Journal of Oral Biology
Download PDF
Case Report
Spontaneous Sequestration of Bisphosphonate Related Oro-Antral Fistula - A Case Report
Muchhala S, Rodríguez-Fernández M*, Barsoum A, Patel V, Fernández-Guallart I and Grasso G
Arthur Ashman Department of Periodontology and Implant Dentistry, New York University, New York
*Address for Correspondence: Rodríguez-Fernández M, Department of Periodontology and Implant Dentistry, New York University, Clinic 5W, 345 E 24th St, NY 10010, New York, Tel: +1-347 279 29 58; E-mail: ycy233@nyu.edu
Submission: 05-February-2020;
Accepted: 31-March-2020;
Published: 03-April-2020
Copyright: © 2020 Muchhala S, et al. This is an open access article
distributed under the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited.
Abstract
Complications of bisphosphonate therapy have received increasing
attention in the fi eld of dentistry as these drugs can potentially cause
osteonecrosis of the Maxilla and Mandible (MRONJ). There have been an
increasing number of reports in the literature associating osteonecrosis with
patients taking bisphosphonates prior to oral surgery (12). In rare cases the
necrotic bone segment is entirely separated from the uninvolved bone,
which is known as simultaneous sequestrum. The purpose of this case
report is to present a case of spontaneous separation of necrotic bone in
the maxillary arch without surgical intervention after sinus augmentation
and implant placement, in a patient with a history of treatment with oral
bisphosphonates. These results and those of others suggested that already
osseointegrated dental implants can also cause the osteonecrosis around
the implant after bisphosphonates administration. En block sequestration of
bone with or without implant might be one of the characteristics of implantrelated
MRONJ.
Introduction
Th e United States is undergoing a rapid increase in its older
population due to increased life expectancy and a greater number of
people entering their sixth decade of life [1]. Th is can be attributed
to advances in modern medicine and an increase in knowledge
regarding public health. However, aging predisposes this population
to increased health risks such as cardiovascular disorders, vision
problems, compromised immune systems and osteoporosis.
Osteoporosis is defi ned by the World Health Organization (WHO) as
a bone mineral density that is 2.5 standard deviations below peak bone
mass as measured by Dual Energy X-Ray Absorptiometry (DEXA).
Th is is the most widely used and thoroughly studied bone density
measurement technology today [2]. DEXA is a simple,quick and noninvasive
procedure which uses a very small dose of ionizing radiations
to measure bone loss. Osteoporosis has been treated with various
modalities, which include exercise, increasing protein, calcium, and
vitamin D intake, estrogen therapy, Parathyroid Hormone (PTH)
and antiresorptive medications such as bisphosphonates [3].
Bisphosphonates are being prescribed more oft en for patients
with osteoporosis to prevent bone fracture. According to the national
osteoporosis foundation data released in 2014, 54 million U.S adults
age 50 years and older are aff ected by osteoporosis and low bone mass.
As estimated, 10.2 million adults have osteoporosis and 43.4 million
have osteopenia (low bone density) which is a precursor condition for
osteoporosis [4]. Th e mechanism of action of bisphosphonates involves
complex interactions within the bone. Th is class of medication causes
decreased osteoclastic activity and eventually apoptosis of these cells.
New osteoclasts are not formed, therefore reduced bone resorption
and increased bone density may reduce the risk of fractures in these patients. In addition to osteoporosis, bisphosphonates are indicated
for treatment of metastatic cancer [5], multiple myeloma [6], Paget’s disease [7], or hypercalcemia associated with malignancy [8]. More recently, bisphosphonates have been used to reduce fracture rates in children with Osteogenesis Imperfecta [9].
Although bisphosphonates are benefi cial in many ways, they
pose a risk to patients taking these medications. Complications of
bisphosphonate therapy have received increasing attention in the
fi eld of dentistry as these drugs can potentially cause osteonecrosis
of the maxilla and mandible [10]. Th e term Medication- Related
Osteonecrosis of the Jaw (MRONJ) was given to this condition by
the American Association of Oral Maxillofacial Surgeons [11].
Osteonecrosis of the Jaw is a serious condition that is characterized by
a non-healing and oft en painful exposure of sequestrating bone. Th e
MRONJ lesion is commonly located in areas with dense bone hence
MRONJ is more probable in the mandible than the maxilla (2:1).
Th ere have been an increasing number of reports in the literature
associating osteonecrosis with patients taking bisphosphonates prior
to oral surgery [12].
Depending on the risk and severity of MRONJ, diff erent treatment
modalities are recommended including pain medication, antibiotics,
antibacterial mouth rinses, surgical debridement and resection of the
exposed site [11]. However, in rare cases the necrotic bone segment
is entirely separated from the uninvolved bone, which is known as
simultaneous sequestrum. To the best of authors knowledge few
articles have reported on treatment of simultaneous sequestrum in
the maxilla [13].
Th e purpose of this case report is to present a case of spontaneous
separation of necrotic bone in the maxillary arch without surgical
intervention aft er sinus augmentation and implant placement, in a
patient with a history of treatment with oral bisphosphonates.
Materials and Methods
Th e clinical data in this case report was extracted from the
anonymous Implant Database (ID) from the routine treatment of
patients at the Ashman Department of Periodontology and Implant
Dentistry at the New York University College of Dentistry Kriser Dental Center. Th e offi ce of Quality Assurance at the New York
University College of Dentistry certifi ed the ID. Th is case report is in
compliance with the Health Insurance Portability and Accountability
Act (HIPPA) requirements and approved by the University
Committee on the Activities Involving Human Subjects (UCAIHS).
Case Report
In August 2004, a 50-year-old Asian female patient, with a 10-
year history of taking Ibandronate sodium (Boniva150mg/4weeks
orally), for treatment of osteoporosis, presented to the Ashman
Department of Periodontology and Implant Dentistry of New York
University College of Dentistry. Her chief complaint was replacement
of teeth with fi xed prosthesis on missing maxillary right, fi rst and
second molars and second premolar. Intraoral evaluation showed a
healthy periodontium. Periapical radiographs made using paralleling
cone technique showed adequate restorative space but lack of apicocoronal bone height for implant placement. A cone beam computer
tomography was taken to confi rm the same.
Aft er temporary cessation of the antiresorptive medication
for 3 months before the scheduled surgery, a sinus augmentation
procedure was done via lateral window approach. Th e Schneiderian
membrane was assessed visually and then was elevated without any
perforation noted. Th e initial osteotomy was made considering
optimal angulation and position for the planned fi nal implants, and
the graft material (Geistlich Bioss large particle) was placed in the
contained space. Two parallel wall implants (Osseotite 3i Zimmer)
were placed in the osteotomy in site #2 and #3. Chromic gut (4-0)
sutures (Henry Schein, Melville, N.Y, U.S.A) were used to achieve
tension-free primary closure. Th e patient was put on pre – operative
(2g amoxicillin 1h prior to procedure) and post-operative antibiotics
(500mg amoxicillin/8h/7days). Regular follow-ups showed uneventful
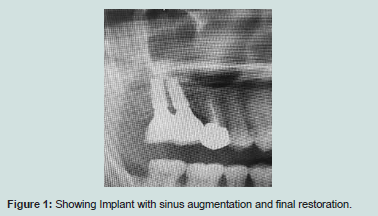
healing. Six months later the fi nal restoration was delivered. Patient
maintained good oral hygiene and regular follow-ups for one year
(Figure 1).
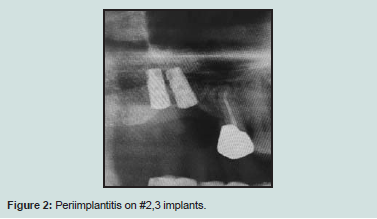
In 2013 the patient presented to the clinic aft er 7 years of missed follow-ups and was diagnosed with peri-implantitis in site #2 (Figure 2). An updated medical history revealed that the patient was now taking Atelvia (Risedronate sodium 35 mg/week orally). Th e fi xed
restoration was removed and the implant in site #2 was explanted due
to peri-implantitis and pain. Th ree years later, in 2016,the implant on
site #3 had to be removed as well due to the same reason (Figure 3).
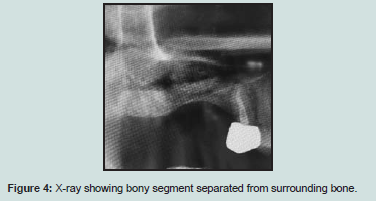
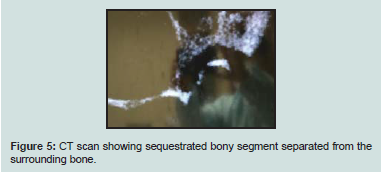
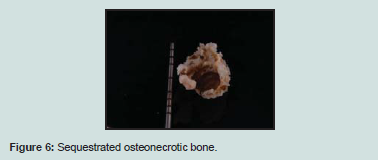
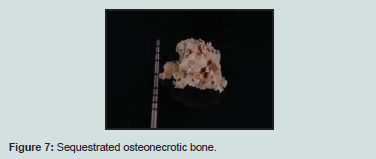
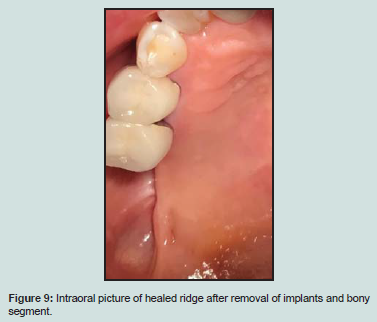
Two months aft er removal of the implant #3, the patient returned with edematous tissue in the maxillary fi rst molar region. Th e tissue was excised, drained and irrigated and patient was put on amoxicillin (500 mg/7 days). Th e same procedure was repeated in the next few visits, but the site did not show improvement. Evidence of bony sequestrum was seen four months aft er the explantation of the implants (Figure 4 and 5). Upon administration of local anesthesia (Lidocaine 1:100,000) the sequestrated bony segment was removed and the patient healed uneventfully (Figure 6-9).
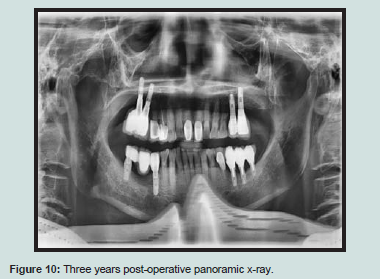
Six months later, two implants 3.3 x 10 mm (EBI, Kyungsan, Republic of Korea) were placed in site #2 and #3. Osseointegration was achieved. 3-year follow-up showed successful results (Figure 10).
Th e patient was put in intervals of 6 months.
Discussion
Bisphosphonates are widely used to treat systemic metabolic
bone diseases. However, their use predisposes a patient to the
potential complication of Medication-Induced Osteonecrosis of the
Jaw (MRONJ). Th is complication must be considered in the various
disciplines in the dental fi eld, including implant dentistry, oral
surgery, periodontics and endodontics.
In MRONJ, alveolar bone becomes exposed for more than 8 weeks
spontaneously, or aft er invasive surgical procedures such as implant
placement, tooth extraction, periodontal surgery or apicoectomy.
Th e osteonecrosis originates in the alveolar bone and extends into the
basal bone. Th e diagnosis is based on clinical fi ndings. However, there
are radiographic, histological, and microbiological fi ndings associated
with MRONJ, which are not pathognomonic for the condition.
Radiographic signs include sclerosis or loss of the lamina dura, and/
or widening of the periodontal ligament space. Microscopically the appearance of necrotic bone with some bacterial colonization has
been noted [9]. Th e 3 most common species associated with secondary
infection in exposed bone due to bisphosphonates are actinomices,
eikenella, and moraxell [12]. Intravenous (IV) bisphosphonates
such as Aredia (pamidronate) or Zometa (zoledronate) cause
osteonecrosis of the jaws from 6 to 16 months post drug treatment
[13]. Reported rates of MRONJ with IV bisphosphonates range
from 0.8% to 12% [14]. In contrast, osteonecrosis caused by oral
bisphosphonates may occur 3 years or more aft er administration due
to their lower absorption rate [15]. Reported rates of spontaneous
MRONJ with oral drugs such as Ibandronate sodium, risedronate
and alendronate were 0.01 to 0.04% and increased to 0.09 to 0.34%
aft er dental extractions [16]. A study which analyzed 119 patients
on IV bisphosphonate therapy in 2005 found that nearly 38% of
bone exposure was associated with extractions and small percentage
(3.4%) was associated with implant placement [13]. On the other
hand, in a study published by Jeff coat in 2006, not a single case of
MRONJ was reported following the placement of 210 implants in
50 patients taking the oral form bisphosphonates [17]. Merck Inc.
has received reports of 170 cases of MRONJ associated with oral alendronate therapy out of approximately 20 million patient-years,
or 0.7 reports of MRONJ per 100,000 patient-years of exposure. With
oral risedronate, 1 to 1.2 cases per 10,000 patient-years were reported
by Procter & Gamble. Current American Association of Oral and
Maxillofacial Surgeons guidelines recommend a drug holiday from
3 to 6 months before dental implant placement in patients with a
history of oral bisphosphonate used for greater than 3 years.
It is estimated that 75% of MRONJ is caused by uncontrolled
dental infl ammatory disease and dental trauma. Th erefore, avoiding
invasive dental surgery is highly recommended aft er drug therapy has
been initiated. Th e absorption of oral bisphosphonates is much slower
than the IV form, so the risk of MRONJ usually does not manifest
itself until aft er 3 years of continuous administration [15]. Dental
treatment, including implants is not contraindicated within this 3
year window [18]. However, physicians may not be inclined to take
patients off of bisphosphonate therapy due to increased morbidity and
mortality rates associated with osteoporotic fractures [19,20]. Patients
who cannot alter their drug regimen and are in need of emergency
care should be treated with informed consent which describes the
potential to develop osteonecrosis of the jaws. Marx has advocated
a method of assessing risk for patients using oral bisphosphonates
[9]. He recommends that the patient receive a blood test for serum
CTX (C-telopeptides of type I collagen) which is a bone turnover
marker. Th is test can identify changes in bone remodeling/renewal
within 2 days to 2 weeks of onset of drug use. Th is test measures the
relative rate of bone renewal and bone resorption. Values greater than
150 mg/ml correlate to low risk for developing osteonecrosis. Values
between 100 and 150 mg/ml correlate to a moderate risk, while values
below 100 mg/ml identify high risk patients. However, the accuracy
of this test has been questioned and there have been no long-term
studies to measure its validity, specifi city and accuracy.
Treatment should be rendered in cases where bone has been
exposed for more than 8 weeks. Management of the patient depends
on the clinical severity of the exposed bone and presentation of
local/systemic infection. Intravenous bisphosphonate-induced
osteonecrosis usually presents as more clinically extensive and
less responsive to treatment than oral bisphosphonate-induced
osteonecrosis [13]. Th e following four categories of treatment are
proposed by the American Association of Oral Maxillofacial Surgery
Position Paper on treatment of MRONJ. Th e preliminary one
includes patients at risk of developing MRONJ due to the fact that
they have been treated with oral or intravenous bisphosphonates,
and only requires prevention such as avoidance of traumatic surgery.
Th e fi rst true category (stage 1), when asymptomatic necrotic bone
is exposed around implants, suggests a treatment of daily rinse
with 0.12% chlorohexidine. Th e second category (stage 2) is seen
in patients with exposed bone associated with infection and pain.
In this case, antibiotics should be considered in addition to daily
rinses with 0.12% chlorohexidine and proper analgesics. Th e primary
antibiotic that is suggested is penicillin (Pen VK 500mg) prescribed
four times daily due to its signifi cant eff ect on the three main species
of bacteria present secondary to osteonecrosis. Other antibiotics
include levofl oxacin (Levaquin 500mg once daily) or azithromycin
(Zythromax250 mg once daily). Antibiotic regimens are given for 14
days. In cases of refractory pain, Flagyl (Metronidazole500 mg) can be prescribed three times a day. Incision and drainage of the area should
be completed when fl uctuant swelling is present. Th e third category
of patients (stage 3) presents with additional clinical signs such as
mobility of the exposed bone, extra-oral fi stula, pathologic fracture or
osteolysis extending to the inferior border, and its treatment includes
surgical debridement and resection for longer term palliation of
infection and pain aft er drug therapy (antibiotic and painkillers, as
well as antibacterial mouth rinse) has been initiated [16].
Good communication with health professionals is essential on
deciding the most appropriate timing of dental treatment. If possible,
IV bisphosphonate therapy should be withheld for roughly 2-3
months while attending to the patient’s dental needs. For patients not
requiring invasive dental therapy, IV bisphosphonate therapy does
not need to be delayed. If a patient is currently on bisphosphonate
therapy, the aim of dental treatment is to maintain optimal oral health
and to avoid invasive dental procedures. For example, a tooth that is
deemed unrestorable due to caries should have endodontic therapy
completed and the crown amputated as opposed to it being extracted.
If a tooth must be extracted, penicillin (Pen VK 500 mg prescribed
four times daily) or azithromycin (Zythromax 250 mg once daily)
should be prescribed for 7 days. Periodontal disease should be treated
non-surgically with supragingival scaling and irrigation with 0.12%
chlorohexidine rinse [18].
Several factors could have played a role in the development of
MRONJ in our patient. Although Bisphosphonates tend to accumulate
in sites of active bone remodeling like the jaws, the surgical trauma to
the alveolar bone during implant surgery could have further stimulated
the postoperative accumulation of the drug in the implanted site.
However, our patient had stopped oral bisphosphonate therapy
for 3 months prior to sinus graft ing procedure and dental implants
placement and still developed MRONJ aft er 7 years. Th e terminal
(slowest) elimination half-life was estimated to be about 10 years,
consistent with the overall estimated half-life of skeletal turnover.
Th is could be another reason for MRONJ development in our patient.
MRONJ is more oft en localized in the mandible than in the maxilla
(2:1 ratio). A compromised blood supply to the maxilla and mandible,
along with altered bone remodeling aft er exposure to long-term
Bisphosphonate therapy, has been proposed as the theory behind the
pathogenesis of osteonecrosis [21,22]. In the present case, the fact that
the episode occurred in the maxilla could be related to the avascular
nature of the sinus cavity, specially aft er being graft ed with xenograft .
In this case, the exposed bone could have been classifi ed as a stage 3
due to its mobility, and was treated with removal and debridement of
the area, antibiotics, painkillers and mouthwash. Aft er its complete
healing and monitoring for 6 more months, the area was considered
suitable for a new minimally invasive implant treatment.
Conclusion
Few reports describe side eff ects of bisphosphonate usage,
particularly such as MRONJ in the maxilla. Th is case addresses
this lack. Presentation of MRONJ is currently more commonly
seen in patients taking the intravenous forms of the drug; however,
prescriptions for oral bisphosphonates continue to rise, and there
is fear that the long-term cumulative eff ects of these drugs may see
MRONJ occurring in patients at a rate equal to that seen in patients undertaking intravenous therapy. Good communication with health
professionals is essential on deciding the most appropriate timing of
dental treatment. Many of the precautions taken in order to reduce
the risk of MRONJ with IV bisphosphonate therapy should also be
followed in patients taking oral bisphosphonates. In conclusion, these
results and those of others suggested that already osseointegrated
dental implants can also cause the osteonecrosis around the implant
aft er bisphosphonates administration. En block sequestration of
bone with or without implant might be one of the characteristics of
implant-related MRONJ.