Journal of Oral Biology
Download PDF
Case Report
Case Presentation andEvolution of Concepts and Techniques in Maxillary Immediate Loading
Hafiz Adawi1*, Parnward Hengjeerajaras, Ye Shi, Shu Wei Kuo and Maryse Manasse
- Department of Periodontology and Implant Dentistry, New York University, USA
*Address for Correspondence: Hafiz Adawi, Department of Periodontology and Implant Dentistry, New York University, Clinic 5W, 345 E 24th St, New York, NY 10010, USA, Tel: +1-2025692026; E-mail: haa382@nyu.edu
Citation: Adawi H, Hengjeerajaras P, Shi Y, Kuo SW, Manasse M. Case Presentation and Evolution of Concepts and Techniques in Maxillary Immediate Loading. J Oral Biol. 2018; 5(1): 6.
Copyright: © 2018 Adawi H, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Oral Biology | ISSN: 2377-987X | Volume: 5, Issue: 1
Submission: 15 January, 2018 | Accepted: 24 May, 2018 | Published: 31 May, 2018
Abstract
Immediate loading in the maxilla is often challenging because of the poor bone quality as compared to the mandible. Moreover, the bone morphology of the maxilla may oftentimes direct the vectors of forces in a non axial direction of loading, which is detrimental for the immediately loaded implants. In literature, few studies are available with more than 3 years of evaluation of immediate loading in the maxilla. While there are several clinical factors that have been recommended for the long term success of immediate loading of the maxilla, it remains a technique sensitive procedure due to the morphology and quality of the maxillary ridge. For these reasons a new screw design, screwdriver and abutment system was introduced to correct the angulation of the implants and fabricate screw retained maxillary immediate loading prostheses. This report documents the clinical results of patients with immediately loaded implants and discusses the evolution of the surgical and restorative concepts in the fully edentulous maxilla.
Introduction
Immediate loading is defined as the loading process in which the prosthesis is attached to the implants within 1 week subsequent to implant placement or on the day of the surgery with occlusal contacts [1,2]. Immediate loading of implants in edentulous jaw provides function, esthetics, phonation and psychological satisfaction to the patient on the same day or within one week of the surgery [3]. There are numerous reports, which show that immediate loading in the mandible is a highly successful treatment modality [4,5]. However, immediate loading in the maxilla may require more planning, better patient selection, is more technique sensitive, and requires clinical experience for a successful outcome [6].
Immediate loading in the maxilla is often challenging because of the poor bone quality as compared to the mandible, where cortical bone is denser. Moreover, the bone morphology of the maxilla may oftentimes direct the vectors of forces in a non axial direction of loading which is detrimental for the immediately loaded implants. In literature few studies are available with more than 3 years of evaluation of immediate loading in the maxilla [7].
There are several clinical factors, which have been recommended to achieve predictable long term success of immediate loading in the maxilla. Recommendations included the use of rough surfaces and threaded implants to attain good primary stability [8-10]. In addition, it is recommended that an insertion torque of at least 20 Ncm should be achieved at the time of implant placement [11]. The latter has been discussed as a very critical factor for immediate loading of the implants. Splinting has been shown to limit the micro movement of the implant within acceptable limits (‹150 micron), leading to an osseointegrated bone healing rather than formation of a fibrous tissue around the implants [12]. Maxillary immediate loading is a technique sensitive procedure due to the morphology and quality of the maxillary ridge. From a prosthetic aspect, both cement and screw retained restorations are difficult to fabricate due to the potential diverse angulation of the implants. Furthermore, the channel of the screw retained restorations should be positioned within the anatomical limits of the marginal ridges and cusps of the prosthesis [13]. For these reasons, a new abutment, screw, and screwdriver system was introduced to correct the angulation of the implants and to fabricate screw retained maxillary immediate loading prostheses.
The purpose of this report was to document the step by step surgical and restorative procedure of a patient with immediately loaded implants and discuss the evolution of surgical and restorative concepts in the fully edentulous maxilla.
Materials and Methods
Clinical data in this study was obtained from the anonymous Implant Database (ID) at the Ashman Department of Periodontology and Implant Dentistry at the New York University College of Dentistry. This data was extracted as de-identified information from the routine treatment of patients. The ID was certified by the Health Insurance Portability and Accountability Act (HIPAA) and approved by the University Committee on the Activities Involving Human Subjects (UCAIHS). A computer search of electronic database from MEDLINE and PUBMED at the Waldman Library at the NYUCD was performed. Keywords such as “maxillary immediate loading”, “dental implant”, “implant angulation”, “screw retained restoration”, were used, alone and in combination, to search the databases. Non-English language publications were excluded. The search was limited to studies involving human subjects. Restrictions were not placed regarding the type of study design.
Results
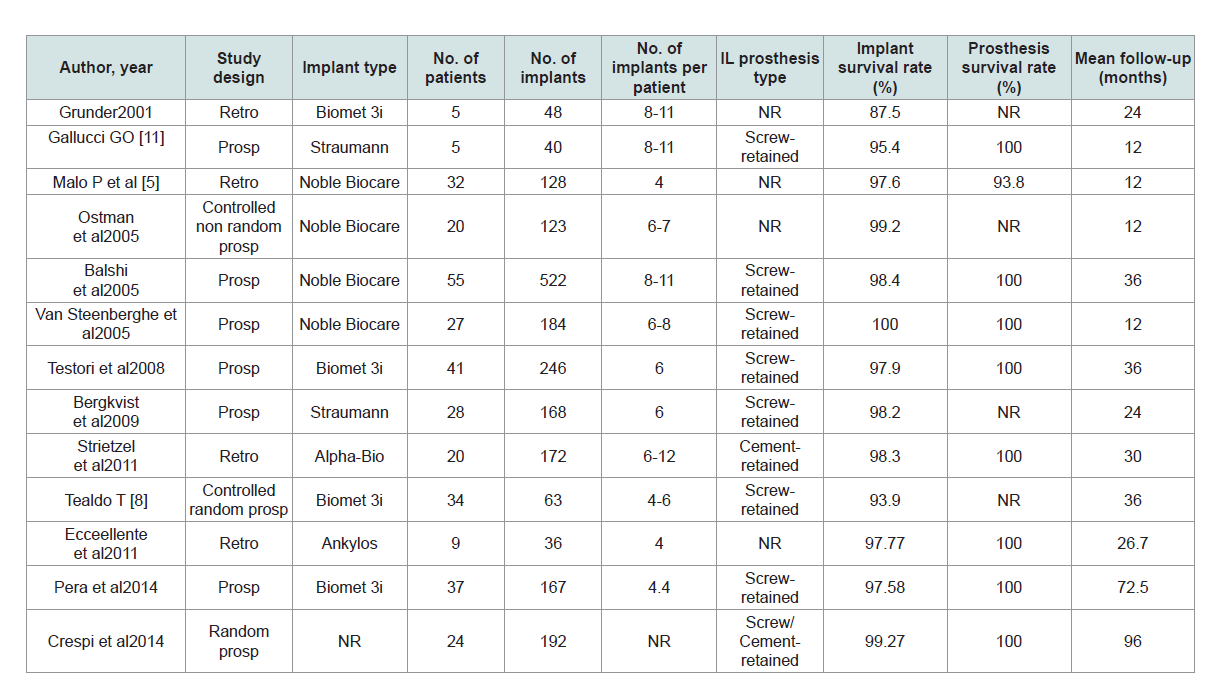
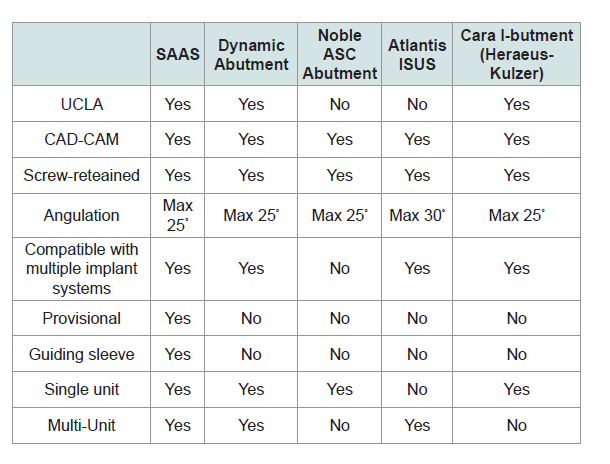
The results of this review are based on clinical findings and literature review. These are resumed and presented in Table 1. Maxillary screw retained immediate loaded provisional may significantly contribute to increase the predictability of the loading protocol and reduce the biological complication derived from the use of cement.
Case Presentation
In 2014, a 67-year-old female patient presented at the Ashman Department of Periodontology and Implant Dentistry (Figure 1). The patient was healthy, a non-smoker with an unremarkable medical history. Her chief complaint was to remove the discomfort of her existing removable complete maxillary denture and have it replaced with a fixed full arch restoration. Above all the patient’s requests was to obtain the fixed prosthesis immediately due to her low tolerance for complete dentures.
After the patient’s diagnostic assessment, the resulting treatment plan was to place seven implants in the maxillary ridge and immediately load them with a fixed full arch provisional.
Clinical procedures
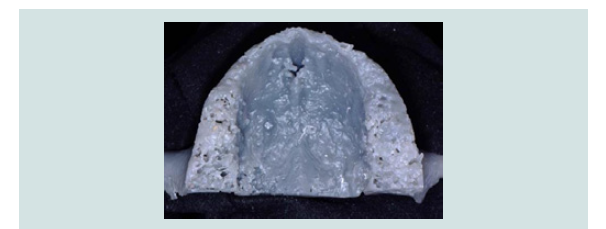
1. Clinical and radiographic examinations were made and a 3-D model of the patient’s maxilla was printed (Figures 2-4).
2. A duplicate of the patient’s maxillary complete denture was made from acrylic self curing resin (Alike, GC America, USA) to be used as provisional restoration.
3. 2 g Amoxicillin (TEVA, USA) was prescribed 1 hour prior to surgery.
4. Local infiltration anesthesia (2% lidocaine 1:100000 epinephrine, Henry Schein, USA) was given.
5. Seven implants were planned (Nobel Brånemark III 4.0x11.5 mm, Sweden) using an implant treatment software.
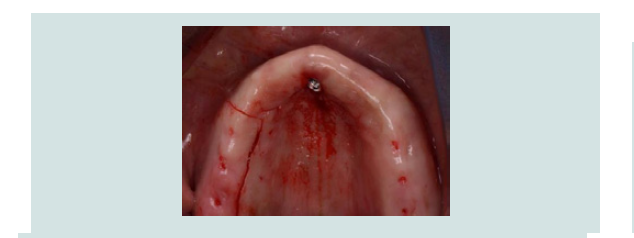
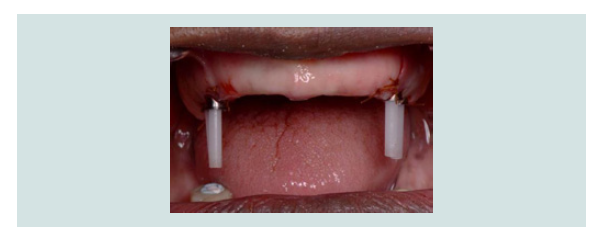
6. The first implant was placed through the soft tissue in the nasopalatine canal. Then two distal bilateral envelope incisions were made to complete the implants placement. Five of the seven implants achieved a primary stability of more than 25 Ncm and were used for the immediate loading. The residualtwo implants were then submerged (Figure 5).
Figure 5: One implant was positioned in the nasopalatine canal. The other six implants were placed in the posterior maxillary ridge. All implants were 4.0 mm in diameter and 11.5 mm in length.
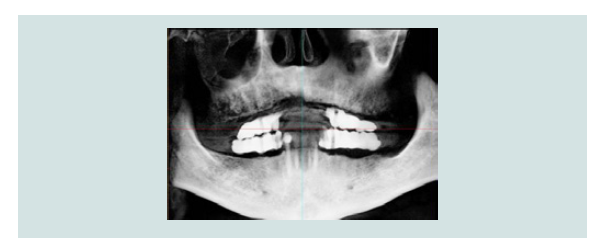
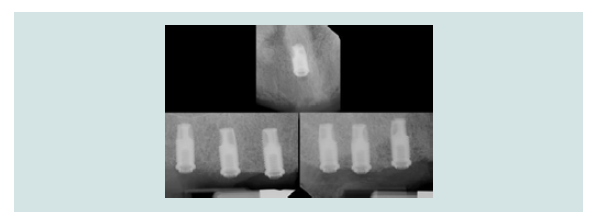
7. After the implants placement a set of periapical radiograph was taken to verify the implants angulation (Figure 6).
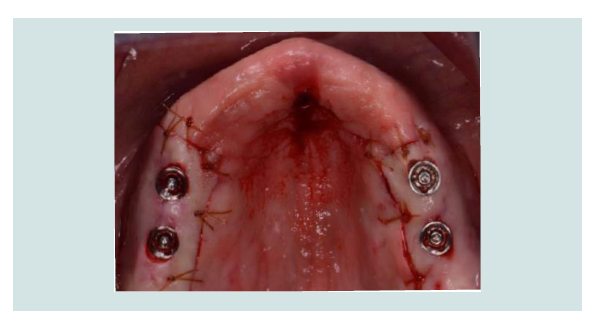
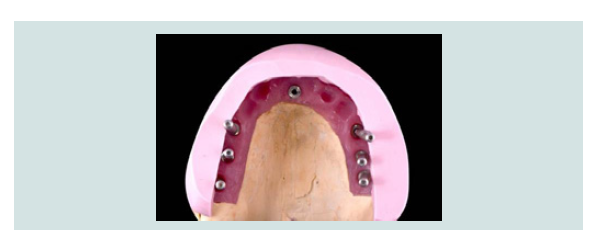
8. Five Screw-channel Adjustable Abutment Systems (SAAS) (EBI Inc, South Korea) were connected to the selected implants for immediate loading. The flap over the implants was perforated with a soft tissue puncher (Omnia, Italy) with the same diameter of the abutments to achieve an easier and a better primary closure. Sutures were performed with chromic gut 4-0 (Ethicon, USA) (Figure 7).
Figure 7: Five out of seven implants were immediately loaded. Primary closure was achieved after the insertion of the five SAAS abutments. The remaining two implants were submerged.
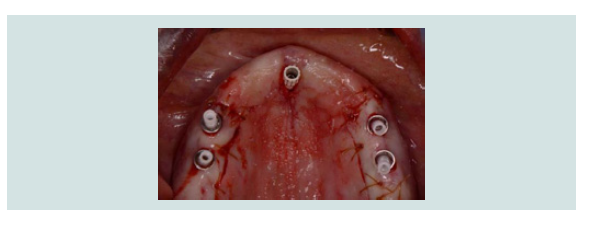
9. Five plastic sleeves were connected to the abutments. The plastic sleeves indicate the angulation of the prosthetic screw channels (Figures 8 and 9).
10. The denture duplicate was adapted to the maxilla. The SAAS plastic sleeves were positioned inside the denture duplicate emerging through the central fossa indicating the position of the screw channels. Acrylic material was injected into the space underneath the duplicated denture to pick up the abutments and plastic sleeves. After the setting of the acrylic material, the abutments were removed with the denture duplicate. The screw-retained provisional was finalized after the buccal and palatal flanges were removed from the denture duplicate, and finally inserted into the maxilla (Figure 10).
Figure 10: The provisional restoration’s screw access holes positioned in the central fossa and in the nasopalatine site.
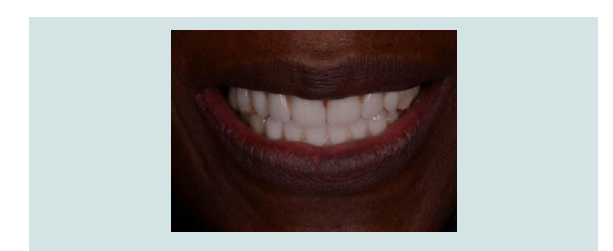
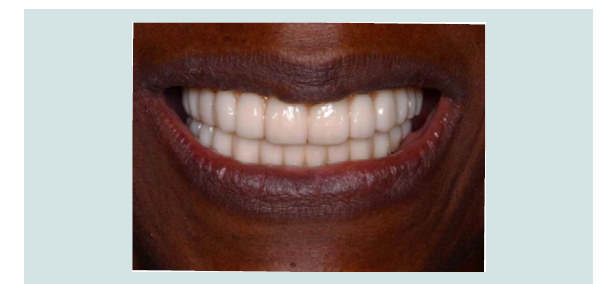
11. The provisional was finalized and polished. The patient was satisfied with the esthetics and phonetics of the provisional (Figure 11).
12. 500 mg amoxicillin were prescribed for 7 days, post-operative instructions were given and a soft diet was indicated for at least 2 months.
13. Healing was uneventful. No surgical or prosthetic complications were observed during the healing period.
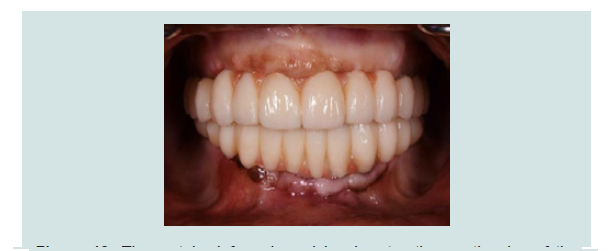
14. An impression was taken after 4 months to fabricate a metal reinforced provisional and delivered to the patient. (Figures 12-14).
Figure 12: A new metal reinforced provisional fabricated with the SAAS was delivered to the patient after 4 months of healing.
Figure 14: The patient was satisfied with the esthetic outcome and the proper function of the metal reinforced provisional.
15. Patient was recalled for periodical follow up and no surgical or prosthetic complications were observed.
Discussion
A reduced maxillary ridge is the result of alveolar bone resorption after the loss of teeth. The anterior maxillary buccal bone plate resorbs more than the palatal plate, for this reason the angulation of the implants in fully edentulous ridges cannot be often maintained parallel [14]. The posterior maxillary area, after teeth extraction, is resorbed due to a combination of alveolar resorption and Pneumatization of the sinus. In addition, maxillary bone is more trabecular and less dense compared to the mandible [15,16]. So avoiding distal cantilever is usually recommended for the immediate loading restoration in the maxilla. For these anatomical limitations immediate implant placement in an ideal position and angulation in the maxilla is more challenging compared to the mandible.
There are two procedures used to retain a fixed implant-supported restoration: screws retained or cement retained [17]. The main advantage of the screw-retained prosthesis is its retrievability. However, the occlusal screw access holes in prosthesis may compromise occlusion, porcelain strength, and esthetics [18]. A cement-retained prosthesis, on the other hand, is easier to fabricate, is more esthetic, but has more biological complications than a screw-retained restorations [19]. Some clinicians favor the use of temporary cements for retrieval, but it is likely that these restorations remain difficult to remove. Because there is no definite evidence determining which is the better approach, the choice of retention in implant prostheses is generally based on the clinician’s preference and experience. For maxillary immediate loading, however screw-retained restoration is preferred; they eliminate the need for cement, along with the associated difficulty in removing the excess from the peri-implant area that may interfere with healing and implant integration [20]. In addition, the interface of machined components is superior to any cement margin that can be developed [21]. Screw retention provides the most definitive and rigid splinting when multiple implants are used, and enhances implant primary stability [22].
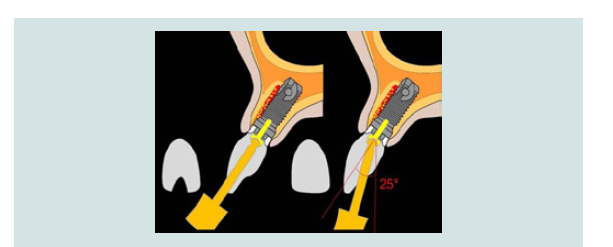
Screw-retained restorations, however, presents with a few limitations especially in the anterior maxilla. Due to the anatomic angulation of the pre-maxilla, the presence of buccal concavities, and the resorption of the maxillary alveolus towards the palate, implants placed in this region often require cement retained crowns with custom abutments to correct angulation discrepancies and prevent facial screw access holes. The SAAS consists of four components: a titanium abutment, a plastic sleeve, a special screw and screwdriver (Figure 15). With the SAAS, the screw channel can be angulated up to 25 degrees from the screw axis in order to position the prosthesis access hole in the ideal point regardless of the implant angulation (Figure 16). In the present case, due to the limitation of the maxillary ridge morphology the implants were placed divergent from each other (Figure 17). With the SAAS the screw access holes of the prosthesis were properly positioned in the central fossa (Figure 18). Other angulated abutments and prosthetic components are also available in the market and their advantages and disadvantages are compared in Table 2.
Figure 16: The SAAS four components: titanium abutment, plastic sleeve, special screw and screwdriver.
Figure 17: The guide pins were connected with the implant analog on the master cast showing the divergent implants angulations.
Figure 18: The SAAS allows the position of the screw channel of the prosthesis to be parallel and the screw holes to be positioned in the central fossa.
In particular situations, if the maxillary anterior teeth are periodontal compromised immediate loading is not possible due to the risk of infection and prominent maxillary bone loss. Consequently, anchorage of implants in the remaining bone around the incisive canal can be considered as an option to provide sufficient anterior support to enhance the biomechanics of implant supported prosthesis [23]. The incisive canal can be considered as a treatment option for previously failed implants or grafting in the anterior maxilla. However, it is still difficult to achieve passive-fit framework because of the different angulation of implants.
Nowadays, more and more clinicians use computer-guided surgery for immediate loading in complete edentulous maxilla. However, there is still a learning curve not only in the surgery but also with the software [24]. Moreover, according to a systematic review by Hultin M et al. there are some complications such as the misfit of surgical guides and immediate provisional prostheses due to the error in the interocclusal registration or software [25].
Conclusion
This case report documented a novel abutment system that allowed the fabrication of restorations with screw access holes positioned in the central fossa of molars and premolars, and one implant positioned in the naso-palatine canal for maxilla immediate loading protocol. While this new approach addresses the difficulties in fabrication and enhances the maxillary immediate loading procedures, long-term follow-up and more clinical studies are still needed.
Acknowledgement
Special thanks to Drs. Arun Vidyadharan DDS and Sousa Soares Ricardo DDS for their contribution of clinical cases and revision of the manuscript.
References
- Adell R, Lekholm U, Rockler B, Brånemark PI (1981) A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg 10: 387-416.
- Branemark PI, Hansson BO, Adell R, Breine U, Lindström J, et al. (1977) Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl 16: 1-132.
- Aparicio C, Rangert B, Sennerby L (2003) Immediate/early loading of dental implants: a report from the Sociedad Española de Implantes World Congress consensus meeting in Barcelona, Spain, 2002. Clin Implant Dent Relat Res 5: 57-60.
- Horiuchi K, Uchida H, Yamamoto K, Sugimura M (2000) Immediate loading of Brånemark system implants following placement in edentulous patients: a clinical report. Int J Oral Maxillofac Implants 15: 824-830.
- Malo P, Rangert B, Nobre M (2003) “All-on-four” immediate function concept with Brånemark System implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res 5 Suppl 1: 2-9.
- Crespi R, Capparè P, Gherlone E, Romanos GE (2007) Immediate occlusal loading of implants placed in fresh sockets after tooth extraction. Int J Oral Maxillofac Implants 22: 955-962.
- Jaffin RA, Kumar A, Berman CL (2000) Immediate loading of implants in partially and fully edentulous jaws: a series of 27 case reports. J Periodontol 71: 833-838.
- Tealdo T, Bevilacqua M, Menini M, PeraF, Ravera G, et al. (2011) Immediate versus delayed loading of dental implants in edentulous maxillae: a 36-month prospective study. Int J Prosthodont 24: 294-302.
- Maló P, Rangert B, Nobre M (2005) All-on-4 immediate-function concept with Bränemark System implants for completely edentulous maxillae: a 1-year retrospective clinical study. Clin Implant Dent Relat Res 7 Suppl 1: S88-S94.
- Brunski JB (1999) In vivo bone response to biomechanical loading at the bone⁄dental implant interface. Adv Dent Res 13: 99-119.
- Gallucci GO, Benic GI, Eckert SE, Papaspyridakos P, Schimmel M, et al. (2014) Consensus statements and clinical recommendations for implant loading protocols. Int J Oral Maxillofac Implants 29 Suppl: 287-290.
- Rangert BR, Sullivan RM, Jemt TM (1997) Load factor control for implants in the posterior partially edentulous segment. Int J Oral Maxillofac Implants 12: 360-370.
- Duyck J, Van Oosterwyck H, Vander Sloten J, De Cooman M, Puers R, et al. (2000) Magnitude and distribution of occlusal forces on oral implants supporting fixed prostheses: an in vivo study. Clin Oral Implants Res 11: 465-475.
- Pietrokovski J, Massler M (1967) Alveolar ridge resorption following tooth extraction. J Prosthet Dent 17: 21-27.
- Jaffin RA, Berman CL (1991) The excessive loss of Brånemark fixtures in type IV bone: a 5-year analysis. J Periodontol 62: 2-4.
- Misch CE (2007) Density of bone: effect on treatment plans, surgical approach, healing, and progressive boen loading. Int J Oral Implantol 6: 23-31.
- Taylor TD, Belser U, Mericske-Stern R (2000) Prosthodontic considerations. Clin Oral Implants Res 11 Suppl 1: 101-107.
- Hebel KS, Gajjar RC (1997) Cement-retained versus screw-retained implant restorations: achieving optimal occlusion and esthetics in implant dentistry. J Prosthet Dent 77: 28-35.
- Sailer I, Mühlemann S, Zwahlen M, Hämmerle CH, Schneider D (2012) Cemented and screw retained implant reconstructions: a systematic review of the survival and complication rates. Clin Oral Implants Res 23 Suppl 6: 163-201.
- Shadid R, Sadaqa N (2012) A comparison between screw- and cement-retained implant prostheses. A literature review. J Oral Implantol 38: 298-307.
- Lee A, Okayasu K, Wang HL (2010) Screw- versus cement-retained implant restorations: current concepts. Implant Dent 19: 8-15.
- Chee W, Jivraj S (2006) Screw versus cemented implant supported restorations. Br Dent J 201: 501-507.
- Peñarrocha D, Candel E, Guirado JL, Canullo L, Peñarrocha M (2014) Implants placed in the nasopalatine canal to rehabilitate severely atrophic maxillae: a retrospective study with long follow-up. J Oral Implantol 40: 699-706.
- Merli M, Bernardelli F, Esposito M (2008) Computer-guided flapless placement of immediately loaded dental implants in the edentulous maxilla: a pilot prospective case series. Eur J Oral Implantol 1: 61-69.
- Hultin M, Svensson KG, Trulsson M (2012) Clinical advantages of computer-guided implant placement: a systematic review. Clin Oral Implants Res 23 Suppl 6: 124-135.