Journal of Surgery
The Role of Wider Safety Margins in the Prognosis of the Basal Cell Carcinoma of the Face and Scalp
Abdou MA Darwish*
- Department of Plastic Surgery, Faculty of Medicine, Minia University, Egypt
*Address for Correspondence: Abdou MA Darwish, Department of Plastic Surgery, Faculty of Medicine, Minia University, Egypt, Tel: 02 086 2344974; Fax: 02 086 2342015; E-mail: abdoudarwish@hotmail.com
Citation: Darwish AMA. The Role of Wider Safety Margins in the Prognosis of the Basal Cell Carcinoma of the Face and Scalp. J Surgery. 2014;2(1): 3.
Copyright © 2013 Darwish AM. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Surgery | ISSN: 2332-4139 | Volume: 2, Issue: 1
Submission: 06 February 2014 | Accepted: 28 February 2014 | Published: 04 March 2014
Reviewed & Approved by: Dr. Josef Kainz, Department of General ENT, Medical University of Graz, Austria
Abstract
The aim of this study was to assess the wider safety margins and its role in recurrence rate of the Basal Cell Carcinoma of the face and scalp. We excise the basal cell carcinoma with wider safety margins (5 mm). In all patients there were safety margins of 0.5 mm in all directions of the tumor, peripheral and deep margins, and histopathological study of the excised lesions revealed clear surgical margins and deep layer from the tumor cells and follow-up for 3 years revealed no recurrence in any of our patients. The best cosmetic appearance was obtained in cases reconstructed by rhomboid flaps and only one case reconstructed by forehead flap needed revision.Keywords
Basal Cell carcinoma (BCC); Recurrence; Wider safety marginsIntroduction
Basal Cell Carcinomas (BCCs) are the most common forms of skin cancer [1]. They rarely metastasize but are often locally aggressive, with a small percentage showing multiple recurrences. They also have a possible, although as yet unproven, adnexal origin and often show differentiation toward adnexal structures [2,3]. Usually, basal cell carcinoma (BCC) appears as a slowly growing tumor arising on sun-exposed areas of the body; the face being the most common site [4]. It is well-known that recurrence rates are higher for larger and previously recurrent tumors, as well as for more aggressive histologic subtypes [5-9].In this study, I used wider safety margins technique to assess their role in recurrence rate.Patients and Methods
PatientsAll patients were subjected to thorough history taking, routine clinical examination in addition to essential laboratory investigations and tissue biopsy (punch biopsy) analysis. All patients have given written informed consents for the surgical interference as well as for enrollment in the study.
Surgical procedure
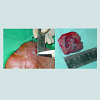
The different presentations of the patients were: BCC of the cheek (10), nasolabial fold (7), nose (5), upper lip (5), forehead (5), lower eye lid (3), outer canthus (3), inner canthus (2), and scalp (5) cases (Table 2). There were variations in surgical techniques according to the site, size and availability of the tissue around the tumor, but all the surgical procedures were performed as follows: clinically clear margins were determined around the tumor by sterile marker, a 5 mm rigorous safety margins around the tumor were marked (Figure 1). Local anesthesia was obtained with infiltration of lignocaine 0.1%: with adrenaline one in 100,000, which was injected beneath and around the area marked for excision and subsequent reconstruction, and the excised specimen was marked with a suture to provide orientation. The excised specimen was submitted for histologic confirmation of the diagnosis and examination for clearness of the surgical margins. Reconstruction was performed with different types of local faciocutanous flaps (rhomboid, rotational, island and advancement flap), the wound were closed in layers using 4/0 Vicryl and 5/0 proline. 5-7 days postoperatively the sutures were removed and follow-up of the patient in the hospital clinic was carried out at one to three months for the first year, and every six to12 months for the next 2 years.
Results
Through 4 years 45 patients with Basal Cell Carcinoma (BCC) of the face treated by surgical excision with safety margins and reconstruction of the defect by local flap. The size of the lesion with the safety margins varies from 2-4 cm in diameter. In all patients there were safety margins of 0.5 mm in all directions of the tumor, peripheral and deep margins, and histopathological study of the excised lesions revealed clear surgical margins and deep layer from the tumor cells and follow-up for 3 years revealed no recurrence in any of our patient. The best cosmetic appearance was obtained in cases reconstructed by rhomboid flaps (Figures 2, 3 and 4) and only one case reconstructed by forehead head flap needed revision.Discussion
Most basal-cell carcinomas are treated worldwide by surgical excision [10]. The recurrence rate for basal cell carcinoma after complete conventional surgical excision is low in the order of 1% [11]. The standard surgical margin for primary nonmelanoma skin cancers is 4 mm [12,13]. In a study done by Kimai Asadi et al. they found that narrow-margin elliptical excision with margins up to 3 mm is only 80% effective in clearing these tumors [14]. In our study we used wider safety margin (5 mm) in 45 patients with different forms of basal cell carcinoma of the face and scalp, the wide safety margin does not affect the cosmetic appearance after excision of the Basal Cell Carcinoma but had reduced the recurrence rate and tumor infiltration to the resection margins to 0%. Also we used different reconstructive procedures according to the tissue availability (rhomboid and rotational flaps had the best cosmetic appearance while the results of island and advancement flaps was satisfactory).References
- Quinn AG, Sikkink S, Rees JL (1994) Basal cell carcinomas and squamous cell carcinomas of human skin show distinct patterns of chromosome loss. Cancer Res 54: 4756-4759.
- Kocsard E (1997) Solar keratoses and their relationship to non-melanoma skin cancers. Australas J Dermatol 38: S30.
- Wade TR, Ackerman AB (1978) The many faces of basal-cell carcinoma. J Dermatol Surg Oncol 4: 23-28.
- Richmond-Sinclair NM, Pandeya N, Ware RS, Neale RE, Williams GM, et al. (2008) Incidence of basal cell carcinoma multiplicity and detailed anatomic distribution: longitudinal study of an Australian population. J Invest Dermatol 129: 323-328.
- Kuijpers DI, Thissen MR, Neumann MH (2002) Basal cell carcinoma: treatment options and prognosis, a scientific approach to a common malignancy. Am J Clin Dermatol 3: 247-259.
- Netscher DT, Spira M (2004) Basal cell carcinoma: an overview of tumor biology and treatment. Plast Reconstr Surg 113: 74e-94e.
- Silverman MK, Kopf AW, Bart RS, Grin CM, Levenstein MS (1992) Recurrence rates of treated basal cell carcinomas. Part 3: Surgical excision. J Dermatol Surg Oncol 18: 471-476.
- Rowe DE, Carroll RJ, Day CL Jr (1989) Long-term recurrence rates in previously untreated (primary) basal cell carcinoma: implications for patient follow-up. J Dermatol Surg Oncol 15: 315-328.
- Rowe DE, Carroll RJ, and Day CL Jr (1989) Mohs surgery is the treatment of choice for recurrent (previously treated) basal cell carcinoma. J Dermatol Surg Oncol; 15: 424-431.
- Goldberg LH (1996) Basal cell carcinoma. Lancet 347: 663-667.
- Griffiths RW, Suvarna SK, Stone J (2005) Do basal cell carcinomas Recur after complete conventional surgical excision? Br J Plast Surg 58: 795-805.
- Wolf DJ, Zitelli JA (1987) Surgical margins for basal cell carcinoma. Arch Dermatol 123: 340-344.
- Thomas DJ, King AR, Peat BG (2003) Excision margins for nonmelanotic skin cancer. Plast Reconstr Surg 112: 57-63.
- Kimyai-Asadi A, Alam M, Goldberg LH, Peterson SR, Silapunt S, et al. (2005) Efficacy of narrow-margin excision of well-demarcated primary facial basal cell carcinomas. J Am Acad Dermatol 53: 464-468.