Journal of Pediatrics & Child Care
Download PDF
Case Report
Point of Care Ultrasound (Pocus) in Early Diagnosis of a Pediatric Pauci-Symptomatic Acute Heart Transplant Rejection
Delmonaco AG1, Garrone E1*, Raffaldi I1, Lauria B1,Aidala E2, Bordese R2 and Bondone C1
1Department of Pediatric Emergency, Regina Margherita Children’s
Hospital, University Hospital of Health and Sci-ence, Italy
2Department of Cardiology and Cardiac Surgery, Regina
Margherita Children’s Hospital, Italy
*Address for Correspondence: Emanuela G, Department of Pediatric Emergency, Regina
Margherita Children’s Hospital, University Hospital of Health and Science, Piazza Polonia 94, 10126,Turin, Italy;
Fax: 39 11 3135060, Email: garrone.emanuela@gmail.com
Submission: 20 September, 2021
Accepted: 12 November, 2021;
Published: 15 November, 2021
Copyright: © 2021 Delmonaco AG, et al. This is an open access article distributed under the Creative Commons AttributionLicense, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
We report the case of a 30-month-old boy affected by
severe cardiac failure in dilated cardiomyopathy requiring heart
transplantation (HT), who was referred to our Emergency Department
with a lightly symptomatic acute cardiac rejec-tion, suspected by
point of care clinical ultrasound, performed by the Pediatrician.
Despite the improvement in medical therapy and the development
in mechanical circulatory support, HT still remains the best therapeutic
option to im-prove survival and quality of life in patients with advanced
heart failure. Rejection remains an important reason for death after
pediatric HT and it can be unrecognized until more severe, because
of a specific signs at presentation. Point of care ultrasound (POCUS)
enhances the clinician’s ability to early recognize many pathologic
patterns allowing a timely and targeted treatment, as we describe in
this case report report.
Abbreviations
HT: Heart Transplantation; POCUS: Point Of Care Ultrasound;
FoCUS: Focused Cardiac Ultrasound; LUS: Lung Ultrasound;
IVC: Inferior Vena Cava; PED: Pediatric Emergency Department;
COVID-19: SARS-CoV-2; DSA: Donor Specific Antibodies; AMR:
Antibody-Mediated Rejection; AHF: Acute Heart Failure; CAV:
Cardiac Allograft Vasculopathy
Case Presentation
We report the case of a child with dilated cardiomyopathy which
evolved in severe cardiac failure requiring heart transplantation
(HT), performed when he was 11 month-old. He was then regularly
followed-up by the Cardiology and Cardiac Surgery Department of
Regina Margherita Pediatric Hospital of Turin. Once discharged
home, the patient was treated with a maintenance therapy with
tacrolimus and mycophenolate mofetil. No signs of rejection were
observed during clinical follow-up and Cath-Lab evaluations.
At the age of 30-month, during COVID 19 pandemic national
lockdown, the patient arrived at our Pediatric Emergency Department
(PED) for mild abdominal pain from3 days, a single vomit and
asthenia during the previous week. Regular therpeutic compliance
was reported. On physical examination the child showed a quite
good general condition, smiling, vital signs appropriated for age. No
oedemas nor cutaneous rash were detectable. A small mouth ulcer
was found. No significant findings on neurologic, cardiovascular and
pulmonary examination. Liver dropped 3 cm below the costal margin.
The oropharyngeal swab proved negative for COVID-19 infection.
His laboratory tests showed elevated N-terminal-pro B-type natriuretic peptide (NT-pro-BNP: 16109 pg/mL - normal value ≤92 pg/
mL); prothrombin time was 27.6 seconds; transaminase, bilirubin,
creatinine, sodium and potassium levels proved normal. Tacrolimus
level resulted within the therapeutic range. The abdominal ultrasound
carried out in the Radiology Unit detected a mild perisplenic and
perihepatic effusion. POCUS performed in the PED by the pediatrician
confirmed these abdominal findings and detected a 2 cm bilateral
pleural effusion, a 5 mm circumferential pericardial effusion, a mild
cardiac sectal hypokinesis and a non-collapsible inferior vena cava
(IVC). The echocardiography performed by a pediatric cardiologist
confirmed mild heart failure and pericardial effusion. The patient
was admitted to the Cardiology unit. Clinical acute heart rejection
was diagnosed and the endomyocardial biopsy was delayed, due to
child’s low weight. Donor specific antibodies (DSA) were detected
against HLA Class II DQ6 and DQ7, suggesting a humoral rejection.
Intravenous Methylprednilosone and Immunoglobulin therapy was
started and tacrolimus dosage was increased, leading to heart failure
regression and absorption of pericardial, pleural and abdominal
effusions. The child was discharged after 10 days, in good general
condition and asymptomatic. The endomyocardial biopsy performed
three weeks after discharge was negative for cellular rejection; C4d
immunostaining was negative and DSA titer was decreasing.
Technique:
POCUS was performed in the PED by the emergency pediatrician
using a ESAOTE ultrasound system; cardiac evaluation was obtained
with a FoCUS approach. The echocardiography done by the
cardiologist was performed using a PHILIPS ultrasound system. A
linear probe was used to detect pleural effusion, and a sector probe to
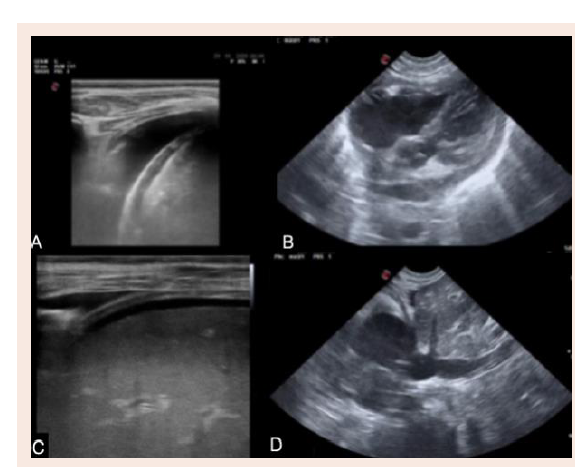
perform FoCUS and echocardiography (Figure 1).Review of Literature and Discussion
HT is a standard treatment for selected pediatric patients with end-stage heart disease. With improvement in surgical techniques
and immunosuppressive drugs, survival following transplantation
has increased over time [2]
. Nevertheless, HT recipients are exposed
to the risk of several potential complications that may impair their
outcome, including graft failure, rejection, infection and CAV (Cardiac
Allograft Vasculopathy) [1]. Although acute allograft rejection
remains an important potential cause of mortality and morbidity
after HT, its incidence and impact on graft survival decreased
over the years as immunosuppressive regimens have improved. Its
diagnosis is a combination of clinical assessment, echocardiographic
findings and endomyocardial biopsy [1-3]. Current knowledge
schematically recognizes two mechanisms leading to graft injury
during acute rejection: cellular-mediated and antibody-mediated
rejection [1-3]. Antibody-mediated rejection (AMR) is characterized
by a graft injury mediated by circulating antibodies against antigens
expressed by endothelial cells. The injury may depend upon
complement activation but can also be mediated by inflammatory
pathways activated within the endothelial cells or mediated by
natural killer cells [1,4]. Treatment depends on severity and includes
immunosuppression adjustment, pulsed corticosteroids, intravenous
immunoglobulins, plasmapheresis, immunoadsorption [1,5]. Acute
heart failure (AHF) in HT acute rejection is a diagnostic challenge
due to non-specific clinical manifestation and the urgent need for
timely and tailored management. Many co-existing or alternative
conditions with different pathophysiology can induce similar
clinical picture, making the differential diagnosis challenging [6].
Imaging modalities are pivotal for fast triage and accurate diagnosis
and for decision-making: several portable and stationary imaging
modalities are being increasingly used for the evaluation of cardiac
structure and function and haemodynamic and volume status. The
point-of-care focused cardiac (FoCUS) and lung ultrasound (LUS)
examinations are invaluable tools for rapid differential diagnosis. A
full echocardiographic examination is necessary for identification
of heart failure aetiology, severity, indications for specific therapy,
and risk stratification during the stabilization phase [6-8]. FoCUS
represents a rapid problem-oriented point-of-care protocol for the ED. FoCUS is possible to carry out with portable or handheld
devices as an adjunct to physical examination. The FoCUS approach,
providing a limited number of evidence-based targets [6], requires
less training and expertise than full echocardiographic exam. In the
early phase of AHF, FoCUS examination is useful to detect structural
and functional abnormalities of ventricles and valves and presence of
effusions [6]. In a case of haemodynamic instability, FoCUS is needed
to identify cardiac causes and it allows to quickly differentiate the
type of shock [6-9]. The integration of FoCUS and LUS into acute
care at an early stage revolutionizes the urgent workup providing
a prompt correct diagnosis, leading to faster clinical decisions and
immediate life-saving therapy [6]. At the arrival our patient did not
appear critical nor manifested signs of shock or evident heart failure.
The prompt application of POCUS allowed to formulate the correct
diagnosis and consequently timely target therapy.
Conclusion
Pediatric HT is standard of care for children with end-stage
heart failure. Though acute rejection has decreased progressively,
both diagnosis and management of antibody-mediated rejection is
still challenging and complex [8]. The diagnostic yield of POCUS,
providing the shortest path to life-saving therapies during first hours
after admission, is emerging. Comprehensive echocardiography has
the central role in the assessment of HF type and aetiology, indications
for treatment, and risk stratification [6]. The diagnosis of acute
rejection may be difficult due to the specific clinical presentation,
especially in early stages, as we observed in our patient. A high
index of suspicion by Pediatricians and the use of POCUS permit
its early recognition and consequently timely targeted therapies. The
POCUS evaluation could be not specific in recognizing an early acute
rejection after heart transplantation, due to the low specificity of the
ultrasound findings at an early stage of disease. Large, multicenter
trials are necessary in order to validate POCUS role in the diagnostic
assessment in the ED of patients with a suspicion for a acute rejection
after heart transplantation.