Journal of Orthopedics & Rheumatology
Download PDF
Research Article
Does a Normal Hip Ultrasound at 3-6 Months of Age Predict a Normal X-ray?
Paez CJ1, Hansen CH1, Bomar JD2, Upasani VV2* and Pring ME2
1University of California, San Diego Medical Center, 200 West
Arbor Drive, MC 8894, San Diego, CA 92103
2Rady Children’s Hospital, San Diego 3020 Children’s Way San
Diego, CA 92123
*Address for Correspondence: Upasani VV, Rady Children’s Hospital, San Diego 3020 Children’s Way
San Diego, CA 92123, USA; Phone (858) 966-6789 / Fax: (858) 966-
7494; E-mail: vupasani@rchsd.org
Submission: 30 September 2021;
Accepted: 04 November 2021;
Published: 10 November 2021
Copyright: © 2021 Paez CJ, et al. This is an open access article
distributed under the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited.
Abstract
Objective: Ultrasound (US) may be used to diagnose/monitor
developmental dysplasia of the hip (DDH) prior to femoral head
ossification, after that, radiographs (XR) may become a better choice.
The objective of this study was to compare US to XR performed on the
same day for diagnosis or monitoring of DDH in patients 3 to 6 months
of age.
Methods: 92 patients (183 hips) ages 3 to 6 months who were seen
for hip screening for DDH were retrospectively reviewed. All patients
had a same-day hip ultrasound and plvis radiograph. Alpha angle, hip
stability, femoral head coverage, acetabular index (AI), IHDI grade,
and break in Shenton’s line were recorded and used to diagnose the
hip as normal or dysplastic.
Results: 17.5% of hips were diagnosed with DDH based on XR, 12%
of hips were diagnosed with DDH on US. Thirteen hips were read as
normal on US but dysplastic on XR. Using XR as the definitive diagnosis,
US had sensitivity of 59% and specificity of 98%. Using US as the definitive
diagnosis, XR had sensitivity of 86% and specificity of 92%.
Conclusion: In the 3-6 month age group, US alone may underdiagnose
hip dysplasia and be inadequate to guide treatment
decisions. In this age group, we suggest that pelvis radiographs be used
when deciding to either initiate or conclude DDH treatment based on
the higher sensitivity of the exam.
Keywords
Ultrasound; Developmental dysplasia of the hip; X-ray vs
ultrasound
Introduction
Developmental dysplasia of the hip (DDH) encompasses a wide
range of pediatric hip disorders from malformation of the acetabulum
to complete dislocation of the hip [1-4]. The incidence of DDH has
been reported as 1-7% of newborns [5], although reported incidences
can vary widely in different populations [6-8]. The American Academy
of Pediatrics Clinical Practice guidelines recommends that patients
with positive physical exam findings be referred to an orthopedic
surgeon for further clinical and radiographic evaluation [1].
Infants less than three months of age with risk factors and/
or physical exam concerning for DDH are typically evaluated with
ultrasonography (US), as the hip structures in this age group are almost
entirely cartilaginous and not well visualized on pelvis radiographs
(XR). As the femoral head ossifies, it creates an acoustic shadow on
US that obscures the portion of the acetabulum behind it, making US
both difficult to perform and less accurate [9,10]. During this time
period, physicians often transition from US to XR to diagnose and
track the progression of DDH. However, the timing for this transition
is often debated. Many advocate for the use of ultrasound as the sole
diagnostic test up to 6 months and some up to 2 years of age in order
to minimize radiation exposure to the infant [11,12].
A combination of static and dynamic ultrasound as described
by Graf and Harke in the 1980’s is commonly used in the pediatric
orthopedic office to diagnose and monitor the progress of DDH in
infants [13,15,16]. Graf characterized the alpha angle, which defines
the slope of the superior portion of the acetabulum [9]. An alpha angle over 60 degrees is considered normal and a smaller angle is
considered acetabular dysplasia [17]. Dynamic ultrasound is an
excellent test for hip instability. However once the hip has been
stabilized, there is debate as to whether or not ultrasound is adequate
for diagnosis of residual acetabular dysplasia.
Pelvis radiographs are used to gauge acetabular morphology,
femoral head ossification, and dysplasia [3]. The acetabular index
is the angle formed by Hilgenreiner’s line and the slope of the
acetabulum on pelvis XR [18]. Larger angles correlate with more
dysplasia [18,19]. XR can also be used to measure the International
Hip Dysplasia Institute (IHDI) grade, which uses the central point
of the proximal femoral metaphysis as a reference point [10]. Similar
to the Tönnis method [14], the hip is divided into four quadrants by
Hilgenreiner’s line (horizontal line through the triradiate cartilages)
and Perkin’s line (vertical line perpendicular to Hilgenreiner’s and
passing through the lateral edge of the acetabulum) and then an
additional diagonal line drawn at 45 degrees from the junction of
Hilgenreiner’s line [10]. Grade I is considered normal; the center
of the proximal femoral metaphysis is located in the inferomedial
quadrant. In grades II-IV, the femoral head is progressively more
lateral and then proximal; higher grade correlates with worsening
dysplasia.
Traditionally, our institution used ultrasound to evaluate infantile
DDH from birth to age three months. At age three months, we
typically switch to x-ray. However, due to a presentation at a national
conference (American Academy of Orthopedic Surgeons - 2017, San
Diego, CA) on the topic of infantile DDH, some of our physicians
began to question the use of x-ray in the three-to-six-month age
group. These physicians began to order ultrasound, as well as x-ray,
in the three-to-six-month age group as they were more familiar with
x-ray in this age group, and this would serve as a way to ultimately
transition from x-ray towards the use of ultrasound.
We have noted both in the literature and in our practice patients
who have a normal ultrasound but later are diagnosed with DDH on XR. It is unclear whether these patients developed dysplasia after the
initial US or if the dysplasia was present but the US was not sensitive
enough to diagnose it. The purpose of this current study was to
directly compare XR to US in infant’s age 3 to 6 months to better
clarify the efficacy of each and to determine appropriate management
of these patients.
Materials and Methods
Following IRB approval, we conducted a retrospective review of
92 patients and 183 hips ages 3 to 6 months who were being evaluated
or treated for DDH at a single institution between November 2017 and
May 2019. All patients who had a hip ultrasound and pelvis radiograph
on the same day were included in the study. One patient did not
have bilateral ultrasound, which excluded one hip from this study.
All ultrasounds were performed by a single ultrasound technician
with over 20 years of experience working solely in orthopedic clinics
treating DDH (Figure 1). Each hip XR and US was measured by two
fellowship trained, pediatric orthopedic surgeons, blinded to patient
identifying information and to the result of the other study (XR or
US). Pelvis radiographs were obtained in a standardized position to
ensure accurate anterior-posterior images without rotation or tilt.
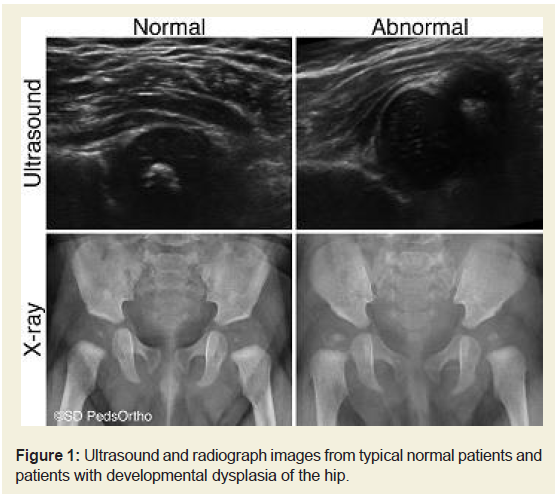
Figure 1: Ultrasound and radiograph images from typical normal patients and
patients with developmental dysplasia of the hip.
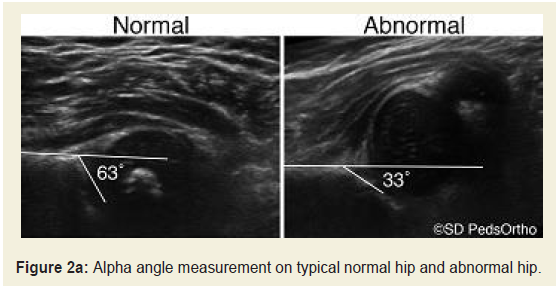
On US, dynamic stability was assessed on both coronal and
transverse views. Any instability was classified as DDH. Instability
was defined as a change in femoral head coverage, as evaluated on
ultrasound, with stress on the hip joint. Alpha angle was measured on
the coronal view on US with the hips flexed to approximately 90˚ and
in neutral abduction (Figure 2a). An alpha angle greater than 60˚ were
considered as normal and an angle less than 60˚ were considered as
dysplastic. Beta angle was not used in this study as the authors felt that
there was too much inter- and intra-rater variability and none of the
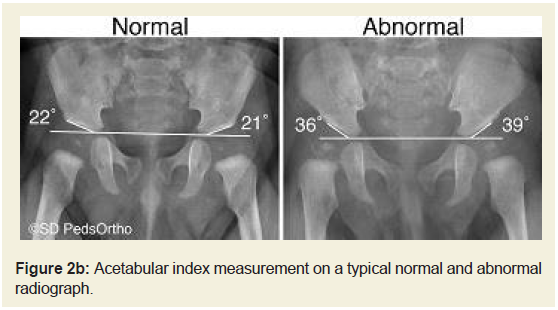
authors use this measure in clinical practice. Acetabular index (Figure 2b), IHDI grade and presence/absence of the ossific nucleus were
determined using the pelvis radiograph. Determination of DDH on
XR was decided based on acetabular index and the IHDI grade (which
includes femoral head coverage/subluxation/dislocation). Hips were
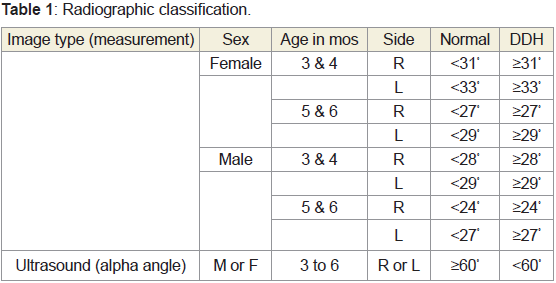
classified as normal or dysplastic based on their measurements compared to the accepted values for their sex, specific age, and
laterality. See Table 1 for details of these values [13,14]. Subjects with
an IHDI grade greater than I were classified as dysplastic, regardless
of their acetabular index. Hips with disagreement between the two
observers were re-reviewed to determine a consensus regarding the
diagnosis. A subset of 24 hips were re-measured greater than two
weeks later to evaluate intra-rater reliability.
Statistical Analysis
Basic descriptive statistics are reported. The unit of analysis was
the hip. All continuous data was evaluated with the Shapiro-Wilk
test of normality and found to be non-normally distributed. This
data was evaluated with the Mann-Whitney test. Gwet’s agreement
coefficient 1 (AC1) adjusted kappa was used for evaluating intermodality
agreement in diagnosing DDH between XR and US due
to the disproportionate number of normal hips. Kappa values were
considered excellent if between 0.8-1.0, good between 0.6-0.79,
moderate between 0.4-0.59, and fair between 0.21-0.39. The intra
class correlation coefficient (ICC) was used to evaluate inter- and
intra-rater reliability of alpha angle and acetabular index. No a priori
power analysis was performed. All analysis was conducted using
SPSS (version 26; IBM, New York, USA). Statistical significance was
defined as p<0.05.
Results
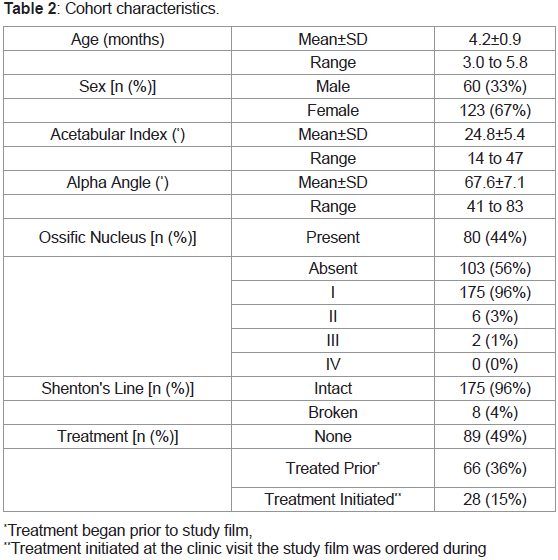
One hundred eighty-three hips in 92 patients were studied. The
majority of patients were female (67%). The mean age of the cohort
was 4.2±0.9 months (range: 3.0 to 5.8 months). The ossific nucleus
was present in 80 hips (44%). Cohort characteristics can be found
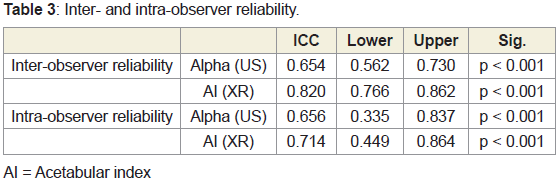
in Table 2. Inter-observer reliability was found to be higher when
measuring acetabular index (ICC=0.820) than when measuring alpha
angle (ICC=0.654). The full ICC distribution can be found in Table 3.
After classifying the 183 hips independently, our two reviewers had the same interpretation for 92% of XR images and 87% of
US images. Both reviewers independently diagnosed 128 hips as
normal on both XR and US. There were 36 hips (14 XRs and 22
USs) with some discrepancy between the two reviewers on at least
one of the measurements. After inter- and intra-observer reliability
was calculated, the two reviewers were again blinded to patient
information and prior reads for this subset of 36 hips and interpreted
the imaging together to determine a consensus. After the consensus,
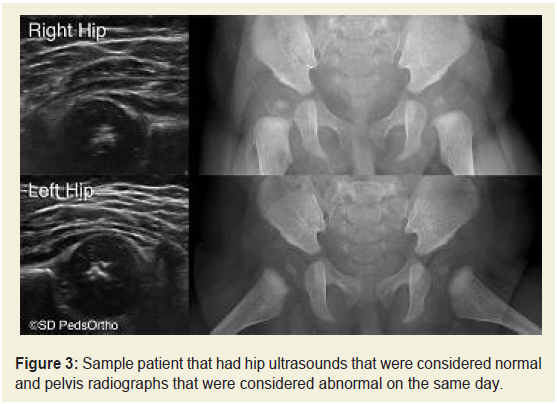
comparisons could be made between US and XR. Nineteen hips
(10.4%) were classified as dysplastic on both US and XR. 148 hips
(80.9%) were classified as being normal on both US and XR. Thirteen
hips (7.1%) were classified as being dysplastic on XR but normal on
US (Figure 3). Three hips (1.6%) were classified as being dysplastic on
US and normal on XR. Three hips (1.6%) with an acetabular index
that was normal for their age/sex were classified as dysplastic based
on an IHDI grade of II, all three had an abnormal ultrasound and a
break in Shenton’s line.
Of the 13 hips that were classified as being dysplastic on XR, but
not on US, all were IHDI grade I, with Shenton’s line intact. Six of
these 13 hips had an absent ossific nucleus. The age range for these
hips was 3.1 to 5.6 months (mean: 4.4±0.9 months). Of the 22 hips
diagnosed with DDH on US, three were ruled as normal on XR. Two
of these hips were classified as mild DDH on US with alpha angles
of 53˚ and 56˚. The remaining hip had an alpha angle of 43˚, with an
acetabular index of 14˚. These hips ranged in age from 3.2 months
to 3.6 months. All three were IHDI grade I with an absent ossific
nucleus. Using XR as the definitive diagnosis, US had sensitivity of
59% and specificity of 98%. Using US as the definitive diagnosis, XR
had sensitivity of 86% and specificity of 92%.
Not surprisingly, hips with an ossific nucleus present were found
to be older (4.6±0.8 months) on average than subjects with an absent
ossific nucleus (3.9±0.8 months) (p<0.001). Six hips with a present
ossific nucleus were found to have DDH via US and all six were also noted to have DDH via XR. Seven additional hips with a present
ossific nucleus were found to have DDH via XR but not on US.
Discussion
In a study by Imrie et. al, 300 patients referred for hip evaluation
due to breech birth position were followed for development of dysplasia [20]. At the initial 6-week screening, 27% of the patients
had an abnormal US. Of the remaining 73% with initial normal
US, 29% had evidence of dysplasia at their 4 to 6-month follow-up
and subsequently underwent treatment for DDH. This subset of
later diagnoses can be explained by the patients either developing
dysplasia after the initial ultrasound or that the initial ultrasound
was simply not sensitive enough to diagnose it. The purpose of our
current study was to compare the efficacy of US to XR with regards to
diagnosis of DDH in infants 3 to 6 months of age. Our study found
that US diagnosed fewer patients (12.0%) with DDH compared to XR
(17.5%). The sensitivity of US was low and the specificity was high.
A test with high specificity will correctly identify hips that do not have DDH. Conversely, a test with high sensitivity will correctly
identify hips that do have DDH. Our finding that US have a high
specificity of 98% indicates that a positive US is sufficient to diagnose
DDH in this age group. The low sensitivity of 59% indicates that a
negative US is insufficient to rule out DDH in this age group. US done
at our institution for evaluation of DDH in 3 to 6-month infants had a
higher number of false negatives than false positives. A false negative
is potentially troublesome when US is used as the only diagnostic
and evaluation tool for DDH. If a patient with DDH is not properly
diagnosed they may not be treated or may have their treatment
stopped prior to complete resolution of DDH.
In this study, ultrasounds that were read as dysplastic correlated
moderately well with XR so we recommend treating for DDH based
on US that shows instability and/or dysplasia, knowing that a small
percentage of patients will be over-treated with a Pavlik or abduction
brace which has a very low complication risk. A normal ultrasound
in the 3-6 month age group does not rule out residual acetabular
dysplasia and may lead to under treatment of DDH if it is the only
diagnostic tool used. Under treating DDH puts the child at risk of
early hip degeneration and osteoarthritis. We therefore recommend
a pelvis radiograph to confirm normal hip development before
releasing the infant from care/treatment. XR has better inter and
intra-rater reliability and is not as operator-dependent or subjective
as US.
Previous studies have made differing recommendations on when
radiographs are the most appropriate modality for assessing DDH
[17,19,21-23]. It is generally agreed that radiographs become more
reliable after 4 months of age and the American Academy of Pediatrics
(AAP) has stated that US and XR seem to be equally effective
between 4 to 6 months of age as the femoral head is ossifying [1].
Many orthopedists predominantly utilize ultrasound until 6 months
of age [10,11]. However, ultrasound is very operator dependent and
reading ultrasounds is quite subjective. The variation in technique
and evaluation may lead to under or over diagnosis of dysplasia by
ultrasound. The AAP has stated that there is no “gold-standard” for
diagnosis of DDH at any point in time and overall there is a paucity of
research to help provide data-driven treatment guidelines [1].
Other studies have directly compared US and XR. Spaans et. al
analyzed US and XR performed on the same day in 74 infants being
treated for stable DDH [24]. Counter to our results, they found that
US was able to diagnose DDH in more hips than XR. However,
similar to us, they found acetabular index and alpha angle to be
poorly correlated. Terjesen et. el also compared US to XR conducted
on the same day in 312 consecutive hips [25]. After excluding normal,
subluxated, and dislocated hips, they also found poor correlation
between US and XR measurements. Similar to our study, radiographs
were able to diagnose DDH in more hips than ultrasonography.
In seven of the fifteen hips with radiographic dysplasia, there were
normal US findings. All patients with abnormal US also had abnormal
XR measurements.
Ultrasound remains an extremely valuable imaging modality for
dynamic assessment of the hip, especially in the first few months of
life when the hip structures are almost entirely cartilaginous. The
combination of static and dynamic US is a valuable clinical tool for the
diagnosis and monitoring of DDH without any radiation risk to the infant. US has been shown to be much better than XR at diagnosing
instability of a hip and should be used until the ultrasound is read as
normal or the femoral head is too ossified to allow good visualization
with US. US remains our primary imaging modality in patients less
than 3 months of age and older if US remains abnormal.
A primary limitation of this study is the prevalence of disease in
this study cohort. Despite the large sample size (183 hips at risk for or
being treated for DDH), there were a small number of hips diagnosed
with DDH (35 hips or 19%) on either XR or US at the time point
where they had both done on the same day. A cohort with a larger
prevalence of DDH could influence our sensitivity and specificity.
However, our cohort reflects the actual distribution of DDH among
subjects seen in our orthopedic clinic for hip evaluation or treatment
during this time period. In addition, this smaller sample of diseased
hips prevented further subset analysis based on potential confounders
such as dysplasia severity and current or prior treatments. We
understand that this does not offer a complete scope of the process
involved in the diagnosis of DDH, but it is our hope that this offers
a compelling platform on which to build further research and
highlights the importance of radiographic imaging in the diagnosis
and treatment of DDH.
In conclusion, our data indicates that in infants age 3 to 6 months,
US missed 13 (41%) of the hips where DDH was diagnosed by XR
performed on the same day. If only US had been done for these 13
hips, they may have been undertreated for DDH that was noted on
XR. We recommend that in the 3 to 6 month age group, treatment
decisions be confirmed by using standard pelvic radiographs. If
ultrasound is normal in a high-risk infant with an unossified ossific
nucleus, we have them return to clinic around 6 months of age to
confirm the normal diagnosis with XR before releasing them from
clinic. If DDH is found on XR at 6 months, there is still adequate time
to treat DDH with a harness or abduction brace.