Journal of Ocular Biology
Download PDF
Case Report
*Address for Correspondence: We Fong Siah, MB BCh BAO, BA, MRCOphth, MRCPI, Department of Ophthalmology, Mater Misericordiae University Hospital, Dublin 7, Ireland, E-mail: wefong_siah@yahoo.com
Citation: Siah WF, Logan P. Retinal Artery Occlusion after Embolization of Intracranial Tumor. J Ocular Biol. 2013;1(2): 2.
Copyright © 2013 Siah WF, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Ocular Biology | ISSN: 2334-2838 | Volume: 1, Issue: 2
Submission: 18 September 2013 | Accepted: 18 October 2013 | Published: 23 October 2013
Reviewed & Approved by: Dr. Bjørn Nicolaissen, Department of Ophthalmology, University of Oslo, Norway
Embolization plays an important role as an adjunct to the surgical management of tumors. The use of liquid embolic agents, embolic microparticles or coils to devascularize the tumor bed facilitates safer surgical resection of the tumor itself [1]. However, this procedure carries the risk of neurological deficit, visual loss and severe disability. Branch retinal artery occlusion [2] and cilioretinal artery occlusion [3] have been reported following embolization of intracranial meningioma. Here, we report two cases of iatrogenic retinal artery occlusions occurring after embolization of intracranial tumor feeder arteries with occlusive agents. Retinal artery occlusion is an ocular emergency that is associated with profound morbidity.
Retinal Artery Occlusion after Embolization of Intracranial Tumor
We Fong Siah1* and Patricia Logan1,2
- 1Department of Ophthalmology, Mater Misericordiae University Hospital, Dublin 7, Ireland
- 2Department of Ophthalmology, Beaumont Hospital, Dublin 9, Ireland
*Address for Correspondence: We Fong Siah, MB BCh BAO, BA, MRCOphth, MRCPI, Department of Ophthalmology, Mater Misericordiae University Hospital, Dublin 7, Ireland, E-mail: wefong_siah@yahoo.com
Citation: Siah WF, Logan P. Retinal Artery Occlusion after Embolization of Intracranial Tumor. J Ocular Biol. 2013;1(2): 2.
Copyright © 2013 Siah WF, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Ocular Biology | ISSN: 2334-2838 | Volume: 1, Issue: 2
Submission: 18 September 2013 | Accepted: 18 October 2013 | Published: 23 October 2013
Reviewed & Approved by: Dr. Bjørn Nicolaissen, Department of Ophthalmology, University of Oslo, Norway
Embolization plays an important role as an adjunct to the surgical management of tumors. The use of liquid embolic agents, embolic microparticles or coils to devascularize the tumor bed facilitates safer surgical resection of the tumor itself [1]. However, this procedure carries the risk of neurological deficit, visual loss and severe disability. Branch retinal artery occlusion [2] and cilioretinal artery occlusion [3] have been reported following embolization of intracranial meningioma. Here, we report two cases of iatrogenic retinal artery occlusions occurring after embolization of intracranial tumor feeder arteries with occlusive agents. Retinal artery occlusion is an ocular emergency that is associated with profound morbidity.
Case 1
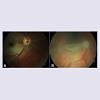
A 23 year old gentleman who has an extensive right temporal lobe haemangiopericytoma involving the skull bone had selective catheterization and embolization of the tumor feeder artery with a liquid embolic agent (Onyx®) to reduce blood flow in the tumor bed prior to an elective surgical debulking procedure. He experienced transient visual obscurations immediately after the procedure and was arranged to be seen by an ophthalmologist at the Eye Clinic. The Snellen visual acuity of each eye was 20/20. While in the waiting room, he developed a sudden deterioration of vision to hand movements only in his right eye. There was a dense relative afferent pupillary defect and a diagnosis of a central retinal artery occlusion (CRAO) was made. This completely resolved after 15 minutes with complete restoration of his vision. Unfortunately, a second episode of CRAO occurred 15 minutes later and his right vision deteriorated to no perception of light. Immediate interventions such as ocular massage, anterior chamber paracentesis, topical beta-blocker and intravenous acetazolamide to improve retinal artery circulation failed to reverse the CRAO. An emergency cerebral angiogram was performed. Although the right ophthalmic artery was patent, his vision remained unchanged. Hence, only a very small dose of intra-arterial fibrinolysis with 10 mg of alteplase (recombinant tissue plasminogen activator) was administered into the right ophthalmic artery. His right vision improved to hand movement the following day. As visualized in Figure 1A, embolic particles are observed in retinal arteries on ophthalmoscopy.Case 2
A 61 year old lady underwent embolization of her right spenoidal wing meningioma with a gelatin microsphere agent (Embospheres). Selective catheterization with 100-300 μm of embospheres prediluted with contrast was used and good angiographic occlusion of the tumor was achieved. The patient experienced loss of vision in her right eye 30 minutes post-embolization. Her vision was no perception of light and an afferent pupillary defect was evident. She was seen by an ophthalmologist within 3 hours of onset and a diagnosis of a retinal artery occlusion was made. She received immediate ocular massage, anterior chamber paracentesis, topical beta-blocker and intravenous acetazolamide. Ophthalmoscopy showed a pale optic disc, ischemic whitening of the retina at the cilioretinal artery distribution, cherry red spot and extensive cattle-tracking of retinal arterioles (Figure 1B). These findings were consistent with a combined CRAO and cilioretinal artery occlusion.Both of our patients had immediate conventional treatment (ocular massage, topical beta-blocker, anterior chamber paracentesis and intravenous acetazolamide) of CRAO following the onset of the event. Our patient in case 1 also underwent intra-arterial fibrinolysis in the attempt to recanalize the retinal artery but failed. The dose of alteplase that was given was very small taking to pre-empt the risk of a hemorrhage with a therapeutic dose. Furthermore, the embolic particles visualized on ophthalmoscopy were suggestive of Onyx® and alteplase was likely to have no benefit. Schumacher et al. demonstrated similar outcomes between conservative management versus local intra-arterial fibrinolysis in acute CRAO independent of tumor embolization [4].
The blood supply of meningiomas usually arises from branches of the external carotid artery, except in cases of anterior and middle cranial base tumors where they are commonly supplied from branches of the internal carotid artery, such as the ophthalmic artery. In a retrospective analysis of 167 cranial base meningiomas that were embolized with polyviny acetyl foam, Rosen et al. found a 1.8% risk of retinal artery occlusion despite supraselective angiography [5]. Two patients had loss of vision and 1 patient was left with a small visual field deficit. In their study, it was interesting that none of the patients who had embolization via the ophthalmic artery develop any ocular complication whilst the 2 patients who developed monocular blindness had embolization via a non-ophthalmic artery route. In these 2 cases, there was no incident uncontrolled embolization particle release or reflux. Rosen and colleagues felt that this devastating complication may not have been averted with any other strategy as the complication was independent of tumor location or vessel embolized.
It is crucial that awareness of such a serious complication be raised among neurosurgeons, intervention neuroradiologist and ophthalmologist. Firstly, the indication for embolization for an intracranial tumor has to be justified. Secondly, the presence of expertise such as intervention neuroradiologist is of paramount importance as good understanding of the vascular anastomosis is required to avoid inadvertent embolization of naïve vessels. Finally, easy access to an ophthalmologist for prompt diagnosis and initiation of treatment is of great value to increase retinal survival time following a CRAO.
The appropriate management of CRAO following embolization is not well explored and this ocular emergency carries devastating implications for the patient. With the increasing use of embolization in the management of intracranial tumors, the authors expect to see a rise in the incidence of this complication. We feel that all patients who are undergoing embolization of intracranial tumors should be informed of the risk of visual loss as this has long term consequences and impact on the quality of life.
References
- Lazzaro MA, Badruddin A, Zaidat OO, Darkhabani Z, Pandya DJ, et al. (2011) Endovascular embolization of head and neck tumors. Front Neurol 2: 64.
- Turner T, Trobe JD, Deveikis JP (2002) Sequential branch retinal artery occlusions following embolization of an intracranial meningioma. Arch Ophthalmol 120: 857-860.
- Kunikata H, Tamai M (2006) Cilioretinal artery occlusions following embolization of an artery to an intracranial meningioma. Graefes Arch Clin Exp Ophthalmol 244: 401-403.
- Schumacher M, Schmidt D, Jurklies B, Gall C, Wanke I, et al. (2010) Central retinal artery occlusion: local intra-arterial fibrinolysis versus conservative treatment, a multicenter randomized trial. Ophthalmology 117: 1367-1375.
- Rosen CL, Ammerman JM, Sekhar LN, Bank WO (2002) Outcome analysis of preoperative embolization in cranial base surgery. Acta Neurochir (Wien) 144: 1157-1164.