Journal of Pediatrics & Child Care
Download PDF
Research Article
The Impact of Preoperative Chlorhexidine Baths on Outcomes in Pediatric Patients Undergoing Adnexal Surgery
Motta M1*, Avila A1, Valdes J2,Samuels S3 and Levene T4
1Department of Surgery, Memorial Healthcare System, FL, USA
2Florida International University, Herbert Wertheim College of Medicine, USA
3Office of Human Research, Memorial Healthcare System, USA
4Pediatric Surgery, Joe DiMaggio Children’s Hospital, Hollywood, FL, USA
2Florida International University, Herbert Wertheim College of Medicine, USA
3Office of Human Research, Memorial Healthcare System, USA
4Pediatric Surgery, Joe DiMaggio Children’s Hospital, Hollywood, FL, USA
*Address for Correspondence:Monique Motta, Department of Pediatric Surgery, Joe DiMaggio Children’s Hospital, Hollywood, FL E-mail Id: mmotta@mhs.net
Submission:17 May, 2024
Accepted:13 September, 2024
Published:16 September, 2024
Copyright: ©2024 Motta M, et al. This is an open access article distributed under the Creative Commons Attr-ibution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Objective:Surgical site infections (SSIs) increase the risk of
morbidity, mortality, and health care costs. Pre-operative bathing
protocols with agents such as chlorhexidine 4% (CHG) have been
implemented however the efficacy of this practice in adnexal surgery
among pediatric patients is unknown.
Methods:We conducted a retrospective chart review of 115 nonneonatal, pediatric patients who underwent adnexal surgery from November 2017 to November 2022. Rates of SSIs, returns to emergency room (ER) and readmissions were compared for patients who did or did not receive a pre-operative antiseptic bath using CHG. Statistical analysis was conducted with statistical significance at p<0.05.
Results:The mean age at time of surgery was 13.3 years (range 0.75-20 years) with patients undergoing detorsion of adnexal structures and/or resection of adnexal masses or cysts. Over one quarter of our study population (26.1%) received a pre-operative bath with CHG. All patients underwent preparation of skin in the operating room just prior to incision with CHG and isopropyl alcohol skin preparation solution. Overall, the rate of SSIs was 1.8% (n=2) and there were no ER visits or readmissions due to SSIs. There was no significant difference in outcomes between pediatric patients undergoing pre-operative CHG bath with those not undergoing CHG bath prior to adnexal surgery.
Conclusion:Our data suggest that pre-operative bathing with CHG does not alter the rates of SSIs, ER visits or readmission rates for pediatric patients undergoing adnexal surgery. A larger multicenter prospective study would be required to determine a study sufficiently powered to make clinical recommendations.
Methods:We conducted a retrospective chart review of 115 nonneonatal, pediatric patients who underwent adnexal surgery from November 2017 to November 2022. Rates of SSIs, returns to emergency room (ER) and readmissions were compared for patients who did or did not receive a pre-operative antiseptic bath using CHG. Statistical analysis was conducted with statistical significance at p<0.05.
Results:The mean age at time of surgery was 13.3 years (range 0.75-20 years) with patients undergoing detorsion of adnexal structures and/or resection of adnexal masses or cysts. Over one quarter of our study population (26.1%) received a pre-operative bath with CHG. All patients underwent preparation of skin in the operating room just prior to incision with CHG and isopropyl alcohol skin preparation solution. Overall, the rate of SSIs was 1.8% (n=2) and there were no ER visits or readmissions due to SSIs. There was no significant difference in outcomes between pediatric patients undergoing pre-operative CHG bath with those not undergoing CHG bath prior to adnexal surgery.
Conclusion:Our data suggest that pre-operative bathing with CHG does not alter the rates of SSIs, ER visits or readmission rates for pediatric patients undergoing adnexal surgery. A larger multicenter prospective study would be required to determine a study sufficiently powered to make clinical recommendations.
Introduction
Surgical site infections (SSIs) represent a significant public health
concern due to their association with an elevated risk of morbidity
and mortality. Patients who develop SSIs often incur heightened
healthcare expenditures attributed to prolonged hospitalization,
emergency department visits, readmissions, and increased outpatient
care utilization. In elective surgical contexts, the incidence of SSI
ranges from 4.4% to 8.7%.[1] To alleviate the burden of SSI within
our patient population, the standardization of perioperative care is
imperative within the healthcare system.[2]The implementation of
evidence-based practices for perioperative care standardization has
the potential to enhance patient outcomes, particularly in terms of
reducing surgical site infection rates.[3,4] Preoperative protocols
encompass various elements, including umbilical cleansing and
administration of antibiotics within one hour of incision.[3]
Preoperative bathing with an antiseptic agent, such as 4%
chlorhexidine (CHG), is common practice in many institutions due
to its bacteriostatic and bactericidal properties.[5,6] While some
data supports preoperative bathing for specific surgical cases (e.g.,
orthopedic surgery, spine surgery, neurosurgery, colorectal surgery,
and vascular surgery), its efficacy remains inconclusive for adnexal
procedures involving benign conditions in the pediatric population.
[7-10]
Despite the existing literature gap concerning the effectiveness
of preoperative antiseptic cleansing with chlorhexidine for
adnexal procedures related to benign etiologies, our institution
has introduced a protocol mandating preoperative antibacterial
cleansing using CHG for inpatients aged over 2 months or weighing
more than 10 kilograms (kg), regardless of the surgical procedure,
including adnexal procedures. However, this policy does not
extend to outpatients undergoing similar surgeries from home or to
patients arriving for surgery directly from the emergency room or
referring hospital. The utility of preoperative CHG in the pediatric
population is poorly defined within elective settings, and current
recommendations lack specificity for this patient group. If a reduction
in SSI rates is observed among patients undergoing preoperative
antiseptic cleansing with chlorhexidine before adnexal procedures,
the establishment of a universal, standardized policy applicable to all
patients, whether inpatients or outpatients, could yield substantial
benefits for both patients and the healthcare facility. Our study aims to
assess the efficacy of preoperative CHG bathing in pediatric patients
undergoing adnexal procedures for benign etiologies by comparing
SSI rates between those who underwent preoperative CHG baths and
those who did not.
Methods
All inpatients aged ≥ 2 months or weighing more than 10 kg,
who are undergoing any surgical procedure at our institution,
including adnexal procedures, are required to undergo pre-operative
antibacterial cleansing using CHG 4%. However, patients who are
directly admitted to the operating room (e.g., those coming from
home, the emergency room, or a referring hospital) do not undergo
pre-operative antibacterial cleansing. The aim of this retrospective
chart review study was to evaluate the effectiveness of pre-operative
CHG baths in the context of adnexal procedures for benign etiologies
(e.g., cysts, non-malignant masses, and torsions) by comparing SSI
rates between patients who received preoperative antiseptic cleansing
and those who did not.
Charts of pediatric patients who underwent adnexal procedures
for benign conditions, performed by a pediatric surgeon at our
institution from November 2017 to November 2022, were collected.
Descriptive statistics were computed for demographic and outcome
variables. Categorical variables were assessed using Pearson’s chisquare
test or Fisher’s exact test, while quantile regression was
employed to compare the medians of continuous variables between
the two groups. Categorical data results are presented as counts and
proportions, and continuous variables are presented as medians
and interquartile ranges (IQR). Results were considered statistically
significant when P < 0.05. All analyses were carried out using Stata/
SE 15.1
Results
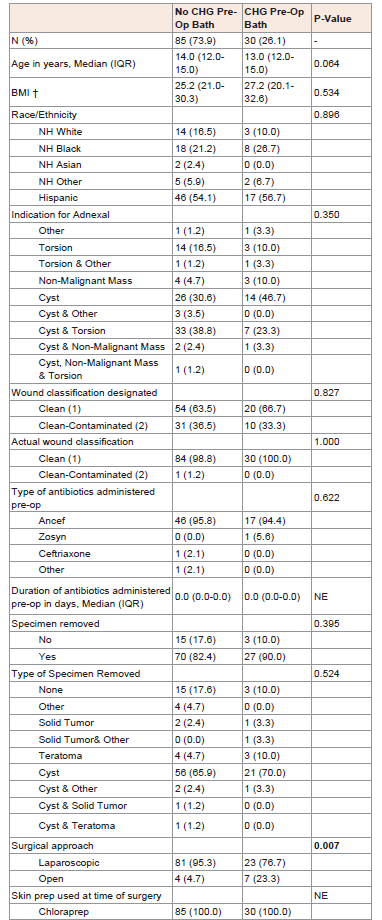
Among them, approximately 26% (n=30) underwent preoperative
antiseptic cleansing, while 74% (n=85) did not receive such cleansing
prior to their surgery [Table 1]. In both cohorts, the predominant
ethnic background was Hispanic. Although no statistically significant
differences were observed, the most prevalent indication for adnexal
procedures among those who did not undergo CHG preoperative
bathing was cysts and torsion (38.8%), while having a cyst without
other indications was the most common indication among those who
received CHG preoperative bathing (46.7%).
A majority of patients in both groups had a specimen removed
(No CHG: 82.4% vs. CHG: 90.0%), and while differences in the rate of
specimen removal and the type of specimens removed did not reach
statistical significance, cysts were the most frequently removed type
of specimen in both cohorts.
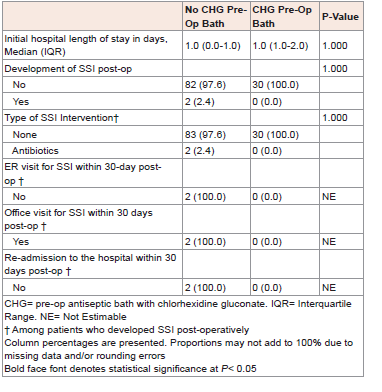
In our study population, the overall SSI rate was 1.8% as
presented in [Table S1]. Upon evaluating patient outcomes, our
findings revealed no statistically significant differences between
the two cohorts concerning various parameters, including hospital
length of stay (LOS), the occurrence of post-operative SSI, and the
choice of SSI intervention as outlined in [Table 2]. It is noteworthy
that only two patients in our study population developed SSI, and
in both cases, antibiotics were administered as the SSI intervention.
Notably, neither of the two SSI patients required an emergency room
(ER) visit, office visit, or re-admission within 30 days post-operation.
The sole statistically significant discrepancy between the two
cohorts pertains to the surgical approach. Our results indicated that
patients who received a preoperative CHG bath were significantly
more likely to have undergone laparoscopic surgery compared to
those who did not receive such treatment (95.3% vs. 76.7%; P=0.007),
as detailed in [Table 1].
Discussion
Surgical site infections in adnexal procedures for benign
diseases have not been extensively documented. Our study, as
presented in [Table S1], reports an SSI rate of 1.8%. While CHG
baths may potentially contribute to SSI prevention in specific cases,
their effectiveness within the pediatric population remains an
underexplored area of research. To our knowledge, this study marks
the inaugural attempt to assess the utility of preoperative antiseptic
chlorhexidine solutions in pediatric patients undergoing adnexal
surgery.
Although CHG has demonstrated efficacy in reducing bacterial
skin colonization, a Cochrane systematic review, incorporating data
from 13 trials conducted between 1983 and 2011, did not show a
benefit for chlorhexidine bathing or showering in various surgical
procedures when compared to a placebo.[12] Similarly, our study
revealed no significant difference in the rate and risk of SSI when
utilizing CHG or not. In our cohort, only two patients developed
surgical site infections, and both were effectively managed with
antibiotic therapy without requiring readmission or reoperation.
In the pediatric population, some laparoscopic procedures have
shown a reduction in SSI rates compared to open procedures, such
as laparoscopic appendectomies (odds ratio of 2.22 [1,19,4,5],
p = 0.01).[13]However, this is not universally applicable; for other
procedures such as laparoscopic fundoplication for gastroesophageal
reflux, inguinal hernia repair, or pyloromyotomy for pyloric stenosis,
there is no difference in SSI rates.[13,14]Our study suggests that
patients without a preoperative CHG bath were significantly more
likely to have undergone laparoscopic surgery compared to those
who had a preoperative CHG bath (95.3% vs. 4.7%, p-value 0.007).
This finding can be attributed to the emergent nature of laparoscopic
adnexal torsion treatment. Emergency surgeries do not undergo
preoperative CHG baths to avoid further delays in care. Although
further studies are warranted to assess differences in SSI rates in
pediatric patients undergoing laparoscopic versus open procedures,
our study concludes that the use of CHG does not significantly impact
SSI rates regardless of the surgical approach.
A 2019 Cochrane review, based on very low certainty evidence in
critically ill patients, highlighted the uncertainty regarding whether
CHG baths reduce hospital-acquired infections, mortality, or length
of stay, or whether chlorhexidine use leads to more skin reactions.[11]
While preoperative bathing with CHG may serve as a cost-effective
tool to reduce SSIs in specific surgical procedures, it is not without
its risks. The National Center for Health Statistics reports that 27.2%
of children have allergies, and allergic contact dermatitis has become
increasingly prevalent in children in recent years.[15]CHG may cause
a wide range of side effects, including skin irritation, allergic reactions
(contact dermatitis, photosensitivity, anaphylaxis), eye problems
upon direct contact, deafness if exposed to the tympanic membrane,
stomach irritation/nausea if ingested, and acute respiratory distress
syndrome (ARDS) if aspirated in high concentrations into the lungs.
The FDA has identified 52 reported cases of anaphylaxis, a severe
form of allergic reaction, associated with the use of chlorhexidine
gluconate products applied to the skin from 1969 to 2015, and this
figure does not encompass unreported cases or recent data.[16]
Although our study does not investigate the incidence of adverse
effects in our cohort, it is imperative to recognize that many children
often suffer from childhood allergies and skin sensitivities that may
be influenced by operative skin preparations. Our study concludes
that the use of CHG baths prior to adnexal surgery for benign disease
in pediatric patients does not significantly improve outcomes.
Therefore, limiting exposure to potential allergens, such as CHG,
may reduce complications and should be taken into account when
devising hospital policies.
Our study is constrained by its retrospective nature, sample size,
and reliance on data collected from a single institution. Additionally,
risk factors known in adults to contribute to the development of SSIs,
such as intraoperative temperature, operative time, and glycemic
control, were not evaluated in this study. Furthermore, our study
does not directly assess the side effects of SSIs or provide a cost
analysis of preoperative chlorhexidine baths. Larger multicenter
studies examining outcomes would enhance our understanding of
whether preoperative antisepsis with CHG reduces postoperative
SSI and readmission rates or holds any clinical benefit for pediatric
patients. As part of the process for evaluating the quality and safety of
care delivery, hospital policies must be critically reviewed.
Conclusion
This study suggests a 1.8% surgical site infection rate in pediatric
patients undergoing adnexal surgery for benign conditions. The
assessment of patient outcome parameters within our study
population revealed that the use of a CHG preoperative bath did not
result in statistically significant differences in the occurrence of SSI
among pediatric patients undergoing adnexal procedures for benign
etiologies. However, it’s important to recognize that the utilization
of CHG carries certain risks. Therefore, to enhance patient care
and formulate clinical recommendations, further studies should be
conducted.