Journal of Oral Biology
Download PDF
Case Report
Full Mouth Reconstruction in a Diabetes Mellitus Type I Patient – A Case Report with 5 Years Follow-Up
Braz de Oliveira R, Gaspar J, Reis N* and Fernández-Guallart I
Department of Periodontology and Implant Dentistry, New York
University, New York, USA
*Address for Correspondence: Reis N, Department of Periodontology and Implant Dentistry, New York University, C/O Dr Paul YC Yu, Clinic 5W, 345 E 24th St, NY 10010, New York, USA Tel: +1-347 279 29 58; E-mail: ycy233@nyu.edu
Submission: 28-10-2019
Accepted: 26-11-2019
Published: 30-11-2019
Copyright: © 2019 Oliveira RB, et al. This is an open access article
distributed under the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited.
Abstract
Periodontal disease is one of the most common oral diseases, caused
by a combination of poor oral hygiene and host defense response. It can be
infl uenced by genetic, environmental and/or developed conditions such as
smoking and diabetes mellitus. Periodontitis leads to bone resorption and
has a reported relationship with peri-implantitis development and implant
failure. However, when sugar levels are controlled, even diabetic patients
can have a long-term success and survival of dental implants. In addition,
the patient’s ability to maintain a good oral hygiene has been reported as
a critical factor to achieve that goal. Dental implants are a good option
for these patients, although there are some factors that should be ensured
prior to the treatment, such as improvement and maintenance of oral
hygiene levels, compliance in disease-control and quitting or reducing of
smoking. The purpose of this case report with 5 years follow-up is to review
the importance of motivation, education and maintenance in a patient
who received dental implants as a type I diabetic with a history of chronic
heavy smoking and poor oral hygiene.
Introduction
Periodontal disease is a chronic infl ammatory disease that aff ects
the periodontium. It is one of the most common oral diseases, caused
by a combination of poor oral hygiene and host defense response,
and can be infl uenced by genetic, environmental and/or developed
conditions such as smoking and diabetes mellitus. Periodontitis
leads to bone resorption, which, without proper maintenance, can
ultimately lead to a hopeless prognosis [1,2].
In cases of partial or complete edentulism, osseointegrated
implants as a support for dental prostheses are a viable treatment
option to replace the missing teeth which nowadays is becoming
more accepted due to its high success rate. However, mechanical and
biological risk factors can cause implant failure. Mechanical factors
pertain to implant characteristics such as body design and surface
architecture, while biological factors involve host aspects like chronic
heavy smoking (more than 10 cigarettes a day), diabetes mellitus, or
presence of periodontal disease. In literature, these biological factors
are considered as relative contraindications for dental implants [3-5].
Smoking can aff ect wound healing due to the decrease in blood
supply in periodontal tissues and therefore infl uences the bone
quality. However, it is reported in the literature that reducing the
number of cigarettes can decrease the complications with dental
implants [6].
Diabetes mellitus type I is characterized by high glucose levels
in the blood due to lack of insulin production, which hinders host
resistance. Th is consequently delays wound healing and increases
the risk of infection specially in the soft tissue. However, literature
reports that diabetic patients with controlled sugar levels can have a long-term success and survival of dental implants [7]. Likewise, the
patient’s ability to maintain a good oral hygiene has been reported as
a critical factor in achieving that goal.
Early loss of teeth due to periodontal disease can be associated
both with diabetes mellitus type I and chronic heavy smoking habits.
Young patients that started to lose their teeth due this condition are
worried about esthetics, and they are not compliant in using removable
dentures as they prefer fi xed prostheses. Dental implants are a good
option for these patients, although there are some factors that need
to be considered prior to the treatment, such as improvement and
maintenance of oral hygiene levels, compliance in disease-control
and quit/reduce smoking.
Th e purpose of this case report with 5 years follow-up is to
review the importance of motivation, education and maintenance in
a patient who received dental implants as a type I diabetic, with a
history of chronic heavy smoking and poor oral hygiene.
Materials and Methods
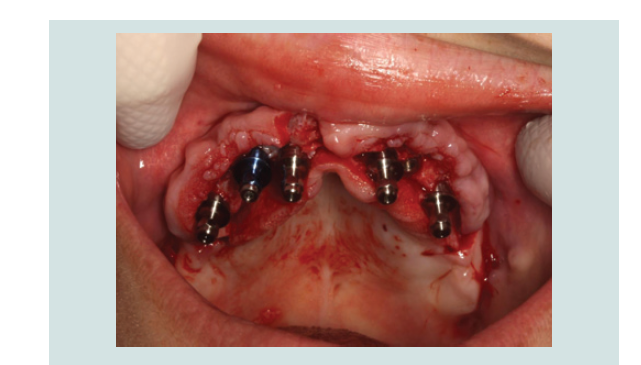
A 31 year old Caucasian female patient presented in the private clinic in 2011 with the chief complaint “I want to replace my teeth with some fi xed restoration, not removable”. Th e medical, social and dental history of the patient were reviewed: she had diabetes type I (HbA1c was 6.7%) and was taking insulin as medication to control the disease. Furthermore, she was a chronic heavy smoker (15-20 cigarettes per day) and reported that she already had some teeth extracted due to generalized periodontal disease (Table 1). At that time, she was using a removable partial denture, but she was not comfortable with it. Aft er comprehensive examination, the proposed treatment plan included extraction of all the remaining teeth and replacement with dental implants and a fi xed hybrid prosthesis in both arches. Th e patient understood the pros and cons of the treatment, agreed, and signed the consent form to proceed with the presented treatment plan.
Before starting with the surgical treatment, the patient was
advised that the diabetes mellitus should be well controlled, so when
she came for surgery her HbA1c levels were 6.1%. In November of
2012, the fi rst surgery was performed, consisting of extraction of the
remaining maxillary teeth followed by the delivery of an immediate
removable complete denture. For the mandible, the treatment
included extractions, immediate implant placement and immediate
provisionalization. One hour before the surgical procedure, the
patient took 2g of amoxicillin with clavulanic acid as prophylaxis.
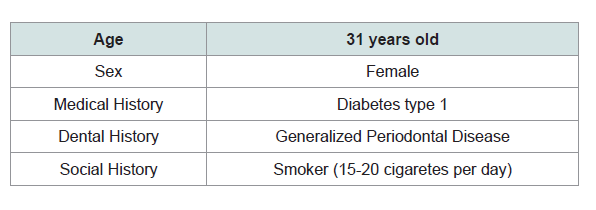
Th e procedure was carried out under local anesthesia (4% articaine with 1:100000 epinephrine, Inibsa, Portugal). Aft er anesthesia was
achieved, the teeth were atraumatically extracted using periotomes,
elevators and forceps. In the mandible, a midcrestal incision from
right fi rst molar to left fi rst molar areas was made and a full-thickness
fl ap was refl ected. Five implant sites were prepared following the
protocol established by the manufacturer, and immediate implants
were placed in the osteotomies (3 SIN 4.0 x 10 mm and 2 Biomet 3i
Osseotite 3.25/4 x 10 mm). Aft er that, temporary cylinders were placed
in four of the fi ve implants and a metal-reinforce acrylictemporary
was delivered and immediately loaded. Primary closure of the fl ap
was achieved with 4/0 silk sutures (Inibsa, Portugal). A maxillary
immediate removable complete denture was delivered, and a
mandibular immediate complete denture was screwed in. Th e patient
was prescribed antibiotic (amoxicillin 875mg with 125mg clavulanic acid every 12h for one week), analgesic (ibuprofen 600mg every 8h as
needed) and mouth rinse (0,12% chlorhexidine for 10 days). Aft er 1
week, she came back for a follow-up and the sutures were removed.
Th e healing process was uneventful, with no infection, infl ammation
or pain.
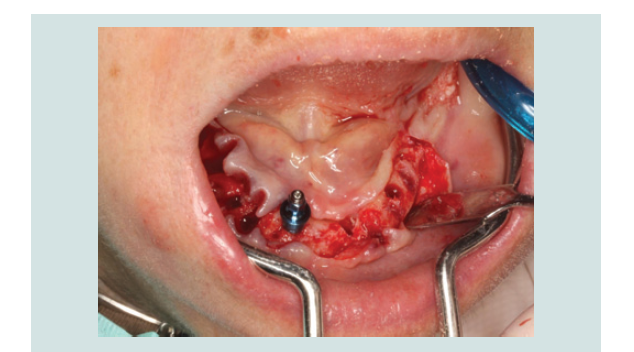
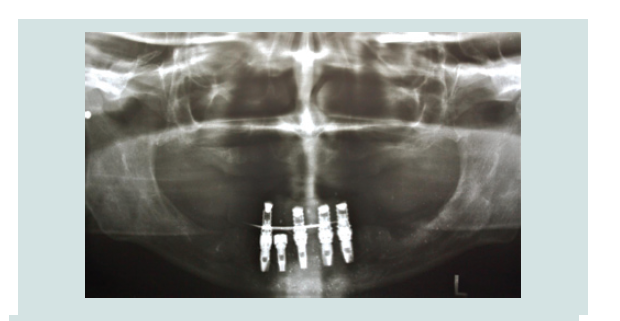
In March of 2013, a second surgery was performed in order to
place six implants in the maxilla. Th e same pre-operative and surgical
protocol was followed, and in this case a vertical incision was made
in the midline to facilitate the refl ection of the full-thickness fl ap. Six
implants were placed (2 SIN 4.0 x 10 mm implants and 4 EBi 4 x 4.1 x
8.5 mm implants) and submerged with cover screws. Primary closure
of the fl ap was achieved with 4/0 silk sutures (Inibsa, Portugal). Th e
patient continued to use the maxillary removable complete denture aft er relining it. Th e same post-operative protocol and instructions
were given to her, and in the follow-up visit the healing was again
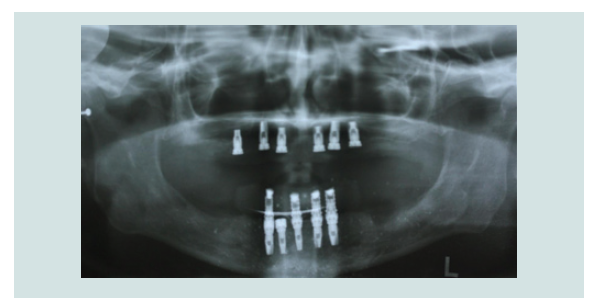
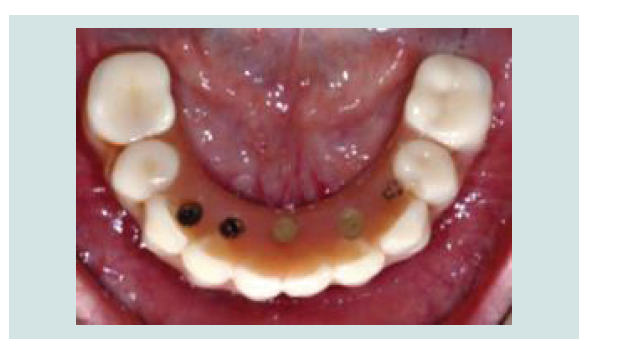
favorable (Figure 1-9).
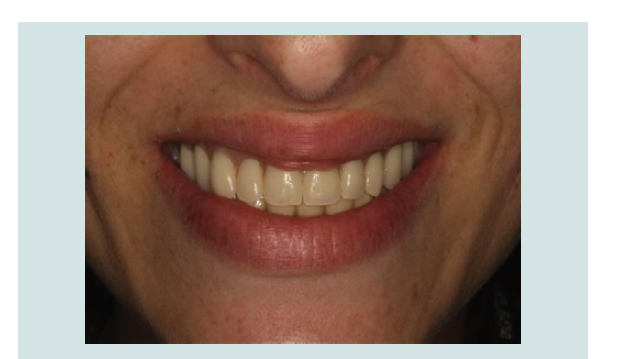
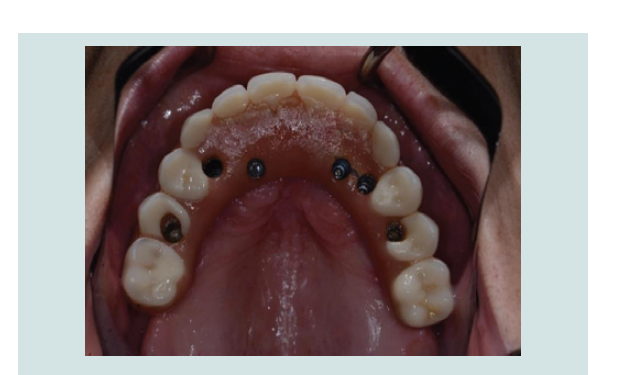
By the end of 2013, both maxillary and mandibular fi nal
restorations (fi xed hybrids) were delivered (Figure 10-13).
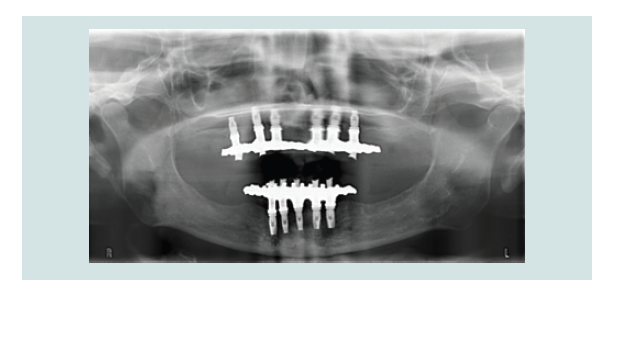
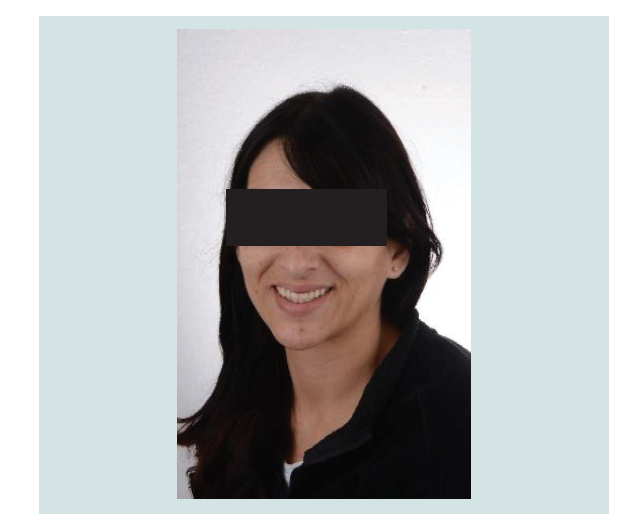
During the following 5 years, the patient came back to the
dental offi ce for maintenance visits every 6 months, where oral
hygiene instructions, education about diabetes mellitus control
with medication (patient HbA1c values were always under 8%) and
motivation to quit/reduce smoking were reinforced (Figure 14-19).
Discussion
According to literature, patients with history of periodontal
disease are more susceptible to periimplantitis [9]. In the systematic review of Ferreira et al. (2018), it was concluded that the history of
periodontitis is associated with the occurrence of periimplantitis.
Similarly, in the meta-analysis of Sgolastra et al. (2015) it was
determined that periodontal disease is a risk factor for implant loss
and periimplantitis, and that it is also related to higher levels of
implant bone loss [10,11].
Smoking tobacco is also associated with teeth loss because it
causes soft tissue infl ammation, decreases salivary fl ow, suppresses
immune response and persuades vasoconstriction, thus facilitating
bacterial growth and deterring regeneration of the periodontium
[12,13]. According to the literature, even the exposure to tobacco
smoke is associated with periodontal disease when compared with
non-exposition to it [14]. Moreover, smoking has an imperative
eff ect in the incidence and development of periodontal disease, since smokers have 80% more risk of periodontal disease than smokers
who quit and nonsmokers. However, smoking cessation has a positive
eff ect in decreasing the risk of periodontal disease (around 14%) and
improves the response to nonsurgical periodontal therapy in the fi rst
year aft er quitting. Likewise, the risk of developing a periodontal
disease in quitters seems to be similar to the one for nonsmokers
[13,15]. In the systematic review of Dreyer et al. (2018), it was
reported that smoking tobacco is also a risk factor for developing
peri-implantitis [9]. However, this habit should not be considered as
an absolute contraindication for implant placement: even if there is a higher risk of failure during the initial healing time aft er surgery,
some authors like Chrcanovic et al. (2015) reported that this depends
on the implant surface’s roughness [16-19]. Th e patient in the current
case report reduced the number of cigarettes smoked per day before
performing the treatment, which could be considered as the fi rst key
factors for the long-term success of it [20] (Figure 14-19).
In the systematic review of Mauri-Obradors et al. (2017), it
was concluded that there is a correlation between diabetes mellitus
and periodontal disease [21]. Th e increase of glucose in the blood
is associated with higher risk of periodontitis due to alterations in
host-immune response against the biofi lm such as the decrease of
neutrophil adherence, chemotaxis and phagocytosis, all facilitating
bacteria to persist in the oral cavity [22]. Similarly, periodontal disease
may cause alterations in the glycemic control (measured using HbA1c)
in diabetic patients as reported in the systematic reviews of Simpson
et al. (2015) and Hasuike et al. (2017), where they found that diabetic
patients with periodontitis who undergo periodontal treatment
improved their glycemic control [23,24]. In the systematic review of
Guobis (2016) it was also stated that diabetes mellitus is an impending
factor for postoperative healing progression aft er implant placement.
As a consequence, this treatment option in diabetic patients should
be only performed in selected cases in which the patient is compliant
in controlling the disease as well as in coming to the dental offi ce
for follow-up appointments [25,26]. According to the literature, the
overall implant failure rate is not higher in diabetic patients when
compared with non-diabetic patients. However, those have a higher
risk of implant failure especially during osseointegration and in the
fi rst year aft er loading [27,28], and they also experience more implant
marginal bone loss in the long term [27]. In the systematic review
of Naujokat et al. (2016) it was concluded that the implant survival
rate aft er 6 years is similar for diabetic and non-diabetic patients.
However, aft er 20 years there is a decrease in the implant survival
rate in diabetic patients well controlled diabetic patients show better
results both in implant survival rate and osseointegration than noncontrolled
ones. Likewise, in the systematic review of Schimmel et al. (2018) it was found that levels of HbA1c greater than 8% are related to less implant survival rate when compared to lower levels [29,30]. Despite all of the above, in the case report of Balshi et al. (2007), it was demonstrated that although implants in diabetic patient have a diff erence in bone remodeling according to RFA and stability measurements, immediate loading protocol is successful and osseointegration survival rate is high [31]. In the systematic review of Naujokat (2016) it was concluded that there is low risk of developing
peri-implantitis in the fi rst years, however peri-implant infl ammation
increases in long-term follow-up in diabetic patients. In the
systematic review of Monje et al. (2017) it was concluded that the risk
is higher in patients with hyperglycemia compared to patient with
normal glucose levels in the blood and that smoking is not needed
to enhance hyperglycemia infl uence in the peri-implantitis [29,32]. Th e current patient’s HbA1c was being well controlled (always under
8%) by medication and this could be considered as the second key
factor for the long-term success of the dental implant in addition to
the patient’s smoking reduction (Figure 14-19).
One of the critical factors to stop the progression of the
periodontal disease is the plaque control performed by the patients.
Th e systematic review of Newton et al. (2015) concluded that the
dentist’s intervention explaining to the patient the severity of the
condition and the benefi ts of changing the oral hygiene care improves
the general oral health [33]. Aft er implant placement, the patient
should be encouraged to improve home oral care and to be present
in the recall visits every 3-6 months for professional oral care and
follow-up evaluation. If this is the case, the long-term prognosis of
the implants will improve [8]. In the study of Costa et al. (2012), it
was concluded that patients without preventive maintenance aft er
implant placement are more prone to peri-implant disease [34]. Th e
current patient was instructed and motivated to start and maintain
good oral homecare and to attend maintenance visits every 6 months,
which could be considered as the last key factor for the long-term
success of the dental implant treatment (Figure 14-19).
Conclusion
• Diabetes mellitus, heavy smoking and poor oral hygiene are
factors that can lead to periodontal and peri-implant diseases, and
consequently to teeth loss and/or implant failure.
• Clinicians should address those factors before considering
implant placement by educating the patient on diabetes mellitus
control, quitting/reducing tobacco and oral hygiene instructions.
• Implant placement with/without immediate loading is a valid
solution for well-controlled diabetic patients in need for fi xed
restorations.
• With proper maintenance, the implants placed on diabetic
patients can have high success rate with minimal bone loss over a
5-year period of time.
References
1. Kinane DF, Stathopoulou PG, Papapanou PN (2017) Periodontal diseases.
Nat Rev Dis Primers 3: 17038.