Journal of Oral Biology
Download PDF
Research Article
Efficacy of 0.75% Boric Acid and 0.2% Chlorhexidine Subgingival Irrigation as an Adjunct to Scaling and Root Planing In the Treatment of Gingivitis. A Comparative Clinico-Microbiological Study
Tasneem N, AN Savitha, Jayaram P and AR Pradeep*
The Oxford Dental College, Bangalore, India
*Address for Correspondence: AR Pradeep, The Oxford dental college, 10th milestone, Hosur Road, Bommanahalli, Bangalore-560068, Karnataka, India, Email: periodonticsgdcri@gmail.com
Submission: 21 May, 2019;
Accepted: 29 June, 2019;
Published: 31 July, 2019;
Copyright: © 2019 Tasneem N et al. This is an open access article
distributed under the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited.
Abstract
Aim: Boric acid has been reported to have antibacterial and antiinflammatory
properties. The purpose of this study was to evaluate the
effects of 0.75% boric acid irrigation as an adjunct to scaling and root
planing on clinical and microbiological parameters and compare this
method with 0.2% chlorhexidine and saline irrigation in patients with chronic
gingivitis.
Methods: 60 patients were recruited and divided equally into three
groups: I. Saline group, II.0.2% chlorhexidine group and III. 0.75% boric acid
group. Subgingival plaque samples were collected after supragingival
scaling, prior to subgingival irrigation and processed immediately for
analysis of Porphyromonas gingivalis and Prevotella intermedia. At baseline,
2 weeks and one month after SRP, clinical parameters including plaque
index, gingival index, sulcular bleeding index, probing pocket depth were
assessed along with the subgingival plaque sample.
Results: Significant reduction in clinical parameters and mean levels
of Porphyromonas gingivalis and Prevotella intermedia were noted at 2
weeks and one-month in all treatment groups. A significantly greater mean
reduction of Porphyromonas gingivalis was found in the 0.75% boric acid
group.
Conclusion: 0.75% boric acid irrigation could be considered as an
adjunct to scaling and root planning in the treatment of patients with
moderate to severe gingivitis.
Keywords
Anti-infective agents; Boric acid; Chlorhexidine; Gingivitis; Root
planning
Introduction
Periodontal diseases are inflammatory conditions of infectious
nature. The unequivocal role of dental bacterial plaque in the
development of these diseases was established almost 40 years ago
[1]. Although, development of gingivitis after plaque accumulation
appears to be a universal finding, the rate of development and the
degree of the clinical inflammatory response is variable between
individuals, even under similar plaque accumulation conditions.
It is generally accepted that the goal of initial periodontal therapy is to restore the biological compatibility of periodontally diseased
root surfaces. While non-surgical periodontal therapy aims to
eliminate pathogenic bacteria in the bio films, complete elimination
remains elusive. Meticulous subgingival debridement is inherently
time-consuming and difficult procedure that usually includes scaling
and root planning by manual instrumentation and/or periodontal
debridement with sonic or ultrasonic scalers [2]. However, its success
relies heavily on the skill of the clinician.
Since most patients are not skilled in adequate plaque
removal, many clinicians currently include one or more adjunctive
chemotherapeutic agents in their nonsurgical anti-infective regimen.
The primary objective of supragingival irrigation is to flush away
bacteria coronal to the gingival margin, thereby diminishing the
potential of developing gingivitis or decreasing existing gingival
inflammation. In contrast, subgingival irrigation attempts to directly
reduce the pocket microflora to prevent initiation of periodontal
diseases or to facilitate their reduction. Therefore, procedures
of eliminating periodontal pathogens are of great interest, and
considerable attention has been devoted to the possibility of using
antibiotics or antiseptics in this respect [3]. Antimicrobials, including
povidone-iodine and chlorhexidine, have been used with limited
success in the treatment of periodontal diseases as a result of potential
toxicity and the unique anatomy of the periodontal pocket. Other
treatment modalities include systemic anti-microbial therapy, locally
placed subgingival anti-infective agents, full mouth disinfection,
chlorhexidine rinsing after debridement, topical anti-microbials and
intra-oral irrigation with and without chemotherapeutic agents.
Antibacterial activity of boron, which is a bioactive trace element
and frequently found in diets plentiful in foods such as fruits,
vegetables, and nuts, has been reported to have a regulatory effect in
the inflammatory and immune response [4,5]. A boron-containing
compound (AN0128) was also recently reported to have both
antibacterial and anti-inflammatory properties [6]. It has been shown
to reduce the formation of inflammatory infiltrate and bone loss in
rats measured histologically and by micro-computerized tomography.
Furthermore, it has been noted that it has in-vitro activity against
some bacteria associated with periodontal disease, namely, Prevotella
intermedia, Porphyromonas gingivalis, Eubacterium nodatum, and Treponema denticola. It has been stated that boric acid could be an
alternative to chlorhexidine, and it might be more favorable because
boric acid was superior in reducing the bleeding on probing, pocket
depth and clinical attachment loss reductions for moderate pockets
in the early healing phase [7]. The effects of 0.75% boric acid gel were
recently evaluated when delivered subgingivally and was shown to
promote bone formation in intrabony defect sites, thereby reducing
PPD and clinical attachment level [8]. Similar improvement was seen
in class II furcation defects where 0.75% boric acid gel was placed and
a significant percentage of bone fill was observed [9].
In light of the above-stated evidence, the present study was
designed to determine the effect of subgingival 0.75% Boric Acid (BA)
irrigation as an adjunct to Non-Surgical Periodontal Therapy (NSPT)
compared with 0.2% Chlorhexidine (CHX) and saline solutions on
clinical and microbiological parameters in patients with chronic
gingivitis.
Materials and Methods
Source of data:
In this longitudinal, interventional study, 60 systemically healthy
patients presenting to the Department of Periodontology, The Oxford
Dental College, Bangalore, Karnataka, India fulfilled the selection
criteria and recruited for the study. The entire nature and scope of
the study were explained in detail to all subjects participating in the
study and informed consent was obtained. The study was conducted
according to the 1975 Helsinki Declaration, as revised in 2000, and
was approved by the institutional ethics committee of the Oxford
Dental College, Bangalore (synopsis no.: 02_D026_63558).Selection criteria:
Patients included in the study were selected based on the inclusion
criteria: (a) age group of 18-40 years who were systemically healthy
individuals, (b) presence of minimum of 20 teeth, (c) presence of
moderate to severe gingivitis {Plaque Score (PI) score ≤ 3, Gingival
Index (GI) score ≤ 3, Sulcular Bleeding Index (SBI) ≤ 5 and Probing
Pocket Depth (PPD) ≤ 3mm}, (d) no history of periodontal therapy
or antibiotic or anti-inflammatory therapy in the past 12 months, (e)
history of compliance with oral hygiene instructions and periodic
recall and (f) radiographic analysis should show absence of alveolar
bone loss.Patients were excluded if they presented with systemic disorders
and platelet disorders, have used any mouth rinse within the last 3
months, smokers, pregnant or lactating mothers and any use of
hormone contraceptives.
Patients satisfying the selection criteria were assigned via
computer-generated software, into three treatment groups: I. SRP+
saline irrigation, II. SRP+ 0.2% CHX irrigation, III. SRP+ 0.75%
BA irrigation. All clinical parameters pre- and post- treatment were
recorded by a single clinician who also provided treatment to all the
groups. Patients were masked for allocation into the treatment groups.
The clinical parameters assessed at baseline, 2 weeks and one month
following SRP included PI [10], GI [11], SBI [12], and PPD. William’s
periodontal probe was used to standardize the measurement of the
clinical parameters.
Primary and secondary outcome measures:
The primary outcomes of the study included the PI, GI and SBI
score, while the secondary outcome included PPD and bacterial
counts difference.Formulation of 0.75% boric acid irrigant solution:
Based on the in-vitro cytotoxicity experiments performed in a
previous study, 0.75% concentration of BA solution was decided to
be used for subgingival irrigation 7]. The formulation was prepared
similar to the study by Saglam et al., by dissolving the weighed amount
of BA in distilled water.Clinical treatment:
SRP was performed thoroughly using an ultrasonic scaler at
baseline, following the collection of subgingival plaque. Subgingival
irrigation was performed immediately after SRP with 10 ml of
experimental irrigant (saline solution, 0.2% CHX or 0.75% BA) for
1 min at selected sites using a blunted needle and syringe. After
irrigation, the patients received oral hygiene instructions which were
reinforced at each revisit.Plaque sample collection:
Prior to SRP and subgingival irrigation, subgingival pooled plaque
samples were Atraumatically collected at baseline, and following SRP
at 2 weeks and one-month. This was performed by inserting a sterile
Gracey curette using a gentle pull-stroke into the selected subgingival
crevice which was properly isolated with cotton and gently dried with
compressed air to prevent contamination from saliva. The plaque
sample was transferred immediately into Reduced Transport Fluid
(RTF).Microbial analysis:
After collection of the plaque sample in the RTF solution, it was
vortexed and then diluted to 1:10 proportion. Following which, it
was inoculated in the culture medium. The medium chosen for the
cultivation of P. gingivalis and P. Intermedia was blood agar which
consisted of Brucella agar with hemin and vitamin K. The selectivity
for P. intermedia was enhanced by the addition of kanamycin and
vancomycin. A similar methodology was followed in earlier studies
by Pfau et al. and Nakayama K. [13,14]. Following the inoculation, the
blood agar was incubated at 37 °C for 3-4 days in a strictly anaerobic
environment provided by an anaerobe jar. Once the incubation was
completed, the plates were removed and the colony characters were
identified by gram staining technique and quantified by counting of
the colony forming units.Statistical analysis:
To achieve 95% power of the study, 20 patients were recruited
into each treatment group and this sample size was calculated based
on data from previous studies [7]. Data were statistically analyzed
using SPSS version 20.0 (IBM, Chicago, IL, USA). The following
statistical tools were used to analyze the data: mean and confidence
interval. One-way ANOVA was done for the comparison between the
three groups. While paired t-test was done to statistically compare
the parameters in each group separately. A p-value of <0.05 was
considered to be statistically significant.
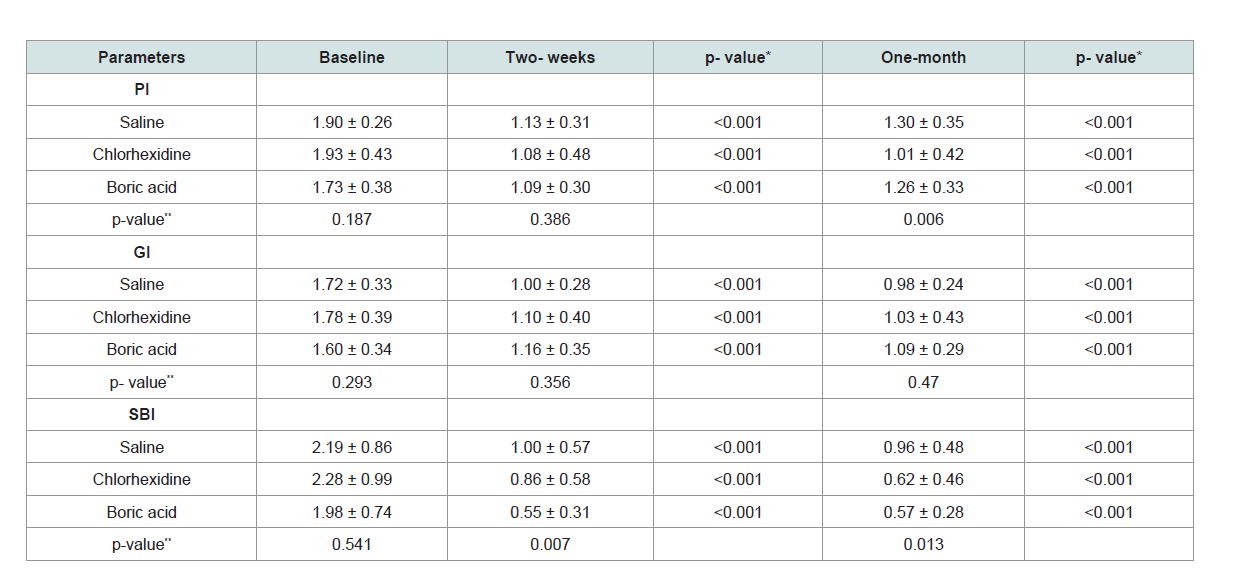
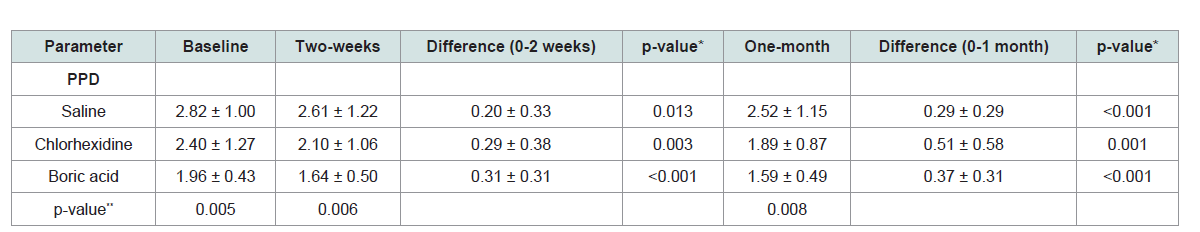
Table 1: Comparison of whole-mouth clinical parameters at baseline, two weeks and one-month (mean ± SD).
Results
At the end of the one-month trial period, no adverse reactions
to the experimental irrigant solutions were reported from the 60
patients who completed the study. A significant reduction in clinical
parameters in all the treatment groups from baseline to one-month
was noted, but on the comparison between the groups, no statistically
significant difference was found for levels of GI, SBI and PPD (Table 1 and 2). However, a statistically significant reduction was observed in
PI for 0.2% CHX group, when compared to the 0.75% BA group and
saline group (p = 0.006) (Table 1).
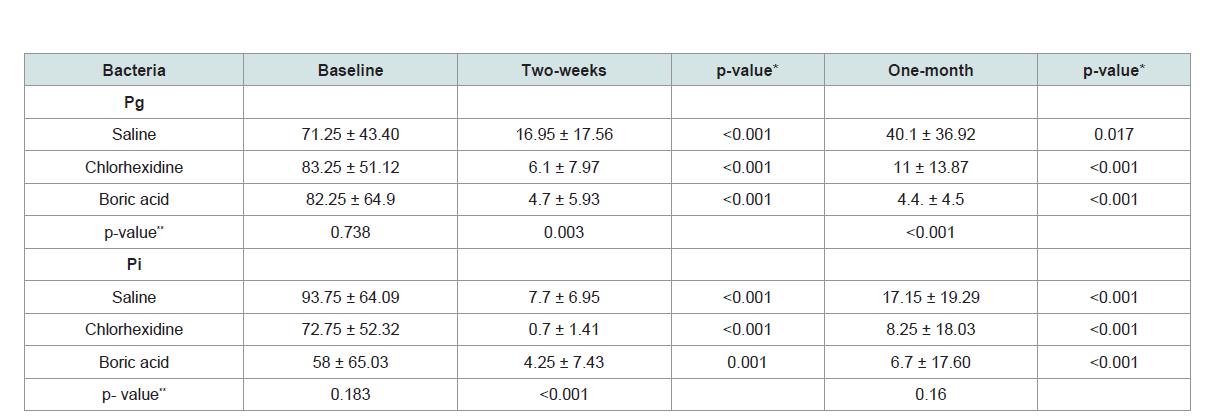
The mean levels of P. gingivalis and P. intermedia have shown
a statistically significant reduction in all the treatment groups. On
comparison of the mean reduction levels of P. gingivalis between the
three groups, it was observed that 0.75% BA group had the greatest
reduction which was statistically significant (p = 0.023). The same was,
however, not observed for the mean level reduction in P. intermedia
which was statistically insignificant for the three groups (Table 3).
Discussion
In this study, the additive effects of 0.75% BA as an alternative adjunct to 0.2% CHX and saline sub-gingival irrigation were compared
on the basis of clinical and microbiological parameters in patients
with gingivitis. The levels of two common periodontal pathogens, i.e.
P. gingivalis and P. intermedia were assessed to determine the efficacy
of the irrigants at the end of two weeks and one month.
The mean levels of the clinical parameters: GI, SBI, and PPD
showed a significant decrease in all the treatment groups. This
improvement in the gingival inflammatory condition shows the
potent anti-inflammatory action of BA, which is in accordance with
the studies by Kanoriya et al. and Singhal et al. [8,9]. However, no
statistically significant differences were observed between the three
groups. Braatz et al. and Watts et al. had found similar results, where
they concluded that adjunctive irrigation with CHX did not provide
any additional clinical benefit when compared with conventional
treatment [15,16].
In the present study, the mean difference of PI values between
the three groups at the end of one-month revealed that 0.2% CHX
group had the highest value of 0.9175 and 0.75% BA group had the
least value of 0.4705 and this difference was statistically significant (p
value=0.006). These results were similar to other research by Walsh et al and Mohammadi and Abbot [17,18]. The superior effect of CHX
can be attributed to its substantive nature which helps maintain
a potent sustained release and ability to help inhibit adherence
of microorganisms to a surface thereby, preventing growth and
development of biofilms [17,18].
The mean microbial levels of P. gingivalis and P. intermedia decreased significantly in all the groups after treatment. The reduction in the mean levels of P. gingivalis between baseline and one-month were statistically significantly higher in 0.75% BA group when compared to saline group and 0.2% CHX group (p = 0.023). This reduction in P. gingivalis levels can be attributed to the antibacterial and anti-inflammatory effects of boric acid as mentioned by Luan et al. who reported that boron-containing compound AN0128 showed activity againstsome bacteria associated with periodontal
disease, i.e P. intermedia, P. gingivalis, E. nodatum and T. denticola with minimum inhibitory concentrations of <0.5 mg/mL [6]. The superiority of BA to CHX can be explained by the decreased antibacterial effect of CHX when exposed to serum proteins in the GCF [19]. Grenier et al. reported that P. gingivalis releases vesicles that bind to and inactivate chlorhexidine, thus protecting themselves from that agent. Due to its unique physicochemical characteristics, antiinflammatory
properties and minimally genotoxic effect on bacteria, boron has gained significant attention in the medical area [20].
The reduction in P. intermedia was statistically not significant (p>
0.05). This result is in accordance with the study by Saglam et al. who
reported no significant differences between 0.75% BA and 0.2% CHX
subgingival irrigation in terms of reduction of perio pathogens [7].
The concentration of BA was safely used based on the results of
in-vitro cytotoxicity experiments conducted by Saglam et al. it was
decided to use 0.75% concentration of BA (pH= 4.9) in this clinical
study. Only three higher concentrations of BA (6%, 3%, and 1.5%)
reduced cell survival of human periodontal ligament fibroblasts and
human gingival fibroblasts significantly [7]. This concentration was
similarly used in gel form in previous studies without any adverse
reactions [8,9]. In contrast, Alleyn et al. demonstrated the exposure of
root surfaces to 0.12% CHX which significantly inhibited subsequent
fibroblast attachment, therefore impeding regeneration of the
periodontium. CHX was found to be highly cytotoxic for human periodontal ligament cells by inhibiting double-stranded nucleic
acid content, protein synthesis, and mitochondrial activity [21]. In a
study by Pucher and Daniel, CHX was demonstrated to be cytotoxic
for human fibroblasts via inhibition of protein synthesis [22]. In the
present study, no additional effect of 0.2% CHX to conventional
treatment for PPD in the early healing period was observed. This
might be a result of the cytotoxic and inhibitory effect of CHX on the
fibroblasts. In a study by Arabaci et al. in 2013, the results showed
a dose-dependent genotoxic and cytotoxic effect of CHX on human
lymphocytes in vitro and therefore, concluded that periodontal
irrigation should be done with lower concentrations of CHX [23].
As reported by Ince et al., boric acid prevents oxidative damage
by increasing an antioxidant agent, glutathione, and its analog and
by promoting other neutralizing agents of reactive oxygen species
[24]. This may be the reason why significant reduction in PPD was
observed in 0.75% BA group.
This present study was the first study conducted on patients
suffering from gingivitis. The follow-up period was only of one-month
duration and this was one of the limitations of the study. Studies with
a longer duration may be required to evaluate the longevity of the
effect of the irrigants. Another important shortcoming of the study
is the method used to detect the periodontal pathogens. The bacterial
culture method with an accuracy of 61-79% is considered to be least
reliable [25]. Hence, more accurate methods, such as DNA probes
could enhance the results of this study.
Conclusion
Within the limits of the study, the present investigation shows
that the use of 0.75% BA or 0.2% CHX as an adjunct to NSPT did not
reveal any statistically significant differences in clinical parameters
compared with conventional treatment. The adjunctive 0.75% BA
irrigation, however, produced beneficial improvement in the levels of
P. gingivalis. Hence, SRP with 0.75% BA irrigation can be considered
as an adjunctive approach in the treatment of moderate to severe
gingivitis. Longitudinal, multicenter, randomized, controlled clinical
trials are, however, required to confirm the findings of the present
study.
Acknowledgement
The authors thank Dr. C.M. Setty (Professor and Head of
Department), Department of Pharmaceutics, the Oxford College
of Pharmacy, Bangalore for providing the necessary formulation
of boric acid. The authors also express their gratitude to Dr.
Kishore Bhat (Professor and Head of department), Department of
Microbiology, Maratha Mandal’s: Nathajirao G. Halgekar Institute
of Dental sciences and Research centre, Belagavi for providing
the facilities necessary to carry out plaque sample testing in their
Laboratory.