Journal of Orthopedics & Rheumatology
Download PDF
Case Report
Monoparesis by Herpes Zooster in an Immunocompetent Patient - Case Report
Silva R*, Freitas EF, Moreira E, Branco R, Ferreira F and Oliveira C
Department of Orthopedics and Traumatology, ULSAM - Viana do
Castelo, Portugal
*Address for Correspondence:
Silva R, Department of Orthopedics and Traumatology, ULSAM - Viana
do Castelo; Portugal; E-mail: Almost_romulo@hotmail.com; Phone:
+351914014259
Submission:13 September 2022
Accepted: 10 October 2022
Published: 14 October 2022
Copyright: © 2022 Silva R, et al. This is an open access article
distributed under the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited.
Abstract
Herpes Zoster is caused by the Varicella Zoster virus, characterized
by a unilateral vesicular rash, usually restricted to a specific dermatome.
It occurs by reactivation of the latent virus in the dorsal spinal cord
ganglion, normally associated with isolated sensory changes. Motor
deficits and muscle atrophy of the corresponding myotome are rare
manifestations of this pathology.
We present a case of Herpes Zoster neuropathy in the L5-S1
territory, with early presenting motor dysfunction.
Keywords
Varicella Zoster; Immunocompetent; Foot weakness
Introduction
Varicella Zoster virus (VZV) can have two clinical presentations,
varicella (chickenpox) or herpes zoster (shingles) [1].
Herpes zoster is characterized by a painful and unilateral rash,
usually restricted to one dermatome, although it can affect adjacent
ones, usually in immune-compromised patients. It has a reported
incidence of 10-20%, with higher rates in the elderly and immuno
suppressed population [2].
Despite its rarity, the virus can cause motor neuropathy in 0.5-
5% of patients [3]. This atypical presentation can occur by several
mechanisms: 1- Infection progression to the anterior horn through the
motor nerve root; 2 - segmental myelitis; 3- secondary degeneration
of the motor nerve root; 4 - Simultaneous inflammation of the motor
and sensory system [4].
The diagnosis is based primarily on the history and clinical
findings such as pain, skin rash and development of neurological
deficits in the corresponding territory [5].
Electromyography is an important accessory method to confirm
the diagnosis, revealing alterations in the motor evoked potentials in
muscle groups [6].
Clinical Case
A 65-year-old man visited the Orthopedics Department with
right foot weakness, without lumbar or sciatic pain. A week later he
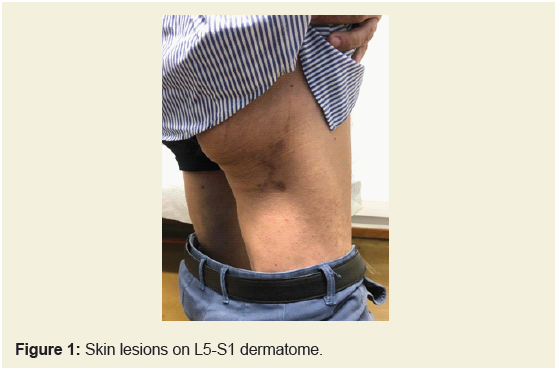
developed right-sided petechiae in the L5-S1 dermatome (Figure 1).
The patient had no relevant pathology or medical history of surgeries/
trauma.
He was unable to dorsiflex the right hallux and ankle (2/5),
with abolition of the Achilles tendon reflex (S1) and dysesthesia in
the lateral side of the right leg and foot. The remaining neurological
examination was normal.
We performed a lumbar MRI that excluded the differential
diagnosis of radicular compression that could be responsible for the
neurological deficits.
A histopathological analysis of the dermal alterations was
performed, with positive varicella-zoster staining. Serological tests
for HIV, Lyme disease, Hepatitis B and C, CMV, Epstein Barr and
Syphilis were negative on serum samples.
The electromyogram revealed severe acute muscular denervation
on the L5/S1 myotomes, compatible with severe radicular ganglionic
neuritis and/or neuropathy of the common sciatic trunk.
Based on these results, a multidisciplinary group meeting
was created with the departments of Orthopedics, Neurology and
Physical Medicine and Rehabilitation to define the treatment of
the patient. We decided for pharmacological treatment with 10
days of Valaciclovir and 3 months of Pregabalin, associated with an
intensive physiotherapy regimen for 4 months. During the follow-up
consultations, there was a complete recovery of muscle strength (5/5),
despite maintained dysesthesia in the foot. A new electromyography
demonstrated a mild to moderate proximal axonal sequel lesion of
the right sciatic nerve.
Discussion
Focal segmental paralyzes are described in up to 5% of Herpes
Zoster cases, occurring in myotomes corresponding to dermatomes
with skin rashes [5], and usually occur 2 to 3 weeks after the beginning
of skin manifestations [8], which statistically highlights the rarity of
our case.
Yoleny, et al. emphasize the underestimation of these values since
the majority of patients develop herpes zoster in regions of the facial
nerves, high cervical (C2-C3) nerves or dorsal roots, regions in which
motor involvement is more difficult to detect.
In the described cases of non-segmental paralysis, diabetic
neuropathy has always been implicated [7], a comorbidity that is duly
excluded in the case presented here.
Aging appears to be the most common cause of viral reactivation,
via weakening of the immune system. It is important to search for
other causes of immunodepression, like HIV or immunosupressive
drug therapy. Our patient was screened for these main comorbidities,
but only tabbaco use was found.
The exact pathophysiology of peripheral neuropathy caused by
herpes zoster is uncertain, but migration of the dorsal spinal ganglion
infection to the nerve root and peripheral nervous system has been
documented [1,6,7].
Saxena, et al. reported a case in which motor neuropathy precedes
skin changes, underlining the uncommonness of such occurrence.
Conclusion
Motor neuropathy following Herpes Zoster reactivation is a
rare entity, especially when the neurological deficits precede the
skin presentation. It is paramount to include this pathology in the
differential diagnosis of the patients who attend our consultations
with ad initium neurological deficits.
Strong clinical suspicion and a multidisciplinary performance are
important to minimize complications and optimize results.