Journal of Orthopedics & Rheumatology
Download PDF
Research Article
Pseudotumor Treated with Two-Stage Revision Due to Aggressive Osteolysis and Soft-Tissue Mass Following Metal on Metal Total Hip Arthroplasty
Yakkanti RR*, Nguyen D and Pretell-Mazzini J
Department of Orthopaedic Surgery, University of Miami, USA
*Address for Correspondence: Yakkanti RR, Department of Orthopaedic Surgery, University of Miami, Miller School of Medicine, 1611 NW 12th Ave #303, Miami, FL 33136, USA, Tel:
502-689-3127; E-mail: ramakanth.yakkanti@jhsmiami.org
Submission: 11 September 2020;
Accepted: 02 November 2020;
Published: 16 November 2020
Copyright: © 2020 Yakkanti RR, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Introduction: This is a unique case of the largest reported pseudotumor in literature, treated with a custom acetabular component in conjunction with a total femur replacement.
Case: Patient is a 71-year-old male, with a large pseudotumor secondary to Metal on Metal total hip arthroplasty, who had chronic pain for 8 years prior to presentation. Imaging revealed extensive soft tissue mass and osteolysis. Patient underwent two-stage surgery, with 1st stage involving surgical debridement of pseudotumor and fixation of custom triflange acetabular component, 2nd stage involved a total
femur replacement.
Conclusion: This case demonstrates the evaluation and management of a large pseudotumor. A two-stage revision in complex pseudotumor cases, with complete revision of the implants and excision of the pseudotumor, to achieve clinical improvement and decrease complications is a viable option.
Keywords
Pseudotumor; Total hip arthroplasty (THA); Metal on metal (MoM); Revision surgery; Mega prosthesis; custom implants
Introduction
There are multiple bearing surfaces available for Total Hip
Arthroplasty (THA), with Metal On Metal (MoM) implants being
a common choice [1]. MoM implants were developed for better
volumetric wear propertiesand improved stability [2]. However,
MoM implants have high rates of metallosis and pseudotumor
formation,1–39%of cases [1,2].
Pseudotumors are defined as non-neoplastic, non-infectious
cystic or solid mass forming lesions1. In many cases they develop due
to biological reactions similar to hypersensitivity type 4 reactions to
metal ions, released from abrasive wear of the prosthesis, leading to
osteolysis and soft-tissue damage [3]. Clinical presentation may vary
from absence of symptoms to pain associated with rashes, instability,
nerve palsy and prosthetic loosening with osteolysis [4].
Classification systems for stratification, diagnosis and management
pathways for implant failure and soft tissue complications due to
pseudotumors have been described in literature; however, no current
evidence-based surgical management guideline exists [5,6].
We describe a patient with a failed MoMTHA due to a large
fibroblastic pseudotumor causing osteolysis of the left hemipelvis
and femur. To our knowledge, this is the first case report in which a
custom tripflange acetabular implant in conjunction with total femur
mega prosthesis was used during a two-stage revision for treatment
of a pseudotumor.
The patient was informed that data concerning the case would be
submitted for publication, and he consented.
Case Report
A 71-year-old male with BMI of 27.7 and history of a left
MoMTHA in 1999 presented to our institution with 8 years of
chronic, progressive left groinand thigh pain which was worse
with weight-bearing and at night. He had complete loss of hip
and knee range of motion and required a walker for ambulation.
Surgical history includes left acetabular liner and femoral head
exchange, without relief of symptoms, 3 years prior to presentation.
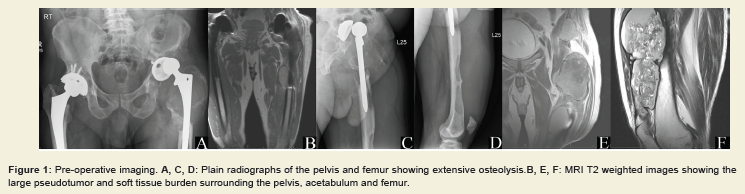
Radiographs showed extensive osteolysis surrounding the acetabular
implant with posterolateral subluxation of the femoral head, as well
as severe osteolysis involving the femoral shaft with multiple large lytic lesionsextending to the distal femur (Figure 1A-D). The MRI
demonstrated a heterogeneous mass with layering of contents, a
low signal intensity mass invasion into the ilium, large soft tissue
mass on the anterior aspect of the thigh with cortical erosion and
breakthrough into several points along the anterior cortex of the distal
femur (Figure 1B,C,F). Laboratory results including CBC, BMP, ESR,
CRP, Serum chromium and cobalt levels were within normal limits.
The osteolytic nature of the soft tissue mass prompted biopsy, which
ruled out neoplastic or infectious process.
Figure 1: Pre-operative imaging. A, C, D: Plain radiographs of the pelvis and femur showing extensive osteolysis.B, E, F: MRI T2 weighted images showing the
large pseudotumor and soft tissue burden surrounding the pelvis, acetabulum and femur.
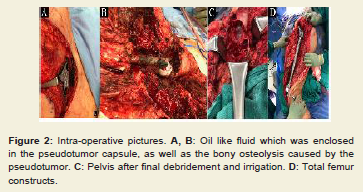
Figure 2: Intra-operative pictures. A, B: Oil like fluid which was enclosed
in the pseudotumor capsule, as well as the bony osteolysis caused by the
pseudotumor. C: Pelvis after final debridement and irrigation. D: Total femur
constructs.
Due to the complexity of the necessary reconstruction the
surgery was staged. First stage involved complete debridement of
the pseudotumor surrounding the left hip, pelvis and proximal thigh
using a Kocher-Langenbeck approach with proximal extension
to iliac crest, and distal extension to lateral approach to femur.
Dissection of the fascia lata revealed a viscous, black, oil-like fluid
(Figure 2A), contained in the pseudotumor capsule. Large portions
of the hip abductors and quadriceps muscles were non-viable due to
metallosis. There was a “pseudo-membrane” covering the proximal
thigh, with severe osteolysis of the proximal femur, acetabulum and
iliac bone (Figure 2B). The pseudo-membrane was debrided, and the
operative field was copiously irrigated (Figure 2C). Reconstruction of
the acetabulum with a custom patient-matched triflange acetabular
component was performed. (Zimmer/Biomet; Warsaw, IN.)
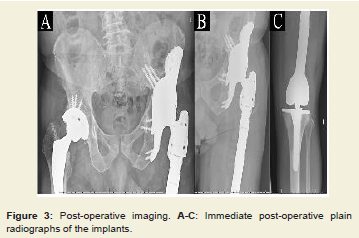
Three days later the second stage involving, resection of the distal
two thirds of the femur due to severe bone loss, and subsequent
reconstruction with a total femoral replacement(Zimmer/Biomet;
Warsaw, IN) using a constrained liner in the hip and a standard
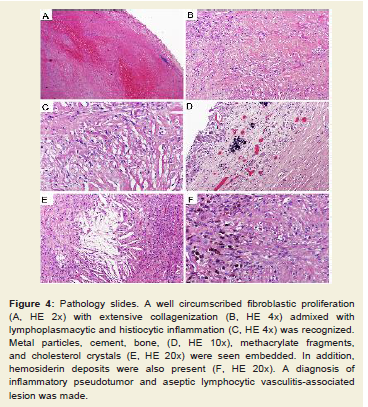
rotating-hinge for the knee, was performed (Figure 2D and 3A-C). Final pathology was compatible with a septic lymphocytic vasculitisassociated
lesion (ALVAL)and inflammatory pseudotumor (Figure 4).
Post-operatively, the patient was allowed full weight bearing with a hip abduction brace that was discontinued at 6 weeks. At his recent follow up (14 months post-op) the patient had a Harris hip score of
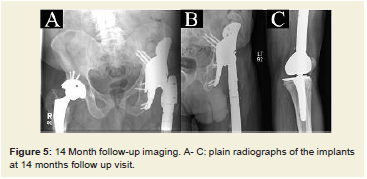
82, which is compatible with a successful outcome. There was no radiographic evidence of osteolysis or component loosening (Figure 5A-C). Blood chromium and cobalt ions were within normal limits.
Discussion
Pseudotumors are mass forming lesions occasionally associated
with MoM THA, and are described as non-infectious, non-neoplastic
soft-tissue proliferations, they can display variable morphology,
including solid, cystic or mixed lesions. These lesions are due to
immune mediate reactions that trigger a cytokine cascade similar
to type-4 hypersensitivity reactions to metal ions more accurately
described as ALVALs.2Local toxicity of the metal ions causes
subsequent osteolysis and soft-tissue cell and fiber damage increasing
the inflammatory stimuli.Schmalzried and Callaghan reported that
these aggressive inflammatory stimuli could lead to lysis occurring at
any point along the space of the hip joint [7].
In patients with pseudotumors, clinical symptoms do not
necessarily correlate with the size of a pseudotumor found on MRI
or ultrasound imaging [7-9]. Elevated serum cobalt might have an
association with tumor size, but not necessarily to symptoms, as 57-
78 % of pseudotumor cases are asymptomatic [1,2,5].
Pseudotumors with Cobalt (Co) and Chromium (Cr) levels
of >7 ppbare concerning and >20μg/L, with or without symptoms,
receive serious consideration for revision arthroplasty [2,3]. Metal (chromium and cobalt) ions and particles released from implants
may lead to devastating cardiac and neurological effects, osteolysis,
as well as soft tissue damage [10]. Risk factors for the formation of
a pseudotumor are cobalt levels>5μg/l, female gender, pain, and
a high acetabular inclination angle >55° [8]. In our case a massive
pseudotumor process with extensive involvement of bone stockin
the pelvis and femur developed. This is despite normal levels of metal
ionsmeasured andappropriate positioning of implants confirmed on
imaging.
Figure 4: Pathology slides. A well circumscribed fibroblastic proliferation
(A, HE 2x) with extensive collagenization (B, HE 4x) admixed with
lymphoplasmacytic and histiocytic inflammation (C, HE 4x) was recognized.
Metal particles, cement, bone, (D, HE 10x), methacrylate fragments,
and cholesterol crystals (E, HE 20x) were seen embedded. In addition,
hemosiderin deposits were also present (F, HE 20x). A diagnosis of
inflammatory pseudotumor and aseptic lymphocytic vasculitis-associated
lesion was made.
Figure 5: 14 Month follow-up imaging. A- C: plain radiographs of the implants at 14 months follow up visit.
Treatment options include isolated revision of the femoral or
acetabular component, or complete-revision surgery [10]. In many
cases treatment can be performed with the same principles used in
revisions for aseptic loosening. Cementless cups and femoral implants
can often be used in combination with cancellous bone grafting if
the bony defects are not significant. Usually the choice for revision
techniques and implants is dependent on the extent of bony erosion.
However, literature to guide surgical planning of pseudotumors is
limited, especially with large lesions involving extensive bone and
soft tissue damage. Established guidelines for non-pseudotumor
revision THA do not provide adequate guidance. The treatment of
this condition is associated with high reintervention rates requiring
a second revision in almost 35% of the cases. Major complications
occur in up to 50% of cases, with patients often experiencing the same
level of pain and functional limitations as prior to the revision surgery
[3].
Another important consideration is the choice of implant
surfaces used in revision surgery. It is generally advisable to avoid
using a metal on metal coupling when performing a revision for
pseudotumor, options of ceramic on polyethylene are preferred, as
they pose the lowest risk of producing metal ion debris.
This case report details a pseudotumor where the soft tissue
component, and the associated osteolysis wereextensive, making
this one of the largest pseudotumors reported in literature. Due to
the size of the pseudotumor a unique staged surgical plan had to be
implemented. Although traditionally revisions are performed in a
single stage, evaluating the imaging pre-operatively gave the authors
insight into the extent of osteolysis, as well as soft tissue reaction
which caused a large pseudotumor to form. There was concern preoperatively
that the amount of dissection required to thoroughly
debride the pseudotumor would be extensive. Especially at the distal
aspect of the thigh where the capsule was abutting the neurovascular
bundle.
Staging was thought to decrease surgical complications, mainly
infection due to reduction of surgical time in one anesthesia episode [4,10]. Custom implants were indicated in order to address the
irregular and extensive areas of bone loss. Due to the damaged
abductor muscles, a constrained liner was used to decrease the risk
of dislocation. Aggressive release of the fibrosis at the knee joint was
also performed at the time of the standard total femur replacement
procedure, providing improved knee range of motion. The utilization
of both a total femur replacement as well as a custom triflange
acetabular implant was unique in this setting and required extensive
planning and coordination of care. Due to the potentially extensive
nature of the dissection for both the acetabular component fixation
as well as the total femur replacement and the inherent difficulty in
performing these procedures in deficient bone, a more conservative
approach with staging the procedure in order to reduce potential
complications was thought to be appropriate.
With this case report, the authors emphasize the importance of
approaching an extensive pseudotumor with careful planning and
attention to detail. Complete characterization of the lesion preoperatively
is especially important in order to guide appropriate
surgical approach, and implant choices, including custom implants
when necessary.
Case reports such as these are vital in providing practicing
surgeons and researchers with an important fund of knowledge
in unique cases, where large volume research studies are difficult
to perform. Case series and case reports make up the majority of
the available literature in regard to revision surgery secondary to
pseudotumor in total hip arthroplasty, specifically in cases involving
extensive bone loss and large volume formation of pseudotumor.
As there are no well documented guidelines to treatment in these
scenarios, this case report and others can serve as an example for a
successful treatment option.
Conclusion
We recommend a two-stage revision in large complex pseudotumor cases with complete revision of the implants as well as excision of the pseudotumor to achieve clinical improvement and decrease complications. To our knowledge, this is the first case report in which a custom triphalangeal acetabular implant in conjunction with a total femur reconstruction was done with a two-stage revision for treatment of a pseudotumor due to MoM THA.