1788.
- Tarnow DP, Magner AW, Fletcher P (1992) The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol 63: 995-996.
- Tarnow DP, Cho SC, Wallace SS (2000) The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol 71: 546-549.
- Yu YC, Alamri A, Francisco H, Cho SC, Hirsch S (2015) Interdental papilla length and the perception of aesthetics in asymmetric situations. Int J Dent 2015: 1-5.
- Bagheri R, Burrow MF, Tyas M (2005) Influence of food-simulating solutions and surface finish on susceptibility to staining of aesthetic restorative materials. J Dent 33: 389-398.
- Kois JC (2001) Predictable single tooth peri-implant esthetics: five diagnostic keys. Compend Contin Educ Dent 22: 199-206.
- Salama H, Salama M, Garber D (2008) The tunnel technique in the periodontal plastic treatment of multiple adjacent gingival recession defects: a review. Inside Dent 4.
- Ruoff H, Terheyden H (2009) Retrospective radiographic investigation of the long-term stability of xenografts (Geistlich Bio-Oss) in the sinus. J Dental Implant 25: 160-169.