Journal of Ocular Biology
Download PDF
Research Article
*Address for Correspondence: Miguel Pedroza-Seres MD, PhD, Instituto de Oftalmologia ”Conde de Valenciana”, Chimalpopoca 14, 06800, Mexico City, Mexico, E-mail: mpedrozaseres@gmail.com
Citation: Pedroza-Seres M, Serna-Ojeda JC, Dalli-Palomera R. Pulsed Intravenous Cyclophosphamide for Severe Ocular Inflammatory Disease: An International Experience. J Ocular Biol. 2015;3(1): 3.
Copyright © 2015 Pedroza-Seres M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Ocular Biology | ISSN: 2334-2838 | Volume: 3, Issue: 1
Submission: 11 February 2015 | Accepted: 07 MArch 2015 | Published: 11 March 2015
Reviewed & Approved by: Dr. Yi Wei, Assistant Professor, Department of Ophthalmology, Ichan School of Medicine at Mount Sinai, USA
All the patients were previously treated with oral corticosteroids. The median number of pulses of cyclophosphamide was 3 (range 1 to 12 pulses). Eighteen patients (85.7%) attained clinical improvement, and thirteen (61.9%) achieved remission of the inflammatory process. Twenty patients (95.2%) achieved reduction in the corticosteroid dose after the treatment with cyclophosphamide, with 10 patients (47.6%) achieving a complete elimination of the prednisone. Fourteen patients (66.6%) gained two or more lines of vision, with a median final best-corrected visual acuity of 20/40 (range 20/20 – hand motion) in the affected eyes. Some patients required also other types of immunosuppressive therapy as follows: Methotrexate in 14 patients (66.6%), azathioprine in 5 (23.8%), mycophenolate mofetil in 1 (4.7%) and oral cyclophosphamide in 1 (4.7%).
Pulsed Intravenous Cyclophosphamide for Severe Ocular Inflammatory Disease: An International Experience
Miguel Pedroza-Seres1,2*, Juan Carlos Serna-Ojeda1 and Roberto Dalli-Palomera2
- 1Department of Uveitis and Ocular Immunology, Instituto de Oftalmologia “Conde de Valenciana”, Mexico City, Mexico
- 2Department of Uveitis and Ocular Immunology, Clinica de Retina, Guadalajara, Jal, Mexico
*Address for Correspondence: Miguel Pedroza-Seres MD, PhD, Instituto de Oftalmologia ”Conde de Valenciana”, Chimalpopoca 14, 06800, Mexico City, Mexico, E-mail: mpedrozaseres@gmail.com
Citation: Pedroza-Seres M, Serna-Ojeda JC, Dalli-Palomera R. Pulsed Intravenous Cyclophosphamide for Severe Ocular Inflammatory Disease: An International Experience. J Ocular Biol. 2015;3(1): 3.
Copyright © 2015 Pedroza-Seres M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Ocular Biology | ISSN: 2334-2838 | Volume: 3, Issue: 1
Submission: 11 February 2015 | Accepted: 07 MArch 2015 | Published: 11 March 2015
Reviewed & Approved by: Dr. Yi Wei, Assistant Professor, Department of Ophthalmology, Ichan School of Medicine at Mount Sinai, USA
Abstract
Study background: The purpose of this study is to assess the clinical response of intravenous pulses of cyclophosphamide for severe ocular inflammation.Methods: This is an observational and retrospective clinical study, with inclusion of all the patients with severe ocular inflammatory diseases treated with pulsed intravenous cyclophosphamide. The data obtained from the medical records included general information, initial and final best-corrected visual acuity, complications, previous therapy and time of follow-up. We assessed inflammation according to the ocular manifestation for outcome analysis. Clinical improvement and the corticosteroid-sparing effect were evaluated.
Results: Twenty-one patients were included (32 eyes) with a median age of 57 years. The most common ocular diagnosis was necrotizing scleritis. The median number of pulses of cyclophosphamide was 3 (range 1 to 12 pulses). Eighteen patients (85.7%) attained clinical improvement, and twenty patients (95.2%) achieved reduction in the corticosteroid dose after the treatment with cyclophosphamide. Fourteen patients (66.6%) gained two or more lines of vision, with a median final best-corrected visual acuity of 20/40. Six patients (28.5%) presented adverse effects attributed to the cyclophosphamide. The median time of follow-up was 8 months (range 3 – 19 months).
Conclusion: The use of intravenous pulses of cyclophosphamide in ocular inflammatory disease could be used with good results including clinical and visual improvement, and with a high rate in reduction in the corticosteroid dose.
Introduction
Severe ocular inflammatory disease may lead to blindness, thus the rapid control of inflammation is mandatory and requires the use of effective anti-inflammatory drugs. Cyclophosphamide, an alkylating agent that inhibits mitosis of lymphocytes, has been proven effective for the treatment of ocular manifestations of systemic autoimmune diseases such as granulomatosis with polyangiitis (Wegener’s) and rheumatoid vasculitis [1,2]. Cyclophosphamide has also been effective in other ocular inflammatory conditions including idiopathic scleritis, Mooren’s ulcer and Vogt- Koyanagi-Harada Syndrome [3].In this study, we assessed the clinical response of intravenous pulses of cyclophosphamide for severe ocular inflammatory disease. Cyclophosphamide was selected as the first line of treatment because the degree of inflammation could cause potential blindness or because it was the first line of therapy in systemic associated diseases like granulomatosis with polyangiitis.
Methods
This is an observational and retrospective clinical study, with inclusion of all the patients with severe and refractory ocular inflammatory diseases treated from June 2012 to December 2013 with pulsed intravenous cyclophosphamide in two academic centers from Mexico. All study participants had a complete ophthalmologic exam, a baseline complete hemogram including differential and platelet values, liver and renal function tests and urinalysis. Laboratory exams to exclude infectious etiologies were also performed, including a tuberculosis skin test, venereal disease research laboratory and a fluorescent treponemal antibody absorption test, among others if the suspicion of another specific entity was high. The patients received previous therapy with oral prednisone at a dose of 1mg/Kg/day, and in some cases with other immunosuppressive drugs. Intravenous pulses of cyclophosphamide (10-15 mg/kg) were administered over a 1-hour period, and these infusions were repeated every four weeks until a complete absence of active inflammation (absence of inflammatory cells in anterior chamber or vitreous, improvement of visual acuity, absence of redness of scleral inflammation or absence of inflammation in conjunctiva in patients with ocular pemphigoid) was observed.The data obtained from the medical records included age at time of consultation, gender, ocular diagnosis, underlying disease, initial and final best-corrected visual acuity, complications, previous therapy and time of follow-up.
We assessed inflammation according to the ocular manifestation for outcome analysis and all the patients were graded from 0 (no inflammation) to 4 (severe inflammation). Scleritis was graded according to inflammation of the sclera and dilation of the deep episcleral vessels with or without uveal show [4]. For uveitis, the degree of anterior and posterior cells was considered [5]. The ocular mucous membranous pemphigoid was assessed by conjunctival inflammation and for the patients with vasculitis, the evaluation was performed clinically and with fluorescein angiography.
Clinical improvement in patients with scleritis was defined as a decrease in their inflammation from 3+ or 4+ to 0+ or 0.5+ based on the clinical criteria defined by Sen [4]. Clinical improvement in patients with uveitis was defined as a two-level decrease in inflammation, and visual improvement as an increase in two lines of vision after treatment, based on the parameters defined by the SUN Working Group [5]. The corticosteroid-sparing effect was evaluated as a final prednisone dose of 10 mg/day or less. Using descriptive statistics, categorical variables were evaluated using percentages and numerical variables were assessed using measures of central tendency for non-parametric distribution.
The data acquisition, study design and methodology were carried out with the approval of the Ethics Committee and Research Board of our institution. The study was in adherence to the tenets of the Declaration of Helsinki. Approved informed consent was obtained from all patients undergoing immunosuppressive therapy.
Results
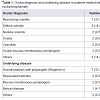
A total of 21 patients were included, with bilateral disease in eleven of them (32 eyes). Thirteen patients were female (61.9%) and eight were male (38.1%), with a median age in the population of 57 years (range 17 to 85 years). The most common ocular diagnosis was necrotizing scleritis. Fourteen patients (66.6%) had an underlying systemic disease, being the most common granulomatosis with polyangiitis (Wegener’s). The ocular diagnosis and underlying disease of the patients are shown in Table 1.All the patients were previously treated with oral corticosteroids. The median number of pulses of cyclophosphamide was 3 (range 1 to 12 pulses). Eighteen patients (85.7%) attained clinical improvement, and thirteen (61.9%) achieved remission of the inflammatory process. Twenty patients (95.2%) achieved reduction in the corticosteroid dose after the treatment with cyclophosphamide, with 10 patients (47.6%) achieving a complete elimination of the prednisone. Fourteen patients (66.6%) gained two or more lines of vision, with a median final best-corrected visual acuity of 20/40 (range 20/20 – hand motion) in the affected eyes. Some patients required also other types of immunosuppressive therapy as follows: Methotrexate in 14 patients (66.6%), azathioprine in 5 (23.8%), mycophenolate mofetil in 1 (4.7%) and oral cyclophosphamide in 1 (4.7%).
Six patients (28.5%) presented adverse effects attributed to the cyclophosphamide, including 3 patients (14.2%) with low leucocyte count and anemia, 1 (4.7%) with blood in urine, 1 (4.7%) with an opportunistic infection and 1 (4.7%) with gastrointestinal upset. The median time of follow-up was 8 months (range 3 – 19 months).
Discussion and Conclusions
In this study we exclusively present the results of a group of patients with severe and in some cases recalcitrant inflammatory ocular disease treated with pulsed intravenous cyclophosphamide.Although the intravenous administration provides some advantages over oral administration of cyclophosphamide including potential lower risks of side effects, the available information suggest that oral administration may be more effective, so both regimens have been studied for ocular inflammatory disease [3,6]. However, in the country of the setting of this study, there is only access to intravenous cyclophosphamide.The most common ocular manifestation in our study was scleritis in different presentations (57% for the 3 groups combined), with Granulomatosis with polyangiitis as the most common underlying disease like in another study that evaluated a pulsed intravenous cyclophosphamide and methylprednisolone protocol [7].
All our patients received previous treatment with corticosteroids. The achievement of remission in our study was slightly lower than the reported from another group, 61.9% and 84.4% respectively, but the reduction in the corticosteroid dose was higher in our patients, 95.2% and 89.7% respectively [8]. Also, the percentage of patients gaining two or more Snellen lines was higher than the one reported in another study of pulsed intravenous cyclophosphamide, 66.6% and 21% respectively.
Finally, less than a third of patients presented adverse effects related to cyclophosphamide, which is consistent with the discontinuation rate of the medication for side effects in a large cohort of patients with ocular inflammatory disease treated with oral or intravenous cyclophosphamide [3].
We can conclude that the use of intravenous pulses of cyclophosphamide in ocular inflammatory disease could be used with other drugs like steroids or immunosuppressive therapy with good results including clinical and visual improvement, and with a high rate in reduction in the corticosteroid dose.
References
- Koldingsnes W, Gran JT, Omdal R, Husby G (1998) Wegener's granulomatosis: long-term follow-up of patients treated with pulse cyclophosphamide. Br J Rheumatol 37: 659-664.
- Scott DG, Bacon PA (1984) Intravenous cyclophosphamide plus methylprednisolone in treatment of systemic rheumatoid vasculitis. Am J Med 76: 377-384.
- Pujari SS, Kempen JH, Newcomb CW, Gangaputra S, Daniel E, et al. (2010) Cyclophosphamide for ocular inflammatory diseases. Ophthalmology 117: 356-365.
- Sen HN, Sangave AA, Goldstein DA, Suhler EB, Cunningham D, et al. (2011) A standardized grading system for scleritis. Ophthalmology 118: 768-771.
- Jabs DA, Nussenblatt RB, Rosenbaum JT (2005) Standardization of uveitisnomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol 140: 509-516.
- Durrani K, Papaliodis GN, Foster CS (2004) Pulse IV cyclophosphamide in ocular inflammatory disease: efficacy and short-term safety. Ophthalmology 111: 960-965.
- Khan IJ, Barry RJ, Amissah-Arthur KN, Carruthers D, Elamanchi SR, et al. (2013) Ten-year experience of pulsed intravenous cyclophosphamide and methylprednisolone protocol (PICM protocol) in severe ocular inflammatory disease. Br J Ophthalmol 97: 1118-1122.
- Suelves AM, Arcinue CA, González-Martín JM, Kruh JN, Foster CS (2013) Analysis of a novel protocol of pulsed intravenous cyclophosphamide for recalcitrant or severe ocular inflammatory disease. Ophthalmology 120: 1201-1209.