Journal of Orthopedics & Rheumatology
Download PDF
Non-steroidal anti-inflammatory drugs (NSAIDs),
Glucocorticoids,
Conventional synthetic DMARDs: methotrexate (MTX),
cyclophosphamide,sulfasalazine, leflunomide, antimalarials,
azathioprine, colchicine, ciclosporin, tacrolimus,
mycophenolate mofetil (MMF),intravenous immunoglobulin
(IVIG)
Targeted syntheticDMARDs: tofacitinib.
Biologic (biologic response modifier) DMARDs:
Tumour necrosis factor inhibitors (TNFi) (adalimumab,
certolizumabpegol, etanercept, golimumab and
infliximab),
The T cell co stimulation inhibitor abatacept,
The anti-B cell agents rituximaband belimumab,
The interleukin (IL)-6 receptor-blocking monoclonal
antibody tocilizumab, and
The IL-1 receptor antagonistanakinra
Review Article
Arthritis and Planning Conception
Gagandeep Anand 1* and Tania G Singh 2
1MBBS; MS(Orthopaedics) Fellowship Trauma. Fellowship Joint
Replacement Surgery Medical Superintendent and Head of Department
(Orthopaedics) Banarsidas Chandiwala Institute of Medical
Sciences, New Delhi Director GNS Hospital, Chattarpur, New
Delhi, India.
2MBBS; MS(Obs/Gynae); FIAOG Associate member Royal College of Obstetrics and Gynaecology,UK Managing Director GNS Hospital, Chattarpur, New Delhi, India
2MBBS; MS(Obs/Gynae); FIAOG Associate member Royal College of Obstetrics and Gynaecology,UK Managing Director GNS Hospital, Chattarpur, New Delhi, India
*Address for Correspondence
Dr. Gagandeep Anand MBBS; MS(Orthopaedics) Fellowship
Trauma Fellowship Joint Replacement Surgery Medical Superintendent
and Head of Department (Orthopaedics) Banarsidas
Chandiwala Institute of Medical Sciences, New Delhi
Director GNS Hospital, Chattarpur, New Delhi, India. E-mail id:
robbz79@googlemail.com
Submission: 02 May 2023
Accepted: 31 May 2023
Published: 05 June 2023
Copyright: © 2023 Anand G, et al. This is an open-access article
distributed under the Creative Commons Attribution License,
which permits unrestricted use, distribution, and reproduction in
any medium provided the original work is properly cited.
Keywords: European League Against Rheumatism (EULAR); Rheumatoid Arthritis; Osteo Arthritis
Abstract
Arthritis is a form of joint disorder characterized by chronic
inflammation in one or more joints that usually results in pain and is
often disabling. Rheumatoid arthritis (RA) is a chronic, systemic,
debilitating, chronic inflammatory autoimmune disease of synovial
joints, which can lead to chronic pain and structural joint damage,
as well as other organ involvement, especially if not adequately
controlled. The etiology of RA is still unknown. Patients with rheumatoid
arthritis have special family planning considerations that require a
frank discussion and careful coordination with health care providers.
More than 2/3rdof patients experience improvement or even remission
of arthritis during gestation. The improvement in RA symptoms can be
seen both with changing the eating pattern as well as with inclusion
and exclusion of certain food items in the diet.
Osteoarthritis, commonly known as wear and tear arthritis, is a
progressive disease of the elderly, but is also found in athletes and
young individuals who use their joints more. The Western Ontario and
McMaster Universities Arthritis Index (WOMAC) is widely used in the
evaluation of Hip and Knee Osteoarthritis. Diet and exercise has a
major role in alleviating the symptoms of osteoarthritis.
Arthritis- an Overview
The term arthritis is derived from the Greek words “artho” and
“itis,” meaning joint and inflammation, respectively. Arthritis is a
form of joint disorder characterized by chronic inflammation in
one or more joints that usually results in pain and is often disabling.
Arthritis includes more than 100 different forms: the most common
form is osteoarthritis, but other forms include rheumatoid arthritis,
psoriatic arthritis, and related autoimmune diseases [1-2].
Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a chronic, systemic, debilitating,
chronic inflammatory autoimmune disease of synovial joints,
which can lead to chronic pain and structural joint damage, as well
as other organ involvement, especially if not adequately controlled.
Rheumatoid arthritis affects approximately 1% of the world
population [3]. The disease severely impacts quality of life with
increased morbidity and reduced life expectancy. Environmental
factors blended with abnormal immune reactions and genetic factors
are responsible for full expression of the disease. Because it can
affect women in their reproductive years, care of pregnant women
with RA requires a delicate balance of maintaining disease control
while limiting potential toxicity to the fetus and neonate. While most
women experience a substantial improvement in disease activity
during pregnancy, for some women their RA remains active.
Etiopathogenesis:
The etiology of RA is still unknown. The most significant
genetic risk factors for rheumatoid arthritis are variations in human
leukocyte antigen (HLA) class II genes, especially the HLA-DR1
and HLA-DR4 gene [4] that presumably interact with T cells. The
frequency of HLA-DRB1 genes that encode for the so-called shared
epitope, an amino acid motif in the third hypervariable chain of the DRβ1 chain, is increased in RA patients [5]. The MHC (major histocompatibility complex) associations with RA also provide the clearest demonstration that the presence of anti-cyclic citrullinated peptide (anti-CCP) antibodies constitutes a distinct genetic subgroup of RA [6].The early stages of RA are dominated by activated T cells (30–50%
in thesynovia), mainly of the CD4+ T helper type. Failure of regulatory
T cells to control autoimmune effector T cells, may contribute to the
chronicity of joint inflammation. There is evidence for the dominance
of T helper cell type 1 (Th1) cytokines in early stages of RA [7]. Later, T
helper cell type 2 (Th2) features emerge. The chronic stage of arthritis
is characterized by the presence of macrophages and their products.
The role of B cells in RA pathology has been highlighted by the
clinical improvements in RA patients receiving B-cell-depleting
therapies such as rituximab, an anti-CD20 antibody [8]. In addition to
producing antibodies, pro inflammatory cytokines and chemokines,
B cells efficiently act as antigen-presenting cells themselves and thus
influence T-cell activation and expansion [9-10].
Other, non genetic factors are also believed to play a role in
rheumatoid arthritis. These factors may trigger the condition in
people who are at risk, although the mechanism is unclear. Potential
triggers include changes in sex hormones (particularly in women),
occupational exposure to certain kinds of dust or fibers, and viral
or bacterial infections. Long-term smoking is a well-established risk
factor for developing rheumatoid arthritis [11]; it is also associated
with more severe signs and symptoms in people who have the disease.
Early environmental factors such as high birth weight promote
chances of development of RA and early start of breast feeding reduces
chances of development of RA [12]. An altered intestinal micro biota
has thus been implicated in the Etiopathogenesis of RA [13-15].
Rheumatoid Arthritis and Family Planning:
Patients with rheumatoid arthritis have special family
planning considerations that require a frank discussion and careful
coordination with health care providers. It is now well established
through large observational prospective studies that women with
RA often experience a spontaneous improvement or stabilization of
their disease during pregnancy [16-17] but only to flare postpartum.
Ideally, RA should be controlled for 3 to 6 months before attempting
pregnancy. Women who have uncontrolled rheumatoid arthritis may
be at increased risk of developing complications during pregnancy
such as preterm birth and delivering small for their gestational age
babies, requiring neonatal intensive unit care after birth.As RA is a chronic, female-predominant inflammatory disease
that may affect women and men during their reproductive years [18],
it is found that some women with RA may experience sub fertility
with majority facing an unexplained sub fertility or caused, to a lesser
extent, by an ovulation [19-22]. It is increasingly being linked with
the periconceptional use of NSAIDs [23]. Few authors have related
the use of NSAIDs to the occurrence of luteinized unruptured follicle
(LUF) syndrome [24-27], wherein ovulation is inhibited without
changes in menstrual cycle length and cycle regularity and they
may be treated as normal ovulating women. The second issue to
be addressed is the limited frequency of intercourse due to painful
joints [28]. Embryo implantation is however not compromised in RA
patients as is shown by a higher pregnancy rates after IVF and IVF/
ICSI (intracytoplasmic sperm injection) treatments in these women
when compared to controls [29].
In females where RA is diagnosed before completion of their
families, the time to pregnancy exceeds 12 months in as many as 36-
42% of cases [30-31] as compared to 10-17% in general population
[19,32-33].This longer duration to get pregnant can lead to more
damage to the joint.
Preconceptional Counselling:
As rheumatoid arthritis is becoming less disabling these days with
better treatment modalities, more and more females are choosing to
pursue pregnancy. Disease activity may decrease for some, but not for
all pregnant women with RA. Preterm birth is more common among
women with RA than among healthy women, which may be explained,
in part, by disease activity and/or use of certain medications. Family
planning consultation with Rheumatologist and Obstetrician before
trying for conception is an essential prerequisite and should be done
minimum three months prior to planning conception. There can be
certain factors that can make conception more difficult. Screening for
such factors is important, so also to change certain medications before
conception and switching over to safer drugs which are not harmful
for the fetus. Few lifestyle factors can negatively impact fertility.
This allows to keep arthritis controlled in a way that may be safer
for the offspring. Keeping arthritis under control is important since
active inflammation can make it more difficult to conceive or increase
the risk of negative pregnancy outcomes. Ingestion of any herbal
formulas, supplements or vitamins need to be discussed in detail.
Medicines should never be stopped on your own as it may worsen
the existing condition. In case the health condition is not favourable
and pregnancy is not advisable, contraception should be discussed in
length. Contraception is safe for women with rheumatoid arthritis.Changes to the diet, exercise or routine physical activity for weight
management, and other lifestyle factors are advised. Its ‘important to
stay active during pregnancy, inculcating range-of-motion exercises
in daily routine to keep the joints flexible. Certain symptoms unique
to pregnancy can be seen in rheumatoid arthritis, such as low back
pain, fatigue, nausea, swollen ankles, feet or hands.
Postpartum flares are very common. Therefore, visit to a
rheumatologist should be a part of the postnatal care.
While discussing the preconception care with a couple, male
partner needs to be taken into consideration. In case the male partner
is suffering from RA, implications of DMARDs and biologics on male
fertility and family planning need to be discussed. Currently, the
existing data is very limited and only a few case reports are available
on influence of these drugs on the male fertility.
Disease Manifestations:
Rheumatoid arthritis is the most common single cause of chronic
synovitis, affecting multiple diarthrodial joints in a characteristic
distribution, leading to pain, deformities and a reduced quality of life.
The disease is two to three times more common in women than in
men, which may be related to hormonal factors.RA is characterized by symmetrical polyarthritis, for example, if
joints in the hand are affected, both hands tend to be involved [34]
which gets worse after a long rest or on getting out of bed in the
morning. The most common signs and symptoms are pain, swelling,
and stiffness of the joints. Small joints in the hands and feet are
involved most often, although larger joints (such as the shoulders,
hips, and knees) may become involved later in the disease. The disease
may appear in phases with flare ups and remissions and need not be
persistent throughout life in milder cases. Continuous health issues
related to disease may be seen in severe cases leading to severe joint
damage restricting mobility.
The extra articular manifestations include subcutaneous nodules,
lung disease, pericarditis, neuropathy, and vasculitis.The disease can
also manifest with other signs and symptoms such as generalised
weakness, a low grade fever, weight loss, anemia.Furthermore,
patients with RA generally complain of gastrointestinal tract problems
particularly dyspepsia (bloating, postprandial fullness, nausea, early
satiety, epigastric pain, burning and belching), mucosal ulceration,
and altered bowel habits (constipation/diarrhoea) [35].
Effects of Arthritis on Pregnancy:
Every pregnancy is unique. More than 2/3rd of patients experience
improvement or even remission of arthritis during gestation [36-38].
Most of these patients start seeing an improvement in symptoms by
the end of the first trimester with the ease in symptoms sustaining
throughout pregnancy.In few patients where the disease is inadequately controlled,
certain symptoms get exaggerated. Joint pain and pressure on joints
may increase especially upon climbing the stairs. With weight gain
and fluid retention in pregnancy, weight bearing joints like knees,
ankles and feet may pain due to this increased pressure. Fluid
retention may make the extremities swell but if swelling is severe, the
causes may be different and this should be notified. With enlarging uterus, the pressure on the back and spine increases which can result in back pain, back muscle spasms, or numbness and tingling in the
legs.
The diaphragm is pushed upwards as the pregnancy advances,
leading to shortness of breath or at times dizziness. These symptoms
should be discussed with both the rheumatologist and the obstetrician.
Weight gain in pregnancy should be within the given range for a
specific population. Measuring the BMI of the patients helps to allow
a particular range of weight gain in pregnancy. Putting on extra kilos
further weakens the damaged joints. Eating a balanced diet and
keeping an active lifestyle is the key to success. A healthy exercise plan
can be drafted for each patient.
As stated earlier, there is aslight increase in prematurity and
intrauterine growth restriction in patients with active disease,
whereas, in rest of the patients the course of pregnancy and outcome
is favourable in RA [39-40].
One should use the same joint protection techniques which were
always used to prevent pain and injuries: range-of-motion exercises,
good posture, hot or cold packs on sore joints, splints or assistive
devices for support, if the need arises, and good sleep habits. Wearing
comfortable, supportive footwear prevents slips or falls.
Its also normal during pregnancy to feel irritated, anxious, tired or
stressed out. Being pregnant and having a chronic rheumatic disease,
with extra medical appointments, tests or concerns, can put a strain
on the patient’s emotions too. Talking to the doctor and discussing
the questions and the concerns, may relax the woman.
An extra care is needed after delivery as relapse is certain in 90%
of patients within the first 3 months [38].After delivery, the maternal
system adjusts again to then on pregnant state. The postpartum flare
of RA could be related to the following:
Decrease in steroid hormones [41],
The re-establishment of a Th1-dominated immune response,
and
The unopposed action of pro-inflammatory cytokines [42].
Rheumatoid Arthritis Drug Safety in Pregnancy:
The desire to start a family adds additional complexity to
management decisions preconception, during pregnancy and
following delivery, given the lack of safety data and potential
teratogenicity of available therapies. Well-established data supporting
the safe use of medications in pregnancy and lactation are available
for a few medications, while for many others the safety profile is
much less certain. It is important to tailor a treatment regimen that
stabilises the woman's disease prior to conception, using medications
that are safe to continue throughout pregnancy and postpartum. The
drugs used for rheumatoid arthritis, in general, are:
A European League Against Rheumatism (EULAR) task force
[43], on anti rheumatic drugs during pregnancy and lactation, was
established to define points to consider on use of anti rheumatic drugs
before pregnancy, and during pregnancy and lactation by identifying
and critically evaluating recent literature and registry data. EULAR
is a multidisciplinary committee consisting of 20 members from
10European countries and the USA. According to this task force, the
drugs can be used in the following manner:
Safe in Pregnancy: Hydroxychloroquine, chloroquine,
sulfasalazine, azathioprine, ciclosporin, tacrolimus and colchicine.
They should be continued in pregnancy for maintenance of remission
or treatment of a disease flare.
Teratogenic Drugs: methotrexate, mycophenolate mofetil and
cyclophosphamide
Limited Safety in Pregnancy: Non-selective COX inhibitors
(non-steroidal anti-inflammatory drugs, NSAIDs) and prednisone
are used only to control active disease symptoms. NSAIDs should be
restricted to the first and second trimesters.
Severe, refractory cases: Use of methylprednisolone pulses,
intravenous immunoglobulin or even second or third trimester use of
cyclophosphamide should be considered.
Biologic DMARDs: Continuation of tumour necrosis factor
(TNF) inhibitors during the first part of pregnancy should be
considered. Over the last decade, tumour necrosis factor inhibitors
have been used increasingly in the periconceptional treatment
of women with RA, and appear to be safe [43] as compared to the
earlier reports where the biologics including anti-TNF agents, were
recommended to be stopped before pregnancy [44].
The major change in the EULAR consensus paper was the support
given to TNFi use in first half of pregnancy. The paper suggested that
the difference in placental transfer related to molecule structure and
half-life needs to be taken into account when selecting a TNFi for
women of fertile age. As a consequence, infliximab and adalimumab
may preferentially be stopped at20 weeks, but can be continued
throughout pregnancy, if indicated. Etanercept should preferably be
stopped at week 30–32 of pregnancy but if needed, can be continued
till term.
The safety of certolizumab in using it throughout pregnancy
still needs further confirmation by extended published reports.
But the current evidence indicates no increased rate of congenital
malformations, therefore, certolizumab can be continued throughout
pregnancy, if necessary.
Sound evidence forfetal/child safety is still lacking for golimumab,
abatacept, tocilizumab, rituximab, belimumab and anakinra, but SLR
and registry data do not suggest any evidence of harm from these
agents when used before conception or in the first trimester.
In nearly 1/3rdto ½ of the cases, pregnancies are unplanned. As the
woman gets to know that she is pregnant, it’s already the 5-6th week of
pregnancy, and organogenesis has already begun. It becomes difficult
to manage such cases, especially, in women receiving Teratogenic
drugs. Termination of pregnancy or continuation of pregnancy then
becomes a major dilemma. Therefore, the women who are planning
pregnancy in the near future should be switched over to the safer
drugs compatible with pregnancy so that even if they enter pregnancy
the drugs need not be changed.
Also the changing of drugs during pregnancy may flare up the
disease, which becomes difficult to manage with the growing weight of
the fetus. Another point of discussion is the effect of these drugs on the
babies. Switching over to drugs that are considered safe in pregnancy
should be a part of routine prenatal counselling but at the same time
those drugs should not have any long term effects on children after
birth. Studies on the long-term effects of drugs administered during
pregnancy and/or breast feeding on child health and development are
scarce, and often of low quality. The data available for azathioprine,
ciclosporin and dexamethasone do not indicate immunosuppression
in exposed children or raise special concern in regard to physical
or neurological development. By contrast, biologics with extensive
placental transfer achieving high serum levels in the child when
administered after gestational week 30 might increase the risk of
postnatal infection. Children exposed to biologics only before week
22 can receive vaccinations according to standard protocols including
live vaccines. Children exposed at the late second and during the
third trimester can follow vaccination programmes, but should not
receive live vaccines in the first 6 months of life. When available,
measurement of child serum levels of the biologic in question could
guide the decision for or against a live vaccine.
Inheritance Pattern:
The inheritance pattern of rheumatoid arthritis is unclear because
many genetic and environmental factors appear to be involved.
However, having a close relative with rheumatoid arthritis likely
increases a person's risk of developing the condition.Dietary Interventions in Rheumatoid Arthritis:
Several studies advocate the role of altered microbiota in the gut
of RA patients being responsible for pathogenesis as well as disease
progression [14, 45-46]. Since RA is an inflammatory-destructive
joint disease, a dysbiotic intestinal flora, characterized by the loss
of beneficial bacteria and a concomitant increase in potentially
pathogenic microbes, is associated with chronic inflammatory
syndromes [14, 47].Recently, it has been confirmed that the
spore-forming probiotic strain Bacillus coagulans may have antiinflammatory
and immune-modulating effects in both animals and
humans. On the other hand, the prebiotic insulin also potentially
influences immunity by changing the gastrointestinal microbiota
composition and fermentation profile [48].Loss of intestinal microbiota and obesity are important factors,
playing a major role in the development and progression of the disease.
Both can be corrected to a large extent through diet management
[49]. Obese RA patients show a higher degree ofsynovitis even after
remission is achieved [50].Obesity may increase RA activity. In a
systematic review involving 13 studies on the relationship between
serum leptin levels (a protein produced by adipocytes) and rheumatoid
arthritis, it was found that plasma leptin level was significantly higher
in the RA group than in healthy controls, especially in RA patients of
Caucasian, Turkish, or Arab origin [51].
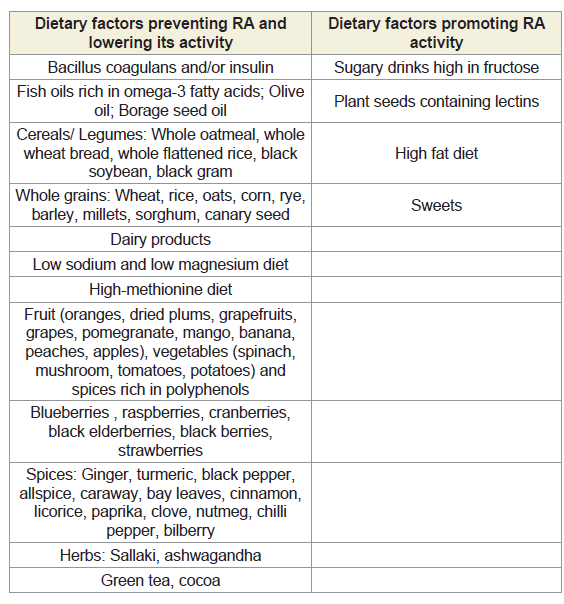
Role of certain Dietary Factors in Preventing Rheumatoid Arthritis:
Diet plays a major role in any disease prevention or its progression,
if adopted at an appropriate time. The improvement in RA symptoms
can be seen both with changing the eating pattern as well as with
inclusion and exclusion of certain food items in the diet.Changing the Eating Pattern
Role of Therapeutic Fasting:
Fasting has been practised for thousands of years and is a staple
across many different religions and cultures around the globe. Today
new varieties of fasting put a new twist on the ancient practice.Several clinical studies have shown that therapeutic fasting
produces anti-inflammatory effects. Fasting leads to an improvement
of the symptoms in many patients with rheumatoid arthritis and
is regularly used by the applicants for the treatment of rheumatoid
arthritis according to various studies.
Fasting alters cellular metabolic pathways and affects immune
function through its impact on cell trafficking and proinflammatory
cytokine expression. There is a much ongoing debate in literature
on Intermittent fasting (IF) and Fasting mimicking diets (FMDs).
Popular examples of intermittent fasting are as follows [52-55]:
16/8 fasting diet: This is one of the most popular styles of fasting.
Healthy eating is limited to a single 8-hour window every day and
abstaining from food for the remaining 16 hours of the day. It is
generally considered less restrictive, and more flexible than many
other diet plans and can easily fit into just about any lifestyle. There
are no strict rules and regulations. It is easy to follow and sustainable
in the long term.
Restricting daily food intake may cause weakness, hunger,
increased food consumption and weight gain. Animal studies show
that intermittent fasting may impact men and women differently and
may even interfere with fertility [56].
5:2 fasting diet: Healthy eating for 5 days per week, and limiting
calories to between 500 for women and 600 for men for 2 days a week.
Intermittent fasting seems to be easier to follow than continuous
calorie restriction, at least for some people [57-58].
Also, many studies have shown that different types of intermittent
fasting may significantly reduce insulin levels. One study showed that
the 5:2 diet caused weight loss similar to regular calorie restriction.
Additionally, the diet was very effective at reducing insulin levels and
improving insulin sensitivity [59].
Alternate day fasting (ADF): Fasting every other day, and healthy
eating during non-fasting days. Studies show that many people find
alternate-day fasting much easier to stick to than traditional, everyday calorie restriction [60-61]. ADF seems to be particularly effective for weight loss among middle-aged people [62].
The most common version of this diet involves “modified”
fasting, where it is allowed to consume 500 calories on fasting days.
Research agrees that modified ADF with 500 calories on fasting
days is much more tolerable than full fasts on fasting days [63].
Furthermore, combining ADF with endurance exercise may cause
twice as much weight loss than ADF alone and six times as much
weight loss as endurance exercise alone [64].Studies have shown that
ADF doesn’t increase compensatory hunger as much as continuous
calorie restriction [65-66].Compensatory hunger refers to increased
levels of hunger in response to calorie restriction, which cause people
to eat more than they need to, when they finally allow themselves to
eat.
Warrior Diet: Fasting over a 20-hour window and then eating
one large meal during a 4-hour evening window.
One meal a day (OMAD): Fasting for 23 hours and eating daily
calories during a1-hour window.
Fasting is an effective treatment for rheumatoid arthritis, but
most patients relapse on reintroduction of food. The effect of
fasting followed by one year of a vegetarian diet was assessed in a
randomised, single-blind controlled trial by Kjeldsen-Kragh et al
[67]. Twenty seven patients were allocated to a four-week stay at a
health farm. After an initial 7-10 day subtotal fast, they were put on
an individually adjusted gluten-free vegan diet for 3·5 months. The
food was then gradually changed to a lacto vegetarian diet for the
remainder of the study. A control group of 26 patients stayed for four
weeks at a convalescent home, but ate an ordinary diet throughout
the whole study period. After four weeks at the health farm, the
diet group showed a significant improvement in number of tender
joints, Ritchie's articular index, and number of swollen joints, pain
score, and duration of morning stiffness, grip strength, erythrocyte
sedimentation rate, C - reactive protein, white blood cell count, and
a health assessment questionnaire score. In the control group, only
pain score improved significantly. The benefits in the diet group were
still present after one year, and evaluation of the whole course showed
significant advantages for the diet group in all measured indices. This
dietary regimen seems to be a useful supplement to conventional
medical treatment of rheumatoid arthritis.
Mediterranean Diet (MD):
Current knowledge suggests that healthier nutrition by adjusting
to a Mediterranean diet and a higher intake of fish is associated
with a reduction in inflammatory activity, an increase in physical
function, and improvement in RA patients’ vitality [68]. Even
more, supplementation withomega-3 polyunsaturated fatty acids
(omega-3 PUFAs) reduce patients’ morning stiffness, painful joints,
and NSAIDs consumption. It involves high consumption of olive
oil, cereals, fruits, vegetables, fish, and legumes; less red meat; and
inclusion of moderate amount of red wine in diet (Cretan MD).In a study by Matsumoto et al [69], it was found that intake of
monounsaturated fatty acids (MUFA) was significantly lower in RA
group and the ratio of consumed monounsaturated to saturated fatty
acid (MUFA/SFA) significantly differed within the RA group after
being sub-classified according to DAS28-ESR.Daily MUFA intake, a component of the Mediterranean diet score, was selected as an independent predictor of remission in the RA group and its intake
might suppress disease activity in RA patients.
On the other hand, few studies have not shown any significant
benefit with MD. Bloomfield et al [70], pointed out that while many
studies have confirmed a beneficial role of the Mediterranean diet in
preventing cardiovascular events, cancer and diabetes, no such role in
RA has been proven.
Elimination Diet:
Studies have shown that consumption of allergenic foods
increases pro-inflammatory cytokines that are considered a hallmark
of RA [71].An Elimination diet can identify triggers of arthritis pain
and can easily be instituted on an outpatient basis.It is usually started with a simple baseline diet, excluding foods
that are more common triggers (mentioned below) and including
only those foods not implicated in arthritis such as brown rice, cooked
or dried fruits, cooked green, yellow, and orange vegetables, plain or
carbonated water, condiments (modest amounts of salt, maple syrup,
vanilla extract).
After a few weeks of eating only baseline foods, other foods are
added back into the diet one by one and any new symptoms are
monitored during these days. If the added foods do not cause any
symptoms, those can be continued. A newly added food associated
with increased joint pain should be removed from the diet for 1-2
weeks, and then reintroduced to see if the same reaction occurs. This
methodical way of adding new foods back in makes it easy to identify
which foods cause inflammation and arthritis pain.
There are different types of elimination diets using different
methods. For example, certain elimination diets completely avoid all
meats including chicken, turkey, fish etc. while others include it.
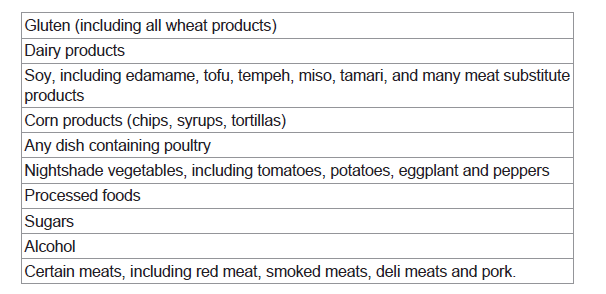
The most likely triggers found in various Elimination diets are:
Elemental Diet:
Elemental diet is an hypoallergenic protein-free artificial diet
consisting of essential amino acids, glucose, trace elements and
vitamins [72]. It is thought to provide complete nutrition and avoids
many of the side effects of other drugs used for pain relief in patients
with RA [73]. Studies have shown that an antigenic load within the
bowel lumen is an important factor in the pathogenesis of rheumatoid
arthritis [74], an elemental diet as the sole source of nutrition may be
an effective treatment. Elemental diet is given to patients with RA in
order to induce a remission and then foods are gradually introduced.
Where a food is suspected of causing symptoms, it is removed from
the diet.A study by Podas et al [75], has shown that an elemental diet for
2 weeks is as effective as a course of oral prednisolone 15 mg daily
in improving subjective clinical parameters. But this study failed to
show any significant improvement in swollen joint score.
Vegan and Vegetarian Diets:
A diet including intake of only fruits and vegetables, eliminating
any animal product or by-products is vegan diet. This has been
repeatedly reported to be clinically beneficial for disease remission in
RA patients [76-79].Researchers in Norway found that a vegan diet
led to reductions in pain, swelling, and morning stiffness, as well as
improvements in C-reactive protein [80] and these symptoms were
sustained for a long time with removal of meat products from the
diet. Another study found significant improvements in RA symptoms
with a 4-week vegan diet intervention [81].Some studies have found that higher intakes of meat [82-83] and
elevated serum cholesterol concentrations [84-85]are associated with
increased risk of developing this disease.
Inclusion and Exclusion of certain Dietary Factors:
There are single dietary factors which have been proven to
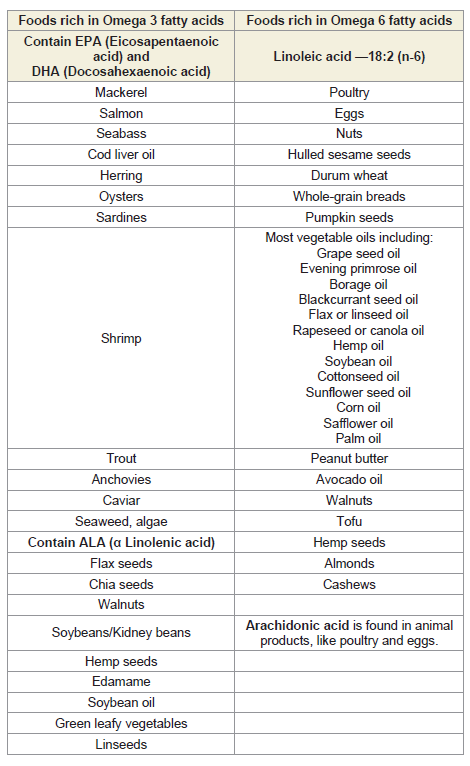
prevent RA.Role of Polyunsaturated fatty acids:
While n-6 PUFAs have a predominantly pro-inflammatory effect,
n-3 PUFAs seem to have anti-inflammatory action. Supplementation
with n-3 PUFAs (such as eicosapentaenoic acid and docosahexaeonic
acid) has been shown to change favourably the n-6/n-3 fatty acids
ratio, reduce inflammation, and alleviate pain, as well as lowering
disease activity in rheumatoid arthritis patients. Marine oil is thought
to have an analgesic effect in arthritis as a likely consequence of
its high content of docosahexaeonic acid (DHA; 22:6 n-3) and
eicosapentaenoic acid (EPA; 20:5 n-3) [86-87].Arachidonic acid (AA; 20:4 n-6), as well as DHA and EPA, are
used in the production of lipid mediators (e.g., eicosanoids), which are
involved (among other functions) in the regulation of inflammation.
However, the mediators produced from DHA and EPA shift the
balance toward resolution [88].
Another study has seen a beneficial effect when fish oils were
taken with primrose evening oil, containing γ-linolenic acid [89].
Other dietary factors with a beneficial role:
Pattison et al [90] confirmed that daily consumption of a glass
of freshly squeezed orange juice is inversely correlated with the risk
of RA, probably due to the protective action of beta-cryptoxanthin,
a natural carotenoid. Similar effect is shown with vegetables like
mushroom and spinach.Both low-sodium [91]and low-magnesium diets seem to have
some anti-inflammatory potential. Low-magnesium diet had
significant reduction in synovial gene expression of IL-6, RORA and
RORC, responsible for the development of Th17 cells [92] in rats and
might show similar results in humans.
Studies suggest that arthritis severity may be alleviated by a high
methionine diet [93].A significant reduction was found in serum
high-sensitive C-reactive protein (hs-CRP) and disease activity
(DAS-28) score in a study involving 40 female patients with a mild to
moderate severity of RA who were supplemented for 12 weeks daily
with a Selenplus capsule containing 50 μg of selenium, 8 mg of zinc,
400 μg of vitamin A, 125 mg of vitamin C, and 40 mg of vitamin E
[94].
Polyphenols and neochlorogenic acid found in dried plums
may inhibit TNF-induced formation of osteoclasts by lowering the
number of tart rate-resistant acid phosphatase (TRAP) positive
cells, responsible for osteoclastogenesis [95]. Similarly, equol, a
major soybean isoflavone metabolite, was found to both alleviate the
severity of arthritis symptoms and slow down the decline in bone
mineral density following collagen induced arthritis [96].
Curcumin has shown to decrease the expression of NF-κB, TNF-α,
and IL-1β in the synovial fluid and blood serum [97]. Studies have
shown that about 1000 mg/day of curcumin can help in alleviating
pain symptoms connected with arthritis [98].Comparable protective
effects against RA are seen with ginger [99].
Pomegranate extract and quercetin are not behind in the list of
products benefitting RA. A decrease in swollen and tender joints,
pain intensity and erythrocyte sedimentation rate (ESR) levels, with
reduction in DAS-28 and HAQ, as well as lower hsTNF-α levels were
seen with pomegranate and quercetin both [100-101].
Exercises in Rheumatoid Arthritis:
People with rheumatoid arthritis can largely benefit from exercise.
It helps in relieving pain and joint stiffness, improves joint function
and flexibility, increases range of motion, and boost mood. But it is
very difficult to stay motivated for exercise especially when patient is
in pain. The best exercises are:Stretching:
Stretching especially in the morning seems to be ideal for these
patients. Stretching should be preceded by warming up for 3-5
minutes by simply walking. One should hold each stretch for 10–20
seconds before releasing it and repeat each stretch 2–3 times. Using a
yoga strap may help maintain proper form while stretching.Walking:
Walking is a low-impact form of exercise that can help with heart
and joint health. It is often sensible to walk slowly initially and then
increase the pace when possible. Though it sounds too simple, but
walking is one of the easiest and most convenient forms of exercise.Tai chi and yoga:
Both tai chi and yoga combine deep breathing, flowing
movements, gentle poses, and meditation. They increase flexibility,
balance, and range of motion while also reducing stress.Tai chi
(sometimes called “moving meditation”) is a traditional Chinese
martial art that combines slow and gentle movements with mental
focus. This exercise improves muscle function and stiffness and
reduces pain and stress levels in patients with RA.Pilates:
Pilates is a low-impact activity that stabilizes the joints and
strengthens the muscles around them. Patients suffering from
rheumatoid arthritis should avoid using a machine for doing pilates.Water exercises:
According to the Centers for Disease Control and Prevention,
water-based exercise can help people with chronic diseases. For
people with arthritis, it improves use of affected joints without
worsening symptoms [102], as it supports body weight and do not
impact heavily on the joints. People with rheumatoid arthritis have
more health improvements after participating in hydrotherapy than
with other activities [103]. Water-based exercise also improves the
use of affected joints, decreases pain, increases flexibility, range of
motion, and strength from osteoarthritis [104].Swimming, water aerobics, and other gentle water exercises
can increase flexibility, range of motion, strength, and aerobic
conditioning. They can also reduce joint stress and stiffness.
Cycling:
Cycling is an excellent, low-impact exercise that’s easier on the
joints than other aerobic exercises. Riding a stationary bike can be a
safe way to get the joints moving and improve cardiovascular fitness.
It helps building leg strength and reduces morning stiffness.Strength training:
Strengthening the muscles around the affected joints, using a
resistance band, helps in reducing pain and other arthritis associated
symptoms.Hand exercises:
Bending the wrists up and down, slowly curling the fingers,
spreading the fingers wide on a table, and squeezing a stress ball can
help increase strength and flexibility in the hands.Gardening:
Gardening is a good way to alleviate mood. Gardening slowly
without overstraining the muscles and joints, serves both the purposes
of caring for the plants as well as the joints.Osteoarthritis:
Osteoarthritis (OA) is defined as a heterogeneous group of
conditions that lead to joint symptoms and signs associated with a
defective articular cartilage and related changes in bone morphology
[105].It can occur in almost any joint in the body. Although the
usual population associated with the condition is the elderly, who are
mostly inactive, athletes and younger individuals are also susceptible.Osteoarthritis is the most common joint disease and the fastest
growing form of disability worldwide [106], causing deterioration
of quality of life and reduced participation in social activities. OAis
characterised by cartilage loss, subchondralbone changes, synovial
inflammation and meniscus degeneration [107]. Treatment options
for symptomatic OA are fairly limited and often only provide
temporary relief.
Pathogenesis of the Disease:
Mechanical injury, hereditary factors and ageing can initiate the
pathophysiological processes that lead to OA.Originally; OA was
considered a non-inflammatory arthritis while only rheumatoid
arthritis was considered inflammatory in nature. The discovery that
many soluble mediators such as cytokines or prostaglandins can
increase the production of matrix metalloproteinases (MMPs) by
chondrocytes led to the first steps of an “inflammatory” theory [108].Joint swelling is one clinical feature of OA attributed to
inflammation and reflecting the presence of synovitis due to
thickening of the synovium or to effusion. Recent experimental
data have shown that subchondral bone may have a substantial role
in the OAprocess, as a mechanical damper, as well as a source of
inflammatory mediators implicated in the OApain process and in the
degradation of the deep layer of cartilage [109-111].
Why exactly the synovium becomes inflamed in OA remains
controversial [112]. Two theories have been proposed:
Theory 1 (Hypertrophic Repair Phase):
In this phase a loss in the glycosaminoglycan will lead to an
increase in water content resulting in softening of articular cartilage.
Further it leads to alteration in cartilage compressive resistance and
osmotic pressure within the tissue [113]. Anabolic activities and
production of collagen type II and proteoglycan are intensified.
Synovial cells consider fallen cartilage fragments, into the joint, as
foreign bodies, thereby producing inflammatory mediators. These
mediators can activatechondrocytes present in the superficial layer
of the cartilage, resulting in their increased proliferation and cluster
formation [114-115]. This leads to metalloproteinase synthesis
and, eventually, increase cartilage degradation. The mediators can
also induce synovial angiogenesis and increase the synthesis of
inflammatory cytokines and matrix metalloproteinases by synovial
cells themselves (vicious circle).Theory 2:
Collagen type II fragments from the damaged cartilage surface can induce inflammatory responses in the synovial membrane resulting
in hyperplasia, lymphocytic infiltration and perivascular lymphoid
aggregates [116]. There is an important role for synovial macrophages
in MMP-mediated cartilage damage. Therefore, more recently,
synovial tissue is involved as a primary trigger of the OA process
[117-119]. Synovial inflammation may drive synovial angiogenesis,
linked to OA pain, through macrophage activation [120-121].Further, it is seen that innate immunity may be a driver of the OA
process. Synovial fluid from patients with early OA cartilage damage
showed:
Increased fibroblast-like synoviocyte responses to TLR-2 and
TLR-4 ligands [122]
Increased levels of interleukin-15 (IL-15) protein
Abnormally high expression and activation of complement in
human OA joints [123]
Etiology of Osteoarthritis:
OA is usually thought to be a progressive disease of the adult and
elderly. However, there are several risk factors apart from age that
predispose an individual to OA, such as genetics, obesity, joint injury,
occupational or recreational activities, gender, and race [124].There
are strong associations of OA with obesity and joint injury.Osteoarthritis, commonly known as wear and tear arthritis, is
found in athletes and young individuals who use their joints more. The
effect of occupational and recreational activities on the development
of OA was evident in a study by Cameron et al [125], where active
duty military personnel were found to have significantly higher rates
of OA compared to the same age group in the general population.
There is ample evidence that anterior cruciate ligament (ACL)
rupture and meniscal tear are two major risks factors for developing
early OA [126]. Athletes are more likely to sustain joint injuries
compared with the average individual. As a result, there is increased
joint instability and altered joint mechanics, even with normal use
[127]. This further restricts mobility, induces pain and functional
impairment, making them “young patients with old knees”.
Joint degeneration occurs in athletes and young individuals
through damage to the articular cartilage caused by repetitive impact
and loading [128]. Sports that cause direct blunt trauma to joints
(such as football, soccer, hockey, lacrosse, and rugby) account for
the most impact damage.For contact stressors to cause disruption
to normal articular cartilage, a force of 25 MPa or more is required.
Activities such as running and jumping, which put mechanical stress
on joints, produce force <25 Mpa, and therefore, are less likely to
cause any disruption to the cartilage [129].
Smoking, physical inactivity, muscle weakness, leptin, vitamin D
deficiency and dietary fatty acid intake [130] also contribute to the
pathogenesis of the disease but their role is still controversial and not
very well defined, when considered individually.
Clinical Presentation and Diagnosis:
Pain is the main presenting symptom of OA but the diagnosis in
athletes and sportsperson might get delayed as pain is a part of their
everyday routine. Also with a high desire to return to play, athletes at times don’t disclose pain or hide the severity of their pain. Few have a high pain threshold and won’t complain until ailment gets worsened
[131-132].In the early phases of the disease, pain is related to activity and
becomes more constant over time, while in the late stages there is
‘background pain’ interspersed with unpredictable intense pain [133].
Morning stiffness of the joints is the second most prominent
symptom of OA. The stiffness usually involves joints of the fingers,
knees, hips, and spine. It usually resolves within an hour of waking up
[134]. Crackling or grating sensation, which occurs as a result of the
roughness of the surfaces in the joint are other symptoms.
The physical exam focuses on the range of motion (both passive
and active), muscle strength, ligament stability, and tenderness of the
affected joints [135], crepitus and effusion.
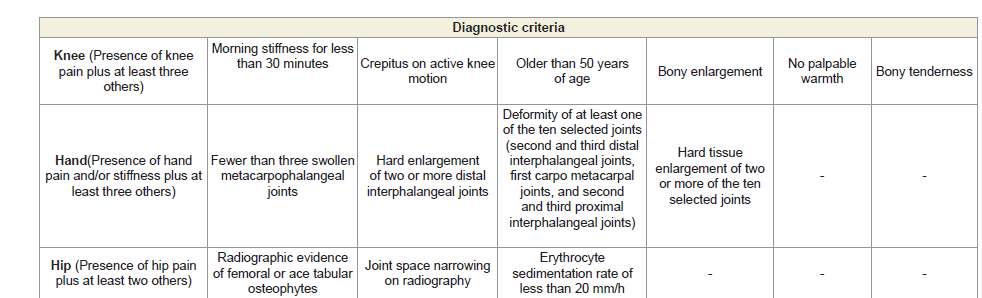
Diagnostic criteria for the OA of knee[136], hand [137]
andhip[138].
The diagnosis of the severity of OA is subjective: based on a quality
of life questionnaire, physical examination and radiography [135].
The most commonly used quality of life measure is Western Ontario
McMaster Index (WOMAC) although other similar measures such
as visual analog scale (VAS) for pain and Lequesne index are also
used [139-140].WOMAC Index was developed in 1982 at Western
Ontario and McMaster Universities. WOMAC is available in over 65
languages and has been linguistically validated [141-142].
The Western Ontario and McMaster Universities Arthritis
Index (WOMAC) is widely used in the evaluation of Hip and Knee
Osteoarthritis. It is a self-administered questionnaire which takes
approximately 12 minutes to complete, and can be taken on paper,
over the telephone or computer [143-144]. It consists of 24 items
divided into 3 subscales [142]:
Pain (5 items): during walking, using stairs, in bed, sitting or
lying, and standing upright
Stiffness (2 items):: after first waking and later in the day
Physical Function (17 items): using stairs, rising from sitting, standing, bending, walking, getting in / out of a car, shopping, putting
on / taking off socks, rising from bed, lying in bed, getting in / out
of bath, sitting, getting on / off toilet, heavy domestic duties, light
domestic duties.
The test questions are scored on a scale of 0-4, which correspond
to:
None (0),
Mild (1),
Moderate (2),
Severe (3), and
Extreme (4).
Plain radiography is usually the initial diagnostic image of choice,
although sensitivity is poor, especially in the early stages of OA
[145]. Radiographic features of OA include osteophytes, joint space
narrowing, subchondral sclerosis, and cysts.
Many a times the radiological defects are an incidental finding
whereas the person is asymptomatic, which often leads to a delay
in investigations and by then the pathological process is far
advanced[146-147].By the time the first knee joint changes are
detected by radiography, more than 10% of the cartilage is already
lost [148]. There are many joint tissues not visible by radiographs,
including the cartilage, synovium, meniscus, ligaments, capsule and
fat pad.
MRI is more sensitive for detecting early structural changes,
not only in the bone, but also in all joint tissues, detecting cartilage
defects, loss of cartilage volume, subchondral bone changes, bone
marrow lesions, synovitis and meniscal tears [149].
Ultrasonography can detect and evaluate both early and late
abnormalities in OA involving the hyaline cartilage, synovial
membrane, meniscus, joint capsule, bursa and bony cortex. As
compared to MRI, it is safe, less expensive and less time consuming.
On the other hand, operator-dependency and its inability to assess
deeper articular structures due to the acoustic shadowing makes it
less widely used [150].Ultrasound can detect synovial hypertrophy,
joint effusion and increased vascularity analysed by synovial power
Doppler, with a moderate to good intra-observer and inter observer
reliability [151].
Management:
To identify people at high risk of developing OA, it is important to
initiate early interventional treatment in patients with early structural
changes, even if they are asymptomatic [152].Exercise is one of the first and the most recommended tool in the
management of OA, which is followed since years [153-154]. Exercises
that increase strength, flexibility, and aerobic capacity are likely to
be the most effective in lower limb OA [155]. Muscle strengthening
exercises are extremely important especially for athletes because these
are very helpful in reducing pain.
In the pharmacological management, NSAIDs play a key role
in alleviating pain and inflammation and are beneficial in the initial
stages of OA. Gastrointestinal upset is a bitter part of NSAIDs,
therefore, the athletes with already existing GI problems should be
careful [156]. Relief from pain will help in improving the alignment
and biomechanical forces in the knee [157]. This is again important to
prevent any future musculoskeletal pathologies [158].
Intra articular injection with corticosteroids [159] and
viscosupplementation with hyaluronic acid [160] is another modality.
Steroids have anti-inflammatory properties and are beneficial for
short term relief. Caution should be observed, however, because of
the cytotoxicity of steroids to chondrocytes, with or without lidocaine
[161].
Hyaluronic acid has anti-inflammatory and analgesic effects,
in addition to its viscoelastic properties, making it valuable in the
treatment of OA [160].However, the combination of glucosamine
and chondroitin sulphate is the most promising. This treatment may
be efficacious for pain relief, functional improvement and also result
in less joint space narrowing [162-166].
As far as the surgical line of management is concerned,
arthroscopy is the first line of management. Radio graphically
invisible pathologies such as cartilage defects and meniscal tears
can be seen by arthroscopy [167]. Arthroscopy, with its tactile and
dynamic capabilities, permits palpation of the joint tissues with a
probe, and can easily detect softening, which is the earliest change in
the cartilage. One of most widely employed procedures for internal
derangement of the knee, the role of arthroscopy in osteoarthritis
is still controversial and unproven [168-169].It has very limited
role in knee OA and has the potential to even accelerate the disease
progression and/or patient’s pain.
Other surgical treatments that are considered before total
knee arthroplasty (TKA) include high tibial osteotomy (HTO) and
unicondylar or partial knee arthroplasty (UKA). Such surgeries
are infrequent in young population suffering from OA. These are
considered the last resorts in the treatment of OA and are usually
performed in elderly.
Dietary Modifications:
Thomas et al. performed a literature review of the relevance
of dietary interventions to OA management. This group found
six modifiable nutritional factors that may be implicated in OA:
adiposity/obesity, metabolic syndrome, type 2 diabetes, consumption
of long-chain n-3 fatty acids, blood cholesterol levels, and vitamin K
intake [170].Weight reduction: An initial aim of 10% body weight reduction
should be included in a first-line approach for obese patients with
OA. Overall aim for obese/overweight patients is for BMI within
the healthy range (18.5–25 kg/m2). This aim should not be achieved
by severely cutting down the calories. Rather it should be achieved
by moderate energy restriction without compromising nutrient
intake. Input from a dietician would be of immense help especially
when mobility is impaired and exercise is limited. Therefore, weight
reduction programmes that combine diet and exercise would show a
better outcome.
Exercise: The aim of exercise should be to reduce adipose tissue
without compromising the muscle mass [171-172]. Exercise schedule
should be tailored separately for each patient. Exercise should include
aspects of light aerobic exercise, strengthening and flexibility. Few
minutes of the exercise schedule should be dedicated to yoga and
breathing exercises for overall health of the body.
It appears that for OA patients, exercises involving supervised
slow movements or isometric exercises may be efficacious and also
have a lower possibility of damage to the joint than other exercises
[139,173-177]. Therefore, aquatic exercises, yoga and tai chi should
be preferred. Running on treadmills should be avoided.
Alteration in lipid intake:
Lipids are stored in the matrix and
chondrocytes of articular cartilage and may contribute towards
inflammation, cartilage degradation and impaired chondrocyte
structure [178].OA joints accumulate high levels of omega-6 (n-6)
fatty acids, precursors of pro-inflammatory eicosanoids [179]. On
the other hand, dietary intake of omega-3 (n-3) PUFAs generate anti
inflammatory mediators (resolvins) [180].Omega-3 fatty acids are a
vital component of the diet as they can minimize inflammation and
keep the body healthy. It should be borne in mind that the balance
of omega-3 and omega-6 in the body plays a role in preventing
inflammation. In addition to increasing omega-3 intake, consumption
of foods high in omega-6 should be limited. The Western diet has
a high ratio of n-6 to n-3 fatty acids, predisposing to inflammation
[181].Increasing long chain n-3 PUFA status to promote an antiinflammatory
effect is best achieved with direct EPA intake alongside
decreased LA intake.EPA and DHA are found primarily in oily fish
[182].Higher intakes of EPA/DHA, including the proposed antiinflammatory
threshold of >2.7 g/day [183], may be more easily
achieved by fish oil supplementation.
Cholesterol Intake:
High cholesterol levels are known to increase cytotoxicity [184]
in cells leading to higher formation of Arachidonic acid and resulting
in more of pro inflammatory mediators [185]. In a normal, healthy
joint, cholesterol accumulation does not take place due to the active
cholesterol efflux system. The latter gets dysregulated in OA as a
result of which, cholesterol gets hoarded in OA cartilage.Statins have shown promising results in reducing levels of
cholesterol. Statins help lower the clinical and radiographic progression
of the disease. They help in preventing cartilage degeneration to a
certain extent and in reduction of the pro inflammatory cytokines/
mediators in joints [186-188].
Studies have shown that dietary changes could result in a 35%
reduction in LDL-cholesterol, equivalent to that of a starting dose
of statins [189-190]. There are a number of foods that help lowering
cholesterol:
High-fibre foods (Oats):
Oatmeal contains soluble fibre, which reduces low-density
lipoprotein cholesterol by reducing its absorption in blood. Soluble
fibre is also found in such foods as kidney beans, Brussels sprouts,
apples and pears.
One serving of a breakfast cereal with oatmeal or oat bran
provides 3 to 4 grams of fibre [191]. Adding a banana or berries to it
will further enhance the fibre level.Omega-3 fatty acids (Fatty fish):
Fatty fish has high levels of omega-3 fatty acids, which can reduce
triglycerides in the blood. LDL cholesterol levels are not much
affected by omega-3 fatty acids. Eating at least two servings of fish
a week, preferably by baking or grilling, gives much health benefits.Almonds and other nuts:
Almonds, walnuts and other tree nuts can improve blood
cholesterol. A recent study concluded that a diet supplemented with
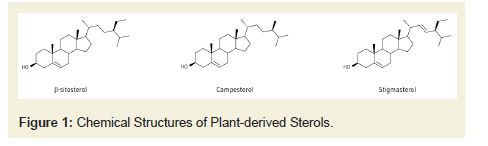
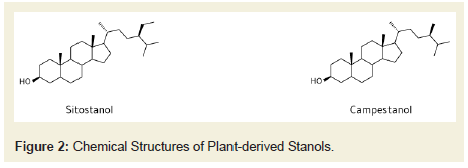
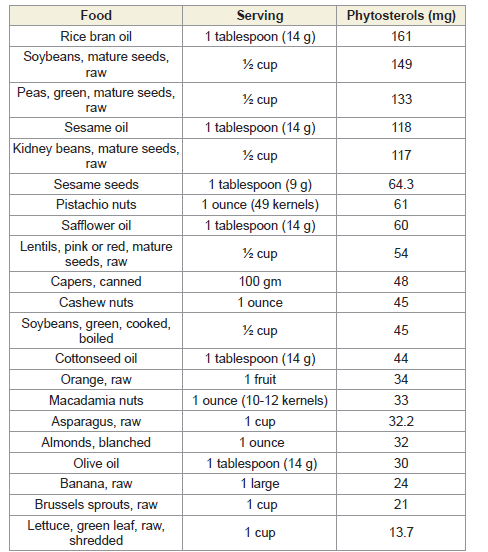
walnuts can lower the risk of heart complications in people with history of a heart attack. All nuts are high in calories, so a handful added to a salad or eaten as a snack will do.Plant Stenols/Sterols:
Plant sterols (PSter) [Figure 1] and stanols (PStan) [Figure 2], together known as phytosterols (PSS), are cholesterol-like
compounds that occur naturally in plant-based foods. Phytosterols
interfere with the intestinal absorption of dietary cholesterol by
displacing cholesterol from micelles; they also facilitate the excretion
of biliary cholesterol in the feces.The LDL-cholesterol lowering effect
of phytosterols is summarized in several meta-analyses showing a
dose-response relationship with intakes of 1.5 to 3 g/day lowering
LDL-C by 7.5% to 12% [192-196].PSS are efficacious in all foods and food supplements; for optimal
efficacy they should be consumed with a (main) meal and twice
daily [197].PSS are effective in both healthy and diseased individuals
suffering from familial hypercholesterolemia, type-2 diabetes mellitus
or Metabolic Syndrome.
Phytosterol Content of FoodsAvocados:
Avocados are a potent source of nutrients as well as
monounsaturated fatty acids (MUFAs). Research suggests that
adding an avocado a day can help improve LDL cholesterol levels in
people who are overweight or obese.Olive oil:
In order to lower cholesterol, olive oil should be used in place
of other fats in the diet. It can be used in a variety of ways, sautéing
vegetables, adding it to a marinade or mixing with vinegar as a salad
dressing. Olive oil can be used as a substitute for butter when basting
meat or as a dip for bread.Foods with added plant sterols or stanols:
Margarines and orange juice with added plant sterols can help
reduce LDL cholesterol. Plant sterols or stanols do not affect levels of
triglycerides or of high-density lipoprotein (HDL) cholesterol.Whey protein:
Whey protein, which is found in dairy products, may account for
many of the health benefits attributed to dairy. Studies have shown
that whey protein given as a supplement lowers both LDL and total
cholesterol as well as blood pressure.Other changes in diet:
Getting the full benefit of these foods requires other changes to
diet and lifestyle. One of the most beneficial changes is limiting the
intake of saturated and trans fats.Saturated fats, such as those in meat, butter, cheese and other fullfat
dairy products, raise total cholesterol. Decreasing the consumption
of saturated fats to less than 7 percent of total daily calorie intake can
reduce LDL cholesterol by 8 to 10 percent.
Trans fats, sometimes listed on food labels as "partially
hydrogenated vegetable oil," are often used in margarines and storebought
cookies, crackers and cakes. Trans fats raise overall cholesterol
levels. The Food and Drug Administration has banned the use of
partially hydrogenated vegetable oils by Jan. 1, 2021.
Role of Antioxidants:
A plausible rationale exists for a role of antioxidants in OA.
Reactive oxygen species and reactive nitrogen species may be involved
in the pathophysiology of OA, and therefore, suppressing these with
antioxidants might delay its onset and progression [198-199].A free radical is a molecule with an unpaired electron in its
outermost orbit [200-201]. In biological systems, a free radical that
involves oxygen is termed a reactive oxygen species (ROS) but the
term ROS is used loosely for oxidants such as peroxides. Normal
physiological processes result in the generation of ROS such as
peroxide, superoxide, hydroxyl radical and peroxynitrite. Thus, ROS
occur normally in the body at very low concentrations (nanomolar to
micromolar). They are a necessary evil since our body needs them for
survival but, when in excess, they may have deleterious effects. Our
body gets rid of the excess ROS using natural antioxidants such as
vitamin C (ascorbate), vitamin E, glutathione and various enzymes
[200-202]. The term oxidative stress is used as a measure of the overall
ROS status. It is the ratio of the amount of peroxide present to that
of the antioxidant capacity of the cell. High levels of oxidative stress
may damage the cells by oxidising lipids and by altering DNA and
protein structure.
The antioxidant vitamins, A, C and E have received the most
attention in this context with vitamin C being particularly relevant
owing to its requirement for collagen formation [203].Several studies
have talked about the use of antioxidant supplements derived from
curcumin, avocado, Boswellia and other herbs [204].
Curcumin:
Curcumin, a compound with antioxidant properties, was
isolated from turmeric about 200 years ago [205]. Curcumin,
(diferuloylmethane; 1, 7-bis [4-hydroxy-3- methoxyphenyl]-1,6-
heptadiene-3,5-dione) along with its mono and di demethoxy
derivatives, collectively called curcuminoids, constitute the major
colouring matter and the biologically active constituents of Curcuma
longa L. or turmeric. Ayurveda, Unani, Siddha and Chinese
medicines recommend turmeric for a wide range of disorders and
diseases. Modern science has provided a scientific basis for such uses
[206-212].The properties of curcumin and its potential role in the therapy
of several chronic diseases including arthritis, cancer and neuronal
disorders have been explored. Curcumin may be efficacious for pain
relief and function retention in OA patients. Presently, some of the
strongest evidence for the therapeutic efficacy of curcumin (confirmed
by meta-analytic analyses of randomized controlled trials) is for
the treatment of arthritis, pain and analgesia, and major depressive
disorder. In a meta-analysis by Daily et al [98], the systematic
review provided scientific evidence that 8–12 weeks of standardized
turmeric extracts (typically 1000 mg/day of curcumin) treatment can
reduce arthritis symptoms (mainly pain and inflammation-related
symptoms) and result in similar improvements of the symptoms as
ibuprofen and diclofenac sodium. In another meta-analysis [213],
eight RCTs were included and curcuminoids was found to be safe and
well tolerated by participants. They were found to significantly reduce
pain and the effect was found to be independent of administered dose
and duration of treatment with curcuminoids.
But curcumin absorption has been reported to be extremely
poor when it is used alone [214-217]. Poor absorption from the gut
and avid metabolism in the body is cited as reasons for the lack of
systemic availability. While the major portion of ingested curcumin
is excreted through the feces unmetabolized, as determined in
several animal studies [218], the small portion that is absorbed is
extensively converted to its water-soluble metabolites, glucuronides
and sulphate, which are then excreted. This seriously limits curcumin
to reach targets distant from the gut and exert its beneficial action.
To overcome this problem, numerous methods have been
undertaken to increase its bioavailability.These include the use
of adjuvants such as piperine, formulating liposomal curcumin,
curcumin nanoparticles, curcumin phospholipid complexes, and
the use of structural analogs of curcumin such as turmeric oil [219-220]. These efforts have shown some success with an increased blood
concentration of curcumin. The study by Shobha et al determined the
effect of piperine (inhibits hepatic and intestinal glucuronidation)
on the bioavailability of curcumin [217]. A co-administration of
curcumin with 20 mg piperine increased its’ bioavailability by 20-
fold.Curcumin has also been reconstituted with non-curcuminoid
components of turmeric into a proprietary preparation termed
BCM-95CG or Biocurcumax [221]. Biocurcumax increased the
oral bioavailability of curcumin when compared to curcumin alone
or curcumin plus lecithin. However, there are no reports using this
preparation for OA.
One trial used the combination of roots of Withania somnifera,
the stem of Boswellia serrata and rhizomes of Curcuma longa and a
zinc complex. There was a significant improvement in pain relief and
function [222]. Ainat - a preparation containing devil’s claw, turmeric
and bromelain also showed a clinically relevant improvement in acute
and chronic pain [223].
Avocado/Soybean Unsaponifiable (ASU):
The unsaponifiable fraction from avocado/soybean oils is
termed avocado/soybean unsaponifiable. ASU has been tested in
the management of OA. ASU contains phytosterols, β-sitosterol,
campesterol, and stigmasterol, fat soluble vitamins, triterpene fatty
acids and possibly furan fatty acids, but the identity of the active
components in it is unknown [224]. Literature provides conflicting
results, with few studies showing very good results and a few
considering soybean protein alone for benefits in OA.Boswellia:
Resins from trees of Boswellia serrata, and other species of this
genus, have been used for arthritis and other diseases in Ayurvedic
medicine since ancient times. One of the compounds present in
Boswellia, acetyl-keto-beta-boswellic acid (AKBA), is an inhibitor of
the lipoxygenase pathway and is suggested to have anti-inflammatory
properties [225]. Almost all studies have shown some or the other
benefit in OA.Ayurvedic Preparations:
Withania somniferum (ashwagandha) [226], Tinospora cordifolia
(Guduchi) [227], Emblica officinalis (or Phyllanthus emblica/amla)
and emblicanins A and B [228], Zingiber officinale (Ginger) root are
among the other divine herbs used in OA.Vitamin D and Osteoarthritis:
Vitamin D insufficiency is a global nutrition challenge. Once
thought to cause solely rickets and decreased bone density, vitamin
D deficiency has been associated with several chronic diseases such
as multiple sclerosis, type I diabetes, and hypertension [229]. Vitamin
D can be obtained through foods such as fatty fish, mushrooms, and
vitamin D-fortified products, and through cutaneous synthesis in
response to ultraviolet-B exposure. There are plenty of supplements
available in the market with different strengths.The classic role of vitamin D is known to increase calcium
absorption through the endocrine pathway. In order for a patient
to have adequate and efficient blood calcium levels, both vitamin
D and parathyroid hormone must be present at sufficient levels and function together [230]. When the levels of blood calcium are
low, the parathyroid gland releases parathyroid hormone, causing
expression of proteins that leads to an increase in total body calcium
levels. In the kidney, parathyroid hormone induces the conversion of
25-hydroxyvitamin D to 1, 25 dihydroxyvitamin D, which ultimately
results in an increase in the transcription of genes responsible
for calcium absorption [231]. When the parathyroid hormone is
removed, vitamin D cannot function properly within the patient,
resulting in hypocalcaemia.
However, as more precise methods for calcium absorption
measurement have been developed over recent decades, the effect
of vitamin D on Ca absorption in adults seems minimal, especially
in adults with 25(OH)D levels ≥ 20 nmol/L [232-235] and does not
increase calcium absorption in adolescents [236-237]. However,
vitamin D supplementation in those with 25(OH) D<50 nmol/L
appears to increase bone mass or prevent bone loss in adults [238-
239] and positively affect bone mineral augmentation in adolescents
[240-241]. Therefore, it is proposed that vitamin D may benefit bone
through an autocrine and/or paracrine pathway, especially since
circulating 1, 25(OH) 2D, the active vitamin D metabolite, is not
associated with 25(OH) D status. Though the mechanism by which
vitamin D affects bone is unclear, serum 25(OH) D ≥50 nmol/L is
required for optimal bone health.
Vitamin D is thought to reduce inflammation via its effect on T
and B lymphocytes, macrophages and dendritic cells [242]. Binding
of vitamin D to its receptors in immune cells leads to its activation.
This blocks the cellular response to TNF-α and IL-1 and allows for the
up regulation of IL-10.
The efficacy of vitamin D in treating or preventing OA is
controversial. Some authors have found that vitamin D deficiency
increases the risk of patients’ developing OA [243-245].Bassiouni et
al [246] and Veronese et al [247] both found that serum 25(OH)D
levels were significantly decreased in the patients with knee OA and
noted that medial meniscal deterioration was seen in patients with
low vitamin D levels.
Malas et al [248] found that vitamin D deficiency significantly
decreased femoral cartilage thickness in women between 20 and 45
years of age, which was determined by ultrasound.
On the other hand, there were reports which showed no
improvement [249-251] with vitamin D supplementation.
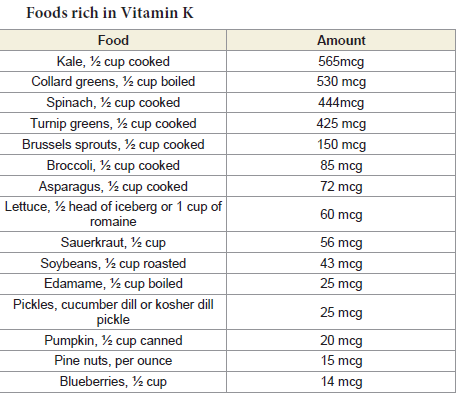
Role of Vitamin K:
Vitamin K is a group of fat-soluble compounds, with two
naturally occurring forms, vitamin K1 (phylloquinones) and vitamin
K2 (menaquinones) [252]. Vitamin K1, synthesized by plants and
algae, is the form most widely found in the human diet, mainly in
green leafy vegetables and oils [253]. Vitamin K2 is predominantly
produced by bacteria [254]. The adequate daily intake of vitamin K
for adults aged 19 years and older is 120 micrograms (mcg) for men
and 90 mcg for women.The main function of vitamin K is as an enzymatic cofactor for
the gamma (γ)-carboxylation of certain calcium-binding proteins,
including matrix gla protein (MGP), a vitamin K-dependent (VKD)
mineralization inhibitor, expressed in human articular cartilage
[255], periostin, gla-rich protein, gas 6 and osteocalcin.
Once carboxylated, MGP inhibits ectopic mineralization by
binding calcium crystals, thereby inhibiting calcium crystal growth,
and by binding to and inhibiting bone morphogenic protein-2,
a protein that induces bone formation [256-258]. In human OA
cartilage, MGP is primarily uncarboxylated, (the less functional
form), whereas in healthy articular cartilage MGP is primarily
carboxylated (functional) [259], suggesting the carboxylation of
MGP is relevant to OA. MGP is also detectable in circulation and
desphospho-ucMGP [(dp)ucMGP] concentrations increase when
vitamin K status is low [260], suggesting circulating (dp)ucMGP may
serve as a functional biomarker of vitamin K status for tissues that
use MGP.Hence, vitamin K is an important regulator of bone and
cartilage mineralization.
Genetic deficiencies of MGP in humans and mice have been linked
to skeletal abnormalities, including premature epiphyseal calcification
and shortening of long limb bones, reflecting endochondral bone
formation [261-264].
A study by Neogi et al [265], suggested that persons with higher
vitamin K levels, as measured by plasma phylloquinone, have a
significantly lower risk of large osteophytes than do persons with low
vitamin K levels, and this finding adds to the understanding of the
pathogenesis of osteophytes.
References
47. Alamanos Y, Drosos AA (2005) Epidemiology of adult rheumatoid arthritis. Autoimmun Rev 4: 130-136.
83. Grant WB (2000) The role of meat in the expression of rheumatoid arthritis. Br J Nutr. 84: 589-595.
108. Berenbaum F (2013) Osteoarthritis as an inflammatory disease. Osteoarthritis and Cartilage 21:16-21.
209. Sharma RA, Gescher AJ, Steward WP (2005) Curcumin: The story so far. Eur J Cancer 41: 1955-1968.