Journal of Surgery
Download PDF
Case Report
*Address for Correspondence: Donald Bramwell, International Musculoskeletal Research Institute, Department of Orthopaedic Surgery, Flinders Medical Centre, Bedford Park SA 5042, Australia, Tel: 08 8204 4673; Fax: 08 8374 0832; E-mail: donald.bramwell@health.sa.gov.au
Citation: Grosser D, Benveniste SH, Bramwell D, Krishnan J. Early Migration of the R3 Uncemented Acetabular Component: A Prospective 2 Year Radiostereometric Analysis. J Surgery. 2013;1(2): 5.
Copyright © 2013 Grosser D, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Surgery | ISSN: 2332-4139 | Volume: 1, Issue: 2
Submission: 30 September 2013 | Accepted: 25 October 2013 | Published: 29 October 2013
Reviewed & Approved by: Dr. Hui B. Sun, Department of Orthopaedic Surgery and Radiation Oncology, Albert Einstein College of Medicne, USA
Early Migration of the R3 Uncemented Acetabular Component: A Prospective 2 Year Radiostereometric Analysis
Grosser D, Benveniste SH, Bramwell D*, and Krishnan J
- International Musculoskeletal Research Institute, Department of Orthopaedic Surgery, Flinders Medical Centre, Bedford Park SA 5042, Australia
*Address for Correspondence: Donald Bramwell, International Musculoskeletal Research Institute, Department of Orthopaedic Surgery, Flinders Medical Centre, Bedford Park SA 5042, Australia, Tel: 08 8204 4673; Fax: 08 8374 0832; E-mail: donald.bramwell@health.sa.gov.au
Citation: Grosser D, Benveniste SH, Bramwell D, Krishnan J. Early Migration of the R3 Uncemented Acetabular Component: A Prospective 2 Year Radiostereometric Analysis. J Surgery. 2013;1(2): 5.
Copyright © 2013 Grosser D, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Surgery | ISSN: 2332-4139 | Volume: 1, Issue: 2
Submission: 30 September 2013 | Accepted: 25 October 2013 | Published: 29 October 2013
Reviewed & Approved by: Dr. Hui B. Sun, Department of Orthopaedic Surgery and Radiation Oncology, Albert Einstein College of Medicne, USA
Abstract
Background: Radiostereometric Analysis (RSA) is a highly accurate and true three dimensional method that analyses implant micromotion following total joint replacement surgery. This methodology was used to assess the migration of a fourth generation acetabular shell: the R3 acetabular component (Smith & Nephew, Memphis, Tennessee) which utilises an enhanced porous ingrowth surface (StikTite). The StikTite surface has previously been evaluated in an RSA study, but on the Reflection Cup.Methods: Twenty patients undergoing primary total hip arthroplasty were recruited and all had the R3 acetabular cup inserted. RSA examinations were performed immediately post operatively and at 6, 12 and 24 months. One patient was removed as they required early revision, three for technical reasons (inaccurate bead placement) and two were lost to follow up. Data was analysed for the remaining fourteen patients. Eight patients received a cementless femoral stem (Anthology; Smith and Nephew) with oxynium femoral heads (32 mm) and twelve a cemented femoral stem (Spectron; Smith and Nephew) with cobalt chrome femoral heads.
Results: RSA revealed no significant migration in all planes of translation and rotation. Mean translations at 2 years were 0.36 mm (x-axis), 0.39 mm (y-axis) and 0.35 mm (z-axis). Mean rotations were 0.68 deg (x-axis), 0.99 deg (y-axis) and 0.77 deg (z-axis). Micromotion along the proximal-distal translation (y-axis) plane represents proximal migration of the acetabular component.
Conclusions: Mean translations and rotations were higher than previously reported for the StikTite coating applied to the older Reflection cup. The levels of early proximal migration two years postsurgery were within published ‘acceptable’ levels, albeit within the ‘at risk’ range of 0.2-1.0 mm. These findings support further investigation and analysis of the R3 acetabular system, and continuing correlation with registry data as it becomes available.
Introduction
Cementless acetabular components in total hip arthroplasty (THA) have become increasingly popular over the last few decades [1], being used in 94.6% of primary THA in Australia in 2011 [2]. The R3 acetabular component (Smith & Nephew, Memphis, Tennessee) is a modular 4th generation cementless acetabular system which was initially provided with three bearing surfaces inside a titanium alloy shell - cross-linked poly, ceramic and metal (cobalt chrome). The metal-on-metal components have subsequently been recalled due to higher rates of revision, however the R3 system with poly or ceramic surfaces remains the third most commonly implanted acetabular shell in Australia [2].The R3 shell utilises a three dimensional asymmetric titanium powder coating (StikTite) with 60% porosity compared with traditional porous coatings with 45% or lower porosity. In a prospective study of 20 patients, Bourne et al. demonstrate less micromotion of a Reflection cup (Smith & Nephew, Memphis, Tennessee) coated in StikTite when compared with a prior study of Reflection cups coated with a traditional sintered bead coating (Rough coat, Smith & Nephew) [3,4]. By making the first post-surgery RSA measurements early, the authors of these two studies report that the initial migration of the acetabular cup occurred in the first six week [3] and two months [4]. To date, however, there have not been any published reports on the R3 system itself.
Aseptic loosening or lysis remains the most common cause for implant failure - in Australian 2012 registry data representing 29% of all revisions [2]. National registry data can be used to identify components that are performing sub-optimally, however as has been recently demonstrated with the Articular Surface Replacement (ASR) prosthesis (De Puy, Warsaw, Indiana) which was withdrawn by the manufacturer in 2010, a large number of prostheses may be implanted prior to sufficient data being available to warrant a recall.
Radiostereometric Analysis, also known as Roentgen Stereophotogrammetric Analysis, is a method that allows highly accurate assessment of implant migration, and can be used to predict prostheses likely to fail within one to two years post-operatively [5]. Clinical RSA study results are recorded in terms of translations and angular rotations, with all degrees of freedom reported. RSA interprets mediolateral (x-axis), proximal-distal (y-axis) and anteroposterior (z-axis) translations along with rotations, anteroposterior tilt (x-axis rotation), anteversion-retroversion (y-axis rotation) and increase-decrease inclination (z-axis rotation) [7]. Translations should always be represented as millimetres and rotations as degrees [7].
As a short term predictor of the long term survival of an implant, the RSA technique allows in vivo three dimensional measurements of prosthesis translation with an accuracy of 0.2 mm and rotation accuracy of 0.5 degrees with clinically relevant information able to be produced from short study follow-ups and small study sizes [5]. In a recent systematic review and meta-analysis of RSA and survival studies of acetabular cups of 700 cups with RSA migration data and 38 013 cups with survival data from national joint registries, Pijls et al. propose that RSA results two years following hip replacement and from a small number of patients (10-60) could indicate proximal migration likely to lead to revision through lysis or loosening over the next 5-10 years [8].
These authors conclude that there is a clinically relevant association between early movement of acetabular cups and longer term revision caused by loosening. They demonstrate that, for every additional millimeter of proximal migration at two years, there was a 10% increase in revision rate. They propose that early migration thresholds should be established to enable early detection of cups at risk of failure over 5-10 years. Pijls et al. find that a 2 year proximal migration rate of 0.2 mm should be considered acceptable, greater than 1 mm unacceptable and cups with proximal migration in the range of 0.2 mm - 1 mm considered at risk of having revision rates higher than 5% at 10 years [8].A prospective trial of 41 THA over a 10 year period with clinical and RSA evaluation shows that during the first two post-operative years cranial translation and sagittal rotation are strong risk factors for later aseptic loosening [6]. Whilst the cups studied in this trial were cemented, the authors propose that the results should also be applicable to other types of acetabular cups.
In a study comparing ceramic-on-ceramic with metal-onpolyethylene implants, Zhou et al. [4] report acetabular migration along all planes of translation and rotation. In the metal-onpolyethylene group, patients receiving a Reflection cup (Smith & Nephew, Memphis, Tennessee) and a Spectron/EF (Smith & Nephew, Memphis, Tennessee) cemented femoral stem, demonstrat a mean proximal migration of 0.31 mm at 24 months [4].
National joint registry data provide a record of revisions performed in the full range of prostheses. The Australian Joint Registry (AOA NJRR) [2] has almost complete records of all hip and knee replacement in Australia with over 93.9% of Registry records verified against health department data and further data obtained from retrieval of unreported records. The R3 has been the third most used acetabular component in primary total conventional hip replacement in Australia from 2008 to 2011 [2]. The 2611 instances of use in 2011, all except four of which were with cementless fixation, represent 9.9% of all acetabular components implanted. The combination of the R3 acetabular cup with the Anthology cementless femoral stem (Smith and Nephew) is reported in the 2012 AOA National Register of Joint Replacements as having 1.00 revisions per 100 observed years (with confidence interval of 0.71 to 1.37), which is within the reported revision rate for all cementless combinations of 0.94 (confidence interval 0.92-0.97) per 100 observed years [2]. The cumulative percent revision of this combination is 1.7 (1.2, 2.3) at one year and 2.2 (1.6, 3.0) at three years. The combination of R3 and Spectron/EF (Smith and Nephew) cemented femoral component shows 1.64 revisions per 100 observed years (with confidence interval of 1.03 to 2.49) against 0.65 (0.63, 0.68) revision rate for all hybrid combinations [2]. The cumulative percent revision of this combination is 1.6 (0.9, 2.8), 3.7 (2.4, 5.8) at one and three years respectively. The R3-Spectron/EF combination was indicated in the 2011 Joint Registry report as having a higher than anticipated revision rate of 2.3 (1.3, 4.1) but 2012 registry data shows that, although it seems large, the revision rate is no longer significantly different from the whole cohort of hybrid combinations.
No prior RSA studies of the R3 acetabular cup have been published, however the Bourne et al. [3] study of Reflection cups with the StikTite coating reveals very low cup migration with mean individual cup translations less than 0.1 mm and mean rotations below 0.35 deg at 6 weeks, 3, 6 and 12 months.
Patient outcomes following total hip arthroplasty are commonly determined by scoring patients, or asking patients to rate themselves, across domains including pain and impact of daily activities. Two of the more frequently used scoring systems with determined reliability are the Harris Hip Score [10] and the Hip Disability and Osteoarthritis Outcome Score (HOOS) [11]. The Harris Hip Score scale ranges from 0 (worst) to 100 (best). This scoring method has a long history of use and is well accepted in the orthopaedic community. HOOS is a patient-administered instrument used to obtain the patient’s opinion about their hip and associated problems during the previous week. The HOOS is intended to be used for hip disability with or without osteoarthritis (OA) and has been used to assess changes in the hip following treatments including total hip replacement, medication and/or physical therapy. HOOS consists of 5 subscales; pain, other symptoms, function in daily living, function in sport and recreation, and hip related quality of life. Five possible responses are allowed for each question and each answer equates to a score of 0 to 4. Points equating to the responses for each subcategory are added together and normalized to a maximum total score of 100. A systematic review of over 1300 articles [12] shows that between 7% and 23% of people report ongoing pain following hip replacement outcome in studies, with the more rigorous studies reporting an unfavourable pain outcome was reported in 9% of patients.
We report the two-year RSA migration and patient outcomes data for the R3 acetabular cup implanted with two different femoral stems.
Patients and Methods
Twenty patients requiring a primary total hip arthroplasty due to non-inflammatory degenerative joint disease, including osteoarthritis, were recruited for the trial. The median age was 70 years (range, 53-87 years) and the median body mass index was 26 (range, 22-38). Study patients received the R3 Acetabular System (Smith and Nephew), all with poly liners. Eight patients received a cementless femoral stem (Anthology; Smith and Nephew) with oxynium femoral heads (32 mm) and twelve a cemented femoral stem (Spectron; Smith and Nephew) with cobalt chrome femoral heads (eleven 32 mm heads and one 28 mm). Ten tantalum markers (0.8 mm diameter; RSA Biomedical, Umea, Sweden) were placed in a standardised formation [7] across the acetabulum whilst six tantalum markers (1.0 mm diameter; RSA Biomedical, Umea, Sweden) were placed in the outer rim of the polyethylene liner at the time of surgery. Baseline RSA examinations were performed at discharge within five days of surgery and again at 6, 12 and 24 months postoperatively. All RSA examinations were taken with patients in a supine position. A ceiling-mounted radiographic tube and a mobile radiographic tube were used simultaneously to take exposures of the hip with a calibration cage (Uniplanar Cage Number 43; RSA Biomedical). Acetabular migration was measured by movement of the acetabular cup relative to the acetabulum, whilst polyliner wear was measured by movement of the femoral head relative to the polyliner of the cup, using the UmRSA software (v6.0; RSA Biomedical). The accuracy of the technique was influenced by the stability and distribution of tantalum markers, determined by the mean error of rigid body fitting and the condition number respectively. A cut-off level of 0.30 mm for the mean error of rigid body fitting and 120 for the condition number were used for exclusion of patients from the analysis [7]. From the twenty patients recruited, one required revision (R3-Spectron/EF combination) prior to 6 month follow-up. Nineteen patients had RSA follow-ups with radiographs performed postoperatively at 6 and 12 months. RSA data could not be generated for one patient due to inaccurate bead placement and this patient was excluded from further analysis in the study.From the remaining eighteen patients, two were unable to complete RSA follow-ups with radiographs at 24 months (one patient died and the other missed a visit). From the RSA follow-ups at 24 months, two patients provided unsuitable RSA analyses due to lack of precision in acetabular bead spread.
Therefore, acetabular cup migration could be determined for fourteen patients 6, 12 and 24 months postoperatively. Of these fourteen remaining patients, eight received the Spectron/EH femoral stem and six received the Anthology. From the cases reported, it should be noted that markerless cup analysis was utilised for the complete RSA follow-up of two patients.
Patient outcomes were measured using the Harris Hip Score and the Hip Disability and Osteoarthritis Outcome Score (HOOS). These questionnaires were completed preoperatively and at 6, 12 and 24 months postoperatively.
Ethics approval was obtained for this study from the relevant local Human Research Ethics Committee. All patients provided informed consent for the insertion of tantalum markers during surgery and the subsequent RSA radiographs.
Results
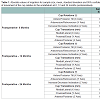
Acetabular migrationAbsolute migration of the acetabular cups along each axis of movement was calculated at 6, 12 and 24 months postoperatively (Table 1). In all three directions mean translations were below 0.40 mm and mean rotations were below 1 deg at 24 months. The data demonstrates that migration of the acetabular cup occurred primarily in the first study follow-up at 6 months postoperatively. Proximal migration of the acetabular cup for patients implanted with a cemented femoral stem (Spectron/EH) and a cementless femoral stem (Anthology) was calculated at 6, 12 and 24 monthspostoperatively (Figure 1). The mean proximal migration of the acetabular cup for both cup-stem combinations was 0.39 mm (CI 0.19-0.58), with the data indicating that there might be greater cup migration associated with the cementless femoral stem, 0.45 mm (CI 0.09-0.98) than with the cemented femoral stem, 0.35 mm (CI 0.24-0.45). Outcome measures
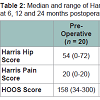
Patient outcome measures were calculated preoperatively and at 6, 12 and 24 months postoperatively (Table 2). A significant difference in the Harris Hip Score, Harris Pain Score and Hip Disability and Osteoarthritis Outcome Score (HOOS) was observed when comparing pre-operative with 6 months, 12 months and 24 months (p < 0.0001).
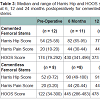
In comparing the patient outcome measures between cemented and cementless femoral stems (Table 3), a difference, however not significant, was observed between the HOOS scores at 24 months (p = 0.0549).
Discussion
The proximal migration of the R3 acetabular cup, at 0.39 mm, was greater than the safe cut off level of 0.2 mm proposed by Pijls et al., placing the cup in the lower end of the ‘at risk’ range [8]. In comparison, the proximal migration of the R3 acetabular cup in this study was similar to the Reflection cup, at 0.31 mm, with a traditional sintered bead coating [4]. Rotation results and the associated confidence intervals from this study were also similar to those reported by Zhou et al. [4].Translation and rotation results of the R3 acetabular cup were larger than reported for StikTite with the Reflection cup [3]. Similarly to Bourne et al., the R3 acetabular cup indicated acceptable fixation stability after an initial period of migration, which in this study was 6 months [3].
Comparison of proximal migration for cemented (0.35 mm) and cementless (0.45 mm) femoral stems expressed similar results 24 months postoperatively. The confidence intervals in this study were similar to those reported by Bourne et al., who utilised a similar prosthesis, sample size and RSA technique in determining micromotion [3]. This study demonstrated that the proximal migration of the Reflection cup remained in the lower end of the ‘at risk’ range of 0.2-1 mm [8] when comparing both the cemented and cementless femoral stems. At both 12 and 24 months a 0.1 mm difference was maintained for the proximal migration between the cemented and cementless femoral stems, however this difference was within the confidence intervals observed.
Although the sample size in each group was small, there was no statistically significant difference between the cemented and cementless stems with the R3 cup. This is an observation that needs to be monitored and compared to registry data.
This study demonstrated an improvement in patient outcome measures post-surgery, however no clinical significance between HOOS outcomes measures were indicated between patients who received a cemented or cementless femoral stem, even though patients with a cemented femoral stem reported a better pre-operative measure.
A limitation of this study was the inclusion of data from two patients where the markerless RSA algorithm was used to analyze migration and wear data. Borlin et al. demonstrated the potential of the markerless RSA algorithm by accurately assessing femoral head penetration, stating that whilst the accuracy for translations was good, rotations were slightly less accurate [8]. In this study, when comparing the R3 acetabular component with other components in the literature, we only report the proximal migration as represented by micromotion along the proximal-distal translation (y-axis) plane. The small number of participants is a further limitation although the confidence intervals and techniques are similar to those reported in other papers.
This study has shown that, although the migration of the R3 acetabular cup is not significantly large and the performance of the cup and the femoral stems falls within acceptable revision rates reported in the Australian Joint Registry, the R3 (with both the cementless Anthology and cemented Spectron/EF stem combinations) warrants further investigation.
These findings would support further investigation and analysis of the R3 acetabular system, and correlation with registry data as it becomes available.
References
- Ries MD (2008) Review of the evolution of the cementless acetabular cup. Orthopedics 31.
- AOA (2012) Australian Orthopaedic Association National Joint Replacement Registry. Annual Report. Adelaide, AOA : s.n.
- Bourne RB, McCalden RW, Naudie D, Charron KD, Yuan X, et al. (2008) The next generation of acetabular shell design and bearing surfaces. Orthopedics 31.
- Zhou ZK, Li MG, Borlin N, Wood DJ, Nivbrant B (2006) No increased migration in cups with ceramic-on-ceramic bearing: an RSA study. Clin Orthop Relat Res 448: 39-45.
- Karrholm J, Borssen B, Lowenhielm G, Snorrason F (1994) Does early micromotion of femoral stem prostheses matter? 4-7-year stereoradiographic follow-up of 84 cemented prostheses. J Bone Joint Surg Br 76: 912-917.
- Nieuwenhuijse MJ, Valstar ER, Kaptein BL, Nelissen RG (2012) Good diagnostic performance of early migration as a predictor of late aseptic loosening of acetabular cups: results from ten years of follow-up with Roentgen stereophotogrammetric analysis (RSA). J Bone Joint Surg Am 94: 874-880.
- Valstar ER, Gill R, Ryd L, Flivik G, Borlin N, et al. (2005) Guidelines for standardization of radiostereometry (RSA) of implants. Acta Orthop 76: 563-572.
- Borlin N, Rohrl SM, Bragdon CR (2006) RSA wear measurements with or without markers in total hip arthroplasty. J Biomech 39: 1641-1650.
- Pijls BG, Nieuwenhuijse MJ, Fiocco M, Plevier JW, Middeldorp S, et al. (2012) Early proximal migration of cups is associated with late revision in THA: a systematic review and meta-analysis of 26 RSA studies and 49 survival studies. Acta Orthopaedica 83: 583-591.
- Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by moldarthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51: 737-755.
- Nilsdotter AK, Lohmander LS, Klassbo M, Roos EM (2003) Hip disability and osteoarthritis outcome score (HOOS)--validity and responsiveness in total hip replacement. BMC Musculoskelet Disord 4: 10.
- Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P (2012) What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patient. BMJ Open 2: e000435.