Journal of Surgery
Download PDF
Case Report
The Silent Band: Not Loud Enough? Asymptomatic Gastric Band Erosion: A Case Report
AlHabib R1, Kayali N1, Al Rashed A1* and Al-Jaser W2
1Department of Surgery, Al Amiri Hospital, MOH, Kuwait
2Department of Gastroenterology, Al Amiri Hospital, Kuwait
*Address for Correspondence:
Al Rashed A, Department of Surgery, Al Amiri Hospital, MOH, 25 Gulf Road
13041, Kuwait City, State of Kuwait, Phone: +965 22450005 (Ext: 5500); Email:
asmaalrashed@dr.com
Submission: 02 July, 2022
Accepted: 01 August, 2022
Published: 06 August, 2022
Copyright: © 2022 AlHabib R, et al. This is an open access article
distributed under the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided the
original work is properly cited.
Abstract
Background: Laparoscopic adjustable gastric band (LAGB)
is a common and an effective bariatric procedure. It involves the
placement of an adjustable band with an inflatable balloon at the
gastric cardia near the gastroesophageal junction. However, several
complications have been reported. These include port-site infections,
slippage of the band, and band erosion.
Case summary: A 44 years-old female who was found to have
an eroding gastric banding during esophagogastroduodenoscopy
incidentally. The gastric band was placed laparoscopically five years
prior to presentation. The band was removed successfully through
an endoscopic laparoscopic-assisted technique under general
anesthesia. Starting endoscopically, the eroded gastric band was
visualized and then broken using a mechanical lithotripter. However,
a small portion of the band remained embedded in the mucosa and
prevented the retrieval. Simultaneously, laparoscopy revealed intraabdominal
adhesions which were released, freeing the gastric band
into the stomach and allowing extraction of the gastric band using a
snare was completed endoscopically while ensuring examination of
intact gastric mucosa. The post-operative course and follow up were
uneventful.
Conclusion: Eroded LAGB can be silent necessitating life-long
follow-up. Endoscopic laparoscopic-assisted approach allows
definitive management, examining gastric wall integrity and leaks
simultaneously.
Keywords
Laparoscopic adjustable gastric banding; Surgery;
Erosion; Weight loss; Bariatric and Metabolic Surgery; Revisional Surgery
Introduction
Laparoscopic adjustable gastric band (LAGB) is a bariatric
procedure that involves placement of an adjustable band with an
inflatable balloon at the gastric cardia near the gastroesophageal
junction. Placing this band will limit the amount of food consumption
promoting early satiety and progressive weight loss with time. LAGB
is a common bariatric surgery procedure ranking as the third most
common in the United States. However, several complications have
been implicated with the use of banding including pouch dilatation
(11%), band infection (1%) band erosion (28%) [1]. As with any
procedure, advantages and disadvantages must be highlighted. LAGB
is the least invasive bariatric procedure with an advantage of it being
adjustable and reversible. No anatomic rearrangements are done;
therefore, it has the lowest morbidity and mortality rates amongst
other bariatric procedures. However, slower rates of weight loss, up
to 40% to 54% of excess weight loss, are implicated in comparison
to other procedures like laparoscopic sleeve gastrectomy (LSG)
and laparoscopic Roux-en-Y Gastric Bypass (LRYGB); 49%-56%
and 55%-66% respectively [2]. Complications of LAGB may arise
including band slippage, band infection, and band erosion. Band
erosion is a late complication occurring at a mean of 22 months after
surgery. It may result either due to gastric wall ischemia from an
excessively tight band, mechanical trauma related to the band buckle
or thermal trauma from electro surgical energy sources used during band placement. Patients complicated with band erosion present
with abdominal pain, weight regain, nausea and vomiting. It may
also result in intragastric migration, partial or complete. Conversion
to other bariatric procedures such as LSG and RYGB are an option
once LAGB has failed whether due to inadequate weight loss or if
any complications have occurred. Gastric bypass has better outcomes
than gastric band procedures for long-term weight loss, type 2
diabetes controls and remission, hypertension, and hyperlipidemia
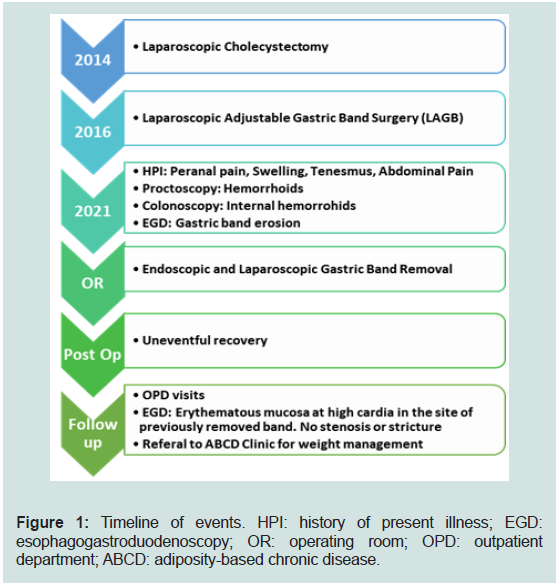
[3] (Figure 1).
Case Report
A 44-year-old female presented to the out-patient department
with a one-month history of perianal pain, swelling and tenesmus.
The perianal pain was sharp in nature, exacerbated by defecation and
lasted for multiple hours. She has a history of chronic constipation
for the past seven years and passes stool with straining, she had used local treatments such as ointments and suppositories. Additionally,
the patient reports abdominal pain and vomiting of one month
duration that occurred after heavy meal consumption with a
sensation of food impacted in the stomach. Past surgical history
revealed laparoscopic cholecystectomy seven years ago and LAGB
five years ago performed in another institution with a total of 17kg
weight loss. Her family history was positive for bowel cancer affecting
both her mother in the 7th decade and paternal uncle in his 8th decade.
The patient’s general appearance and vital signs were normal.
Her measurements were height 171 centimetres (cm), weight 87.2
kilograms (kg), and body mass index (BMI) 28.8 cm/kg. Abdominal
examination revealed mild tenderness in the epigastric area, without
distention, rigidity, or peritonitis. Proctoscopy showed grade II
hemorrhoids at 11 o’clock and grade I hemorrhoids at 3 and 9 o’clock
positions. The patient was advised for lifestyle changes and a decision
was made to proceed with colonoscopy to rule out malignancy and
esophagogastroduodenoscopy (EGD) for gastric band surveillance.
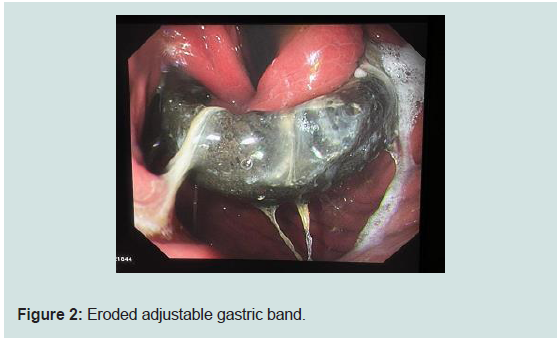
The colonoscopy showed internal hemorrhoids; however, EGD
showed gastroesophageal (GEJ) at 37 cm, normal esophagus, the
gastric band eroding the gastric wall (nearly 2/3 of band circumference
was visualized) and migrated upwards, just below the GEJ by 2 cm
(Figure 2). The rest of the examination was unremarkable. A Barium
meal showed that the gastric band is noted in the proximal part of the
stomach but appears relatively superiorly located with an increased
phi angle, measuring 70 degrees, suggestive of displacement with mild
superior migration of the gastric band and no leak. The findings were
consistent with the diagnosis of gastric band erosion. The diagnosis
and the management options with risks, benefits and complications
were discussed with the patient. She consented for endoscopic, and/
or laparoscopic and/or open laparotomy for eroded gastric band
removal.
The patient was admitted to the hospital and followed preoperative
assessment as per protocol. Preparation and coordination
with the intervention gastroenterologist team was arranged. The
patient was brought to the operating room, placed in supine position,
and underwent general anesthesia with endotracheal intubation.
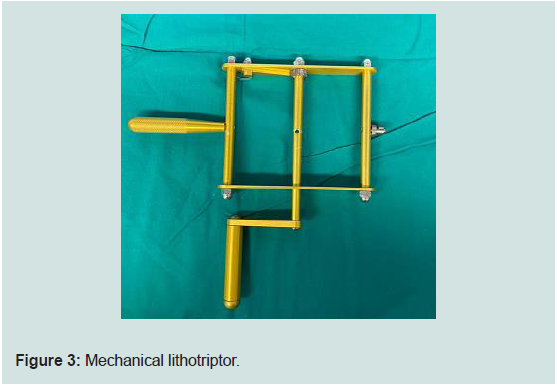
Starting with endoscopy, an eroded gastric band around 2 cm below
the GEJ at 39 cm was identified. A mechanical lithotripter was then
used to break the band successfully (Figure 3). However, one position
of the band system, most likely the buckle, was embedded in the
mucosa impeding the retrieval. After multiple attempts to pull it out,
a decision to proceed with laparoscopy was taken to assess if external
adhesive bands have prevented the endoscopic retrieval. The patient
was re-positioned to split-leg supine position. Pneumoperitoneum
achieved with 12-15 mmHg using Veress needle at Palmer’s point,
and then entry to the abdominal cavity in the left supraumbilical area
using a bladeless vesi-port 10 mm and a 30-degree camera was done.
Surveillance revealed a dilated stomach and small bowel with multiple
upper quadrant adhesions to the abdominal wall and the stomach.
The gastric band tube was followed to lead to the anterior portion of
the stomach. Few adhesive-bands were released using hook cautery
which facilitated in pushing the gastric band inwards to the gastric
lumen until no further resistance was felt. The EGD was performed
simultaneously to confirm that the entire gastric band is seen free
in the stomach cavity, which was then retrieved using a snare out
of the oral cavity (Figure 4). Integrity of the stomach was confirmed through insufflations of the stomach and filling the abdominal cavity
with sterile water. No bubbles were noted intra-abdominally while
the stomach was fully distended. The gastric-band reservoir was in
the epigastric subxiphoid area, and an incision was made to extract
it. All pieces of the gastric band tube system have been extracted
successfully. The port sites were inspected which were satisfactory for
hemostasis, pneumoperitoneum was then deflated, and the wounds
closed. On post operative day 1, the patient was vitally normal and
had only mild pain over the incision sites. A barium meal fluoroscopy
was performed, and no radiological signs of leak were seen. The
patient had an uneventful postoperative course, tolerated a fluid diet
with normal bowel function. On post operative day 2, the patient
was discharged home on proton-pump inhibitors (PPI) medication
and followed up in the outpatient clinic in the following week. Upon further follow up at OPD, she reports mild symptoms of food being
impacted in the stomach and vomited a few times; otherwise, she
was doing well and tolerating oral diet. An EGD was performed as
an out-patient to assess for stricture that showed an erythematous
mucosa at high cardia in the site of previously removed band with
no stenosis or stricture. She was advised to maintain a healthy diet
and lifestyle; continue the PPI medication and she was referred to the
Adiposity Based Chronic Disease Clinic (ABCD) for further followup
regarding weight maintenance after the LAGB removal. In her 6
months follow up the patient was asymptomatic.
Discussion
Laparoscopic adjustable gastric band is a common and effective
procedure for morbid obesity. However, complications of LAGB are
not uncommon. This can include port-site infections, slippage of
the band, and band erosion. Gastric erosions after LAGB were first
reported in 1998 [4].
Gastric band erosion can present as an early or late complication.
Early erosions are usually related to the surgeon’s experience and port
site infection. Late erosions are related to port system dysfunction
and chronic ischemia. The incidence rate of gastric band erosion
ranges from 0.5% to 11% [5]. The variation in incidence rate could
be attributed to the type of the band and the surgical techniques.
Possible etiological factors of erosions are overfilling of the band
leading to gastric wall ischemia, suturing over the buckle of the band,
damage from the surgical instruments, and the dissection method.
Other causes are related to the patient’s factors including smoking,
use of NSAIDs, and consumption of alcohol.
The clinical presentation can range from asymptomatic with
incidental finding of erosion with routine endoscopy to failure to
achieve weight reduction, dysphagia, epigastric pain, and dehydration.
The erosion can be diagnosed by a CT scan. However, to confirm
the diagnosis of gastric band erosion, an upper gastrointestinal
endoscopy is needed.
Different techniques of gastric band removal have been reported in
the literature. This includes laparoscopic, endoscopic, and combined
endoscopic and laparoscopic techniques. The endoscopic technique
has proved to be successful in many cases. However, this technique
can only be done when more than 50% of the band has eroded
through the stomach and when direct visualization of the buckle is
possible. Adhesions can also limit the endoscopic retrieval of the
band. In a systematic review by Egberts et al, endoscopic removal was
not recommended because of the failure rates, the lengthy procedural
time, and the need for anesthesia and hospital admission [6].
In a case series by Chisholm et al, however, 46 cases out of 50
endoscopic retrievals were successful yielding a success rate of 92%
[7]. Similarly, Neto et al reported 82 cases of gastric band erosion with
a 95% success rate of endoscopic removal of the band [8].
Rodarte-Shade et al have described a hybrid technique for the
removal of eroded gastric bands. Adhesiolysis was done through a
laparoscopic technique. This was followed by an upper gastrointestinal
scope to visualize and remove the band trans-orally [9].
In our case, an endoscopic removal under general anesthesia was
attempted as more than 2/3 of the gastric band was visible; however, high resistance while pulling the band into the gastric lumen indicated
possible external adhesions. We proceeded to the laparoscopic
approach and found a few centimetres of the band visible and the tube
with multiple adhesions to it. After releasing the adhesions, the band
was smoothly pushed into the stomach and retrieved endoscopically.
Some of the advantages of laparoscopic-assisted endoscopic
retrieval of the band approach is to examine gastric wall integrity, to
test for leaks and to allow definitive management in that case with one
exposure to general anesthesia.
Kohn et al advocate for laparoscopic technique as this allows for
early intervention regardless of the percentage of erosion of the band
into the stomach [10].
In a retrospective review by Robinson et al that involved twentytwo
patients with gastric band erosions, one patient has undergone
a combined endoscopic and laparoscopic approach. This decision
was made based on the history of Roux-en-Y gastric bypass followed
by banding of the gastric pouch, which has undergone a combined
endoscopic and laparoscopic approach. Adhesiolysis was done and
the band was retrieved endoscopically [11].
In one case report by Spitali et al, the authors have introduced
the use of a trans-gastric single incision laparoscopic surgery for the
removal of an eroded gastric band with an uneventful postoperative
course [12]. In a video case report, the authors preferred laparoscopic
trans-gastric removal in which the band was removed through
the trocar under direct visualization using both endoscopy and
laparoscopy. The reason for this is dense scarring in the anterior wall
of the stomach [13].
A trans-gastric endoscopic rendezvous technique was described
by Karmali et al to remove an eroded Molina gastric band. This
technique was preferred because the area of dense adhesions around
the stomach can be avoided [14].
Conclusion
Laparoscopic-assisted endoscopic retrieval of the band is a safe
and an effective approach that allows to examine gastric wall integrity
and to test for leaks. It also allows a definitive management with one
exposure to general anesthesia.
Acknowledgement
Author Contributions: Kayali N and AlHabib R, reviewed the
literature and contributed to manuscript drafting; Al-Jaser W,
revision of the manuscript, the gastroenterologist who performed the
endoscopy portion of the procedure; Al Rashed A, conception and
revision of the manuscript, the surgeon who operated the laparoscopic
portion of the procedure. All authors issued final approval for the
version to be submitted.