Journal of Orthopedics & Rheumatology
Download PDF
Research Article
Posterior Pediculectomy and Vertebral Trough-Cut Technique for Reduction of Retropulsed Bone Fragments in Thoracolumbar Burst Fractures: A Surgical Technique and Treatment Algorithm Plan
Gabriel Liu*, Jun-Hao Tan, Jun Cheong Kong, Yong Hao Joel Tan, Nishant Kumar and Jiong Hao Tan
Department of Orthopaedic Surgery, National University Hospital,
National University Health System, 1E Kent Ridge Road 119228,
Singapore
*Address for Correspondence:
Liu G, Department of Orthopaedic Surgery, National University Hospital,
National University Health System, 1E Kent Ridge Road 119228, Singapore;
Email: junhao_tan@nuhs.edu.sg
Submission: 26 November 2021;
Accepted: 10 January 2022;
Published: 17 January 2022
Copyright: © 2022 Liu G, et al. This is an open access article distributed
under the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided
the original work is properly cited.
Abstract
Introduction: This study aims to describe the feasibility and
outcomes of the pediculectomy and vertebral trough-cut technique
to reduce bony fragments in thoracolumbar burst fractures. This allposterior
retrovertebral fragment reduction technique requires the
complete removal of the pedicle, followed by cutting a trough ventral
to displaced retrovertebral burst fragments to create space for easy
posterior to anterior fragment reduction.
Methods: This was a retrospective study of patients with
thoracolumbar burst fractures and canal compromise of more than
50% on axial computed tomography (CT). All patients had neurological
deficits secondary to spinal fracture. Each patient underwent
removal of the pedicle by cutting a trough ventral to the displaced
retrovertebral burst fragment to create space for posterior to anterior
fracture fragment reduction followed by posterior instrumentation and
fusion.
Results: Thirteen patientswith a mean age of 33 (24-50) years
were analysed. All patients’ retropulsed fracture fragments were
approached via a pediculectomy. Additional trough cut was
performed in 9 patients when the retropulsed fragment was deemed
to be irreducible. The average post to pre-operative improvement
in axial compromise was 60.7% while the average improvement
in vertebral height was 33.9% and the average improvement in
vertebral body angle was 9 degrees. All patients experienced mean
improvement in ASIA grade of 2. Eleven out of thirteen of the patients
were able to walk independently at last follow-up.
Conclusion: The pediculectomy and vertebral trough cut
technique for the reduction of retropulsed fragments in burst
thoracolumbar fractures is feasible and reproducible with good
clinical and radiological outcomes.
Introduction
Traumatic fractures at the thoracolumbar junction (T10–L2)
are the most common fractures found in the spinal column [1].
Thoracolumbar burst fractures are the second most common
thoracolumbar fractures after compression fractures with almost
25,000 cases reported annually in the United States [1]. Burst
fractures occur when the vertebral segment is subjected to an axial or
flexionload, which leads to a failure of both the anterior and middle
column of the spine with retropulsion of the posterior vertebral wall
into the spinal canal resulting in neurological injury.
Stable burst fractures with no neurological compromise or
disruption of the posterior osseo-ligamentous complexare managed
with bracing and early mobilization [2]. Unstable burst fracture with
retropulsed bone fragments compromising the spinal canal leading to neurological deficits require surgical decompression, correction of
spinal deformities and fracture stabilization [1,3]. Surgical approaches
employed to expose the retropulsed spinal fragment include
laminectomy, lateral extracavitary techniques, anterior vertebrectomy
and posterior vertebral column reconstruction (PVCR) [3-6].
The aim of this study is to describe the feasibility and outcome
of the use of pediculectomy and vertebral trough cut technique to
reduce bony fragments in thoracolumbar burst fractures. This all
posterior retrovertebral fragment reduction technique requires first
the complete removal of the pedicle (pediculectomy), then followed
by cutting a trough (trough cut) ventral to the displaced retrovertebral
burst fragment to create space for easy posterior to anterior fracture
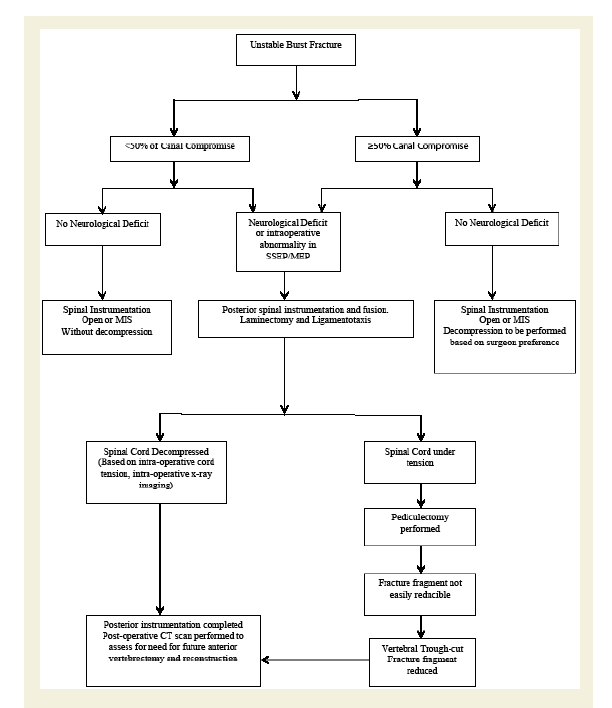
fragment reduction. We also propose a treatment algorithm for the
treatment of unstable burst fractures with neurological deficits.
Materials and Methods
This is a retrospective single surgeon study of patients with
thoracolumbar burst fractures and spinal canal compromise by
retropulsed fracture fragment of more than 50% on axial computed
tomography (CT). All patients had neurological deficits secondary to
spinal fracture and preoperative and postoperative Asia scores were
recorded [7]. Plain radiographs, CT and magnetic resonance imaging
(MRI) were used to assess the level of injury and to determine the
extent of neural compression. Each patient’s fracture was classified
according to the AO spine thoracolumbar classification system [8],
the Thoraco-Lumbar Injury Classification and Severity score (TLICS)
and the Gaines Load Sharing Classification [9,10].
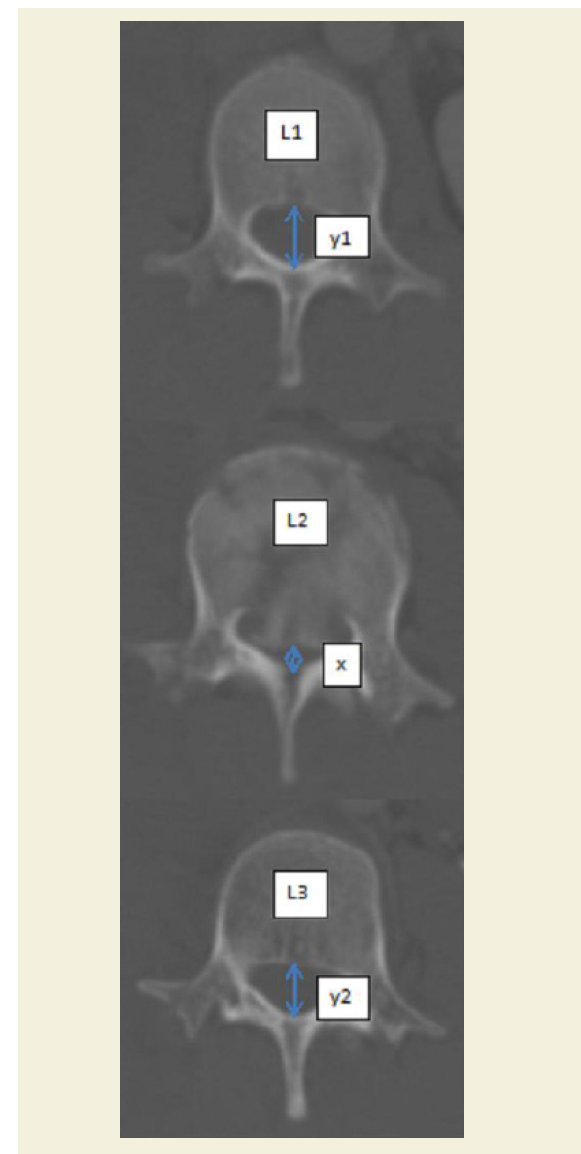
Using pre-operative CT, the percentage of axial canal compromise
was determined using the formula α= (1-x/y) ×100. α is the percentage
of canal compromise, x is the narrowest mid-sagittal diameter of the
spinal canal at the level of injury, and y is the average mid-sagittal
diameter of the spinal canal at one level above and below the injured
segment [5].The vertebral body angle of the fractured vertebral body
was measured as the angle between the upper margin of the vertebral
body and the lower margin of the vertebral body [5].The vertebral body height percentage was determined using the formula = 2F/
(A+B)×100, where F is the height of the fractured vertebral body, A
is the height of the upper vertebral body, and B is the height of the
lower vertebral body [5] (Figure 1). A post-operative CT was then
performed and the above measurements re-measured to document
improvement in canal compromise, vertebral body angle and height.
All perioperative complications and postoperative neurological
compromise was recorded.
Figure 1: Measurement of the percentage of axial canal compromise,
vertebral body angle and vertebral body height percentage.
Surgical Technique:
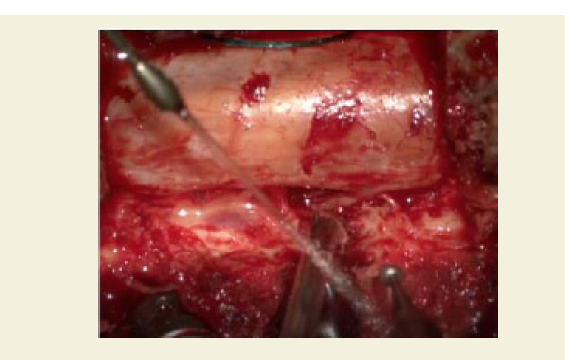
A standard midline posterior approach was performed to expose
the fracture site and its adjacent vertebrae for instrumentation.
Under loupe magnification a laminectomy and partial facetectomy
was performed at the fracture site and the corresponding exiting and
transversing nerve roots were identified and protected. The pedicles of
the fractured vertebrae were identified. With the use of a high-speed
burr a pilot hole was created within the pedicle and then widened
until the pedicle walls become thin and removed with a pituitary
rounger. The author would prefer to remove the pedicle only at the
side where maximum retropulsion of the burst fragment has occurred
(Figure 2a).
Figure 2a: Pilot hole created with high speed burr and widened till pedicle
walls are thin enough to be removed with a rounger.
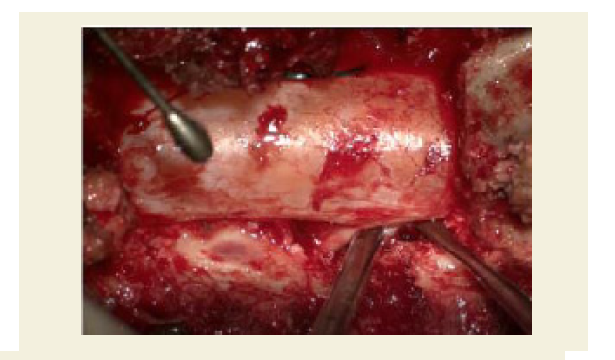
A Penfield and Macdonald were then used to free the dura
posterior to the retropulsed fragments to avoid dural entrapment
within the retropulsed fragments. The Macdonald was then used to
glide over the retropulsed fragments in the midline to gauge the extent
of the displacement. The retropulsed fragment was gently pushed
forward with a reversed angle curette to assess its reductability. Care
was taken to avoid sudden recoil of the curette when attempting to
reduce the fragment into the vertebral body to prevent traumatisation
of the spinal cord (Figure 2b). During fracture manipulation, a nerve root
retractor is used to protect the neural elements and a temporary
rod was then applied on the contralateral side for fracture stability.
Figure 2b: Use of a Penfield retractor to assess extent of retropulsed
fragment and assess reducibility.
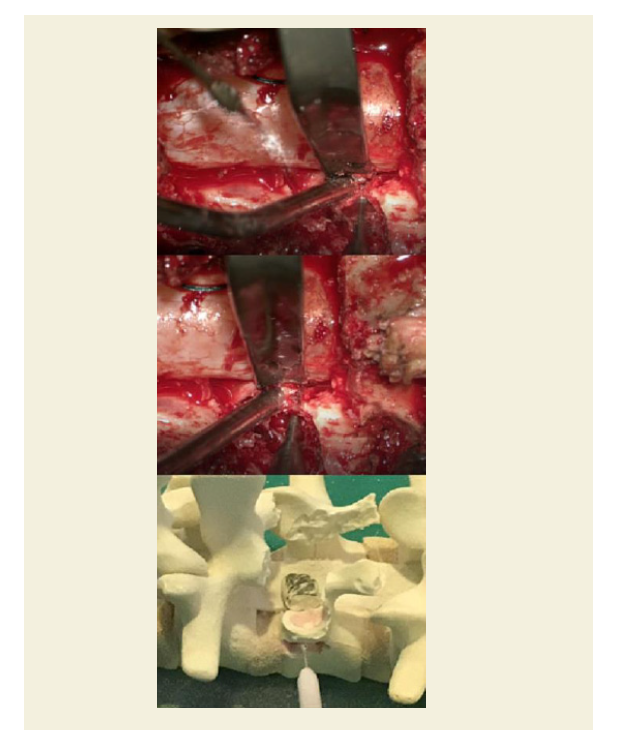
If the retropulsed fragment was not reducible, a trough was then
made along the posterior one quarter of the vertebral body on the
lateral wall where the pedicle was removed. A 3mm ball tipped highspeed
burr (Midas Rex, Medtronic, Minnesota, USA) is used to create
this trough cut from lateral to medial at a depth of 0.5cm below the
posterior vertebral wall (Figure 2c). This weakens the posterior wall
of the vertebrae and creates room to allow the retropulsedfragement
in the midline to be easily reduced into the vertebral body (Figure 2d). After instrumentation, and fracture deformity correction,
posterolateral fusion was performed (Figure 3).
Figure 2c: A high speed burr is used to create this trough from lateral to
medial to a depth of 1cm below the posterior wall.
Figure 3: Preoperative images of a 50 year old male with an L1 burst fracture
after a fall from height. There was more than 50% vertebral canal compromise
with cord signal change and kyphotic deformity. Pre, postoperative and 3 years
post-operative CT scan and radiographs demonstrating reduction of retropulsed
fragment and decrease in canal compromise as well as correction of kyphotic
deformity.
Results
13 patients, 11 male and 2 females with a mean age of 33 years
(range 24-50) were analyzed. The mechanism of injury was fall from
height in 11 patients and motor vehicle accident in two patients. All
patients had an AO type A3 burst fracture. The mean preoperative
TLIC’s score was 7 (6-8) and the mean Gaines score was 5 (4-8).
Neurologically4 patients were ASIA A, 2 patients were Asia B, 3 of the
patients were ASIA C and 4 of the patients were Asia D. There were 2
patients with preexisting dura tears diagnosed on completion of the
laminectomy and these were managed with a Sandwich technique.
Firstly, closure with Prolene 5-0 suture following which medical
adhesive is applied onto the suture line and dural surface. A gelatin
sponge is then trimmed and placed over the tear and its adjacent area following which a second layer of medical adhesive is sprayed over the
gelatin sponge and its edges.
All patients’ retropulsed fracture fragments were reduced via
a pediculectomy. In this series all pediculectomies performed were
unilateral on the side where maximum retropulsion had occurred.
Additional trough cut was performed in 9 patients when the retropulsed
fragment was deemed to be irreducible. None of the patients required
anterior vertebrectomy. Mean operative time was 310 minutes (243-
358) and mean blood loss was 795mls (100-2000). Pre-operatively, the
mean axial canal compromise percentage was 61% (50-90), the mean
vertebrae body height percentage was 59%( 45-80) of the original
height. The mean preoperative vertebral body angle was 15 degrees (7-
28). All patients had radiological improvements postoperatively with
the mean axial canal compromise percentage reduced to 24% (9-39),
mean vertebrae body height percentage was restored to 79% (range
65-95) and the mean vertebral body angle was increased to six (2-10)
degrees. Percentage improvement in axial compromise and vertebral
height was calculated by the following formula (postoperative findingpreoperative
finding)/ preoperative finding) x 100%. The average post
to pre-operative improvement in percentage of axial compromise was
60.7% while the average improvement in vertebral height was 33.9%
and the average improvement in vertebral body angle was 9 degrees.
The mean duration of follow up was 18 months (range 3-120 months).
At the time of discharge from hospital, all patients experienced
improvements of mean 2 grades (1-4) in Asia score. 11/13 of the
patients were able to walk independently at time of last follow-up.
The two patients who were unable to walk upon discharge were both
polytrauma patients who had had multiple lower limb fractures
and were loss to follow up. One patient had a post-operative wound
infection and 1 patient had screw malposition requiring screw
revision surgery.
Discussion
The surgical goals of treatment of for thoracolumbar burst
fractures with spinal canal compression and neurological deficit is
decompression of neural structures, correction of spinal deformity,
spinal stabilization and fusion. However, the ideal surgical technique
to remove or reduce the retropulsed fracture fragment is still up for
debate [11-5]. Surgical decompression and indirect reduction of
fracture by ligamentotaxis have been described [12,,16,17]. The role
of decompression and physical removal of retropulsed fragments
is controversial. Miyashita et al showed that in patients with burst
fractures treated without decompression [18], spinal canal compromise
decreased with time, and all patients with incomplete paraplegia had
improved by at least one Frankel grade at the time of final follow
up. However, in the same study 50% of their patients remained
incompletely paraplegic and had to walk with aids [18]. Fehlings et
al showed in the STASCIS study that surgical decompression of the
compressed spinal cord within 24 hours of injury was associated with
better neurological outcomes [19]. In our hospital, we practice early
fracture stabilization and neuro-decompression of patients with burst
fractures having neurological deficits. All our patients experienced an
improvement in Asia score and 11 out of 13 patients were able to walk
at the time of final follow up. Two of our patients were lost to follow up
and we were unable to record their final ambulatory status, although
both patients had an improvement in their Asia score from Asia A to Asia B while hospitalized but were unable to ambulate due to lower
limb fractures.
Several authors have recommended the use of an anterior
approach to allow for better exposure of the fracture vertebrae and
direct removal of the retropulsed fragments [6,11,15]. However, this
is associated with approach related complications such as intercostal
neuralgia, abdominal wall outpouching and pneumothorax [6,11,15].
In recent meta-analysis the anterior surgical approach in the treatment
of thoracolumbar burst fractures was associated with longer operative
time [20-22], greater blood loss and greater cost when compared to
the posterior approach alone. Similarly Tan et al performed another
meta-analysis and reported that a combined anterior and posterior
approach to thoracolumbar burst fracturesdid not result in additional
improvement in clinical, radiological (including kyphotic deformity)
and functional outcomes [23], but lead to longer operative times,
increased blood loss and prolonged hospital stay when compared to a
posterior approach.
Kim et al described the reduction of the retropulsed burst fracture
fragments into the vertebral body via a prone posterior approach with
laminectomy and minimal facetectomy without the removal of the
fractured bone fragments [24]. The mean postoperative spinal canal
diameter improvement was 38%of total canal diameter at follow-up.
This suggests that repositioning of the retropulsed fragments may
be sufficient to reduce spinal cord compression and compromise.
Packing of the retropulsed fragments within the vertebral body may
contribute to a more compact vertebral body with decreased loss in
vertebral height, and make screw insertion and bone fusion more easy.
In their series, the mean vertebral body height improved significantly
27% after surgery from 41.3% preoperatively to 68.3% postoperatively.
Similarly, in our study the mean improvement in canal diameter was
60.7% and vertebral height restoration was 33.9%. We propose that
the additional improvement in spinal canal restoration was achieved
by the addition of pediculectomy with or without the trough cut
technique.
Kwon et al have reported their fracture decompression experience
by removing the pedicle of the fractured vertebrae via a retroperitoneal
anterior approach and achieved an 81.9 % canal restoration (5). Six
patients (33.3%) had dysesthesia at the incision site due to intercostal
nerve injury. Our technique avoids the complications and operative
time associated with removal of the retropulsed fragment by an
anterior approach. Kaya et al described a posterior transpedicular
approach where they removed the medial and superior wall of
both pedicles to visualise the dural sac and the retropulsed fracture
fragment followed by reduction of the retropulsed fragment into
the fractured verterbrae [4]. They did not report the percentage
of reduction in canal compromise. 23 of the 28 patients in their
study showed neurological improvement after surgery with 71.4%
of patients able to ambulate at 1 year after surgery. In our study all
patients experienced improvement in Asia score, (mean 2 grades
(1-4)) and 11/13 of the patients were able to walk independently at
time of last follow-up. Maciejczak et al and Xiong et al have described
approaches involving a partial or complete pedicle removal combined
with vertebrectomy [25,26]. However our technique avoids the blood
loss and surgical time involved with performing a vertebrectomy.
The concept of pediculectomy with the complete removal of the pedicle at the fractured vertebrae via a posterior approach allows a
tangential path to reach the retropulsed fragment without the need
for cord manipulation or retraction. This provides a safe surgical
corridor for the reduction of bony fragments and avoids iatrogenic
injury due to manipulation of fracture fragments. In addition, post
pediculectomy, the size and reducibility of the retropulsed fragment
can now be assessed easily from the cephalad to caudad direction,
as the pedicule no longer blocks visualisation of the retropulsed
fragment.
Another novelty of the current reported approach is the vertebral
trough cut technique. The concept of the vertebral trough cut is to
create a small trough anterior to the retropulsed fracture fragment.
This is performed by cutting a trough in the lateral wall of the
fractured vertebrae anterior to the retropulsed fragment at the side of
the pediculectomy has been performed. This trough cut creates a void
anterior to the retropulsed fragment, to make way for reduction of the
retropulsed fragments into the fractured vertebral body. This improves
our ability to reduce the retropulsed fragment into the fractured
vertebral body. The use of pediculectomy and vertebral trough-cut
technique provides a wide surgical corridor to reach the contralateral
pedicle without the need to remove part of the contralateral pedicle
as described by Kaya et al [4]. The reconstitution of the retropulsed
fracture fragment into the injured vertebral may lead to better bone
healing and vertebral height maintenance and reduce the risk of
failure of the posterior vertebral construct. Furthermore, the void
created by the trough cut adds safety to preventre-herniation of the
reduced spinal fracture fragments into the spinal canal, which was
confirmed in our post-operative CT scan results.
One of the limitations of our study was the small number of
patients in this series and the need for a comparison group to better
evaluate and compare the clinical outcomes. However, the aim of this
study is to demonstrate the proof of concept of the new technique and
its potential benefits.A treatment algorithm for the surgical treatment
of thoracolumbar burst fractures via an all posterior approach using
pediculectomy and vertebral trough-cut is described (Table 1).
Conclusion
In conclusion, the novel pediculectomy and vertebral trough cut
technique for the reduction of retropulsed spine fragments in burst
fractures is feasible, safe and reproducible. It is able to provide good
radiological and clinical outcomes with minimal post-operative
complications. Further larger prospective studies are needed to
further validate this concept.