Journal of Surgery
Download PDF
Research Article
Twenty-Year Follow-up: Multiple Arterial Grafting Is Associated with Better Outcomes for Coronary Artery Bypass Grafting Patients
Chanapong Kittayarak MD*, Panat Kittisit MD, Chalit Cheanvechai MD, Pimchanok Junnil MD, Vichai Benjacholamas MD, Seri Singhatanadgige MD, Pat Ongcharit MD and Jule Namchaisiri MD
Cardiovascular and Thoracic Surgery Unit, Department of Surgery,
King Chulalongkorn Memorial Hospital, Bangkok, Thailand
*Address for Correspondence:
Kittayarak C, Cardiovascular and Thoracic Surgery Unit, Department of
Surgery, King Chulalongkorn Memorial Hospital, Bangkok, Thailand Email:
chanapongk@hotmail.com
Submission: 07 August, 2022
Accepted: 02 September, 2022
Published: 05 September, 2022
Copyright: © 2022 Kittayarak C, et al. This is an open access article
distributed under the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided the
original work is properly cited.
Abstract
Objectives: The optimal conduits for coronary artery bypass
grafting (CABG) remain controversial in multivessel coronary artery
disease. Some studies have shown that multiple arterial conduits
offer better long-term survival. We sought to analyze the long term
outcomes of arterial graft during CABG in our institute.
Methods: Retrospective cohort analyses of all patients undergoing
primary isolated CABG in King Chulalongkorn Memorial Hospital,
Bangkok, Thailand, from January 1997 – December 2001. We stratified
patients into three groups including patients with multiple arterial graft
(MAG) versus single arterial graft (SAG) versus non-arterial graft (NAG).
The primary outcome was survival rate. The secondary outcome was
time to first event of a composite of death, MI, stroke, and repeat
revascularization (major adverse cardiac and cerebrovascular events,
MACCE).
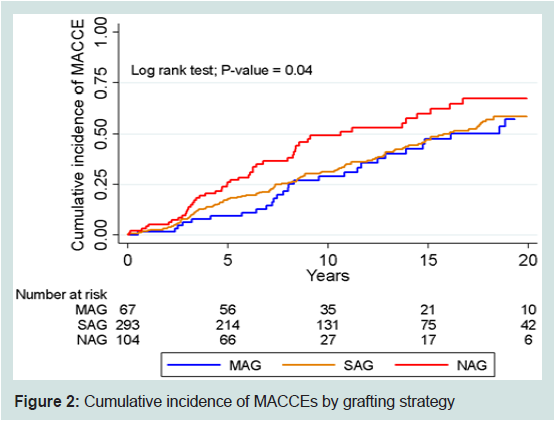
Results: Four hundred sixty four patients underwent isolated CABG
during our study period; 67 patients (14.4%) in multiple arterial graft
group (MAG), 293 patients (63.1%) in single arterial graft group (SAG)
and 104 patients (22.5%) in non-arterial graft group (NAG). Mean and
maximum follow-up was 12.5 and 24.5 years, respectively. Median age
of population is 63 years (IQR 56-69) with 60 years in MAG, 63 years in
SAG and 66 years in NAG (P < 0.001).Most common second arterial
conduit is radial artery grafting, accounting for 76 patients (16.4%). Other
baseline characteristics are not different between groups. In-hospital
mortality was 0% for MAG vs 1.7% in SAG and 5.8% in NAG (P = 0.04). On
the other hand, 20-year survival of MAG, SAG and NAG is 52.9%, 44.3%
and 23.7%, respectively. At 20 years, incidences of MACCE, survival,
repeat revascularization, and myocardial infarction were inferior in
multiple arterial groups. The risk factors associated with death were
non-arterial graft, age more than 60 years, low BMI, diabetic mellitus,
renal dysfunction, pre-operative IABP, cardiopulmonary bypass time
more than 75 minutes and postoperative atrial fibrillation.
Conclusion: CABG with multiple arterial grafts was associated with
better clinical outcomes compare with single and non-arterial graft at
20-year follow-up.
Introduction
For a long time, coronary artery disease has been a leading cause of
death worldwide which kills more than 3, 00,000 people per year. Up
until now, there are many scientific evidences proving that coronary
artery revascularization improves survival and reduces incidence of
major adverse cardiac events (MACEs) [1]. There are two principal
methods of coronary revascularization including coronary artery
bypass grafting (CABG) and percutaneous coronary intervention
(PCI). It has been shown in many studies that CABG offers
advantages over PCI in patients with complex coronary anatomy especially in diabetic patients [2,3]. CABG needs conduits to bypass
the stenotic coronary lesion which were shown in many studies that
multiple arterial conduits offer better long-term outcome compared
with single arterial and venous conduits [4-7]. However, these studies
investigated mainly in western population and very little of them
follow-up more than ten years. Our study took place in a tertiary care
hospital in Thailand with twenty-year follow-up aiming to compare
survival and incidence of major adverse cardiac or cerebrovascular
events (MACCEs) in patients who underwent coronary artery bypass
grafting with different types of conduits application.
Methods
The study population was derived from all consecutive patients
who underwent primary isolated CABG in King Chulalongkorn
Memorial Hospital, Bangkok, Thailand from January 1, 1997 to
December 31, 2001. Inpatient, outpatients, emergency department
and operative records were retrospectively reviewed. Patients who
lost follow-up were telephone follow-up by investigators. Inclusion
criteria were patients who underwent primary isolated CABG
with any graft configuration. Exclusion criteria were patients who
underwent redo CABG, non-isolated CABG (combined with valve
or aortic operation) and incomplete data of grafting strategy. The
primary outcome of this study is twenty-year survival. The secondary
outcome is incidence of major adverse cardiac and cerebrovascular
events (MACCEs). The study was approved by the Institutional
Review Board of the faculty of Medicine, Chulalongkorn University,
Bangkok, Thailand in compliance with the international guidelines
for human research protection as Declaration of Helsinki, The
Belmont Report, CIOMS Guideline and international Conference on
Harmonization in Good Clinical Practice (ICH-GCP).
Preoperative demographic data including sex, age, BMI,
preoperative hematocrit, angina grading (Canadian Cardiovascular
Society, CCS), Dyspnea grading (New York Heart Association,
NYHA), history of congestive heart failure (CHF) and myocardial
infarction (MI), underlying disease, coronary lesion and left
ventricular function were collected. Intraoperative data including
grafting strategy, urgency of operation, mechanical support necessity,
cardioplegia delivery strategy, cardiopulmonary bypass (CPB) and aortic cross-clamp time were collected. Postoperative course data
including complications, length of stay (LOS) and ICU stay were
collected. Follow-up data including all-cause death, incidence of
MACCEs were collected. In patients who underwent re-coronary
angiography due to any indication, the patency of grafts was also
reviewed.
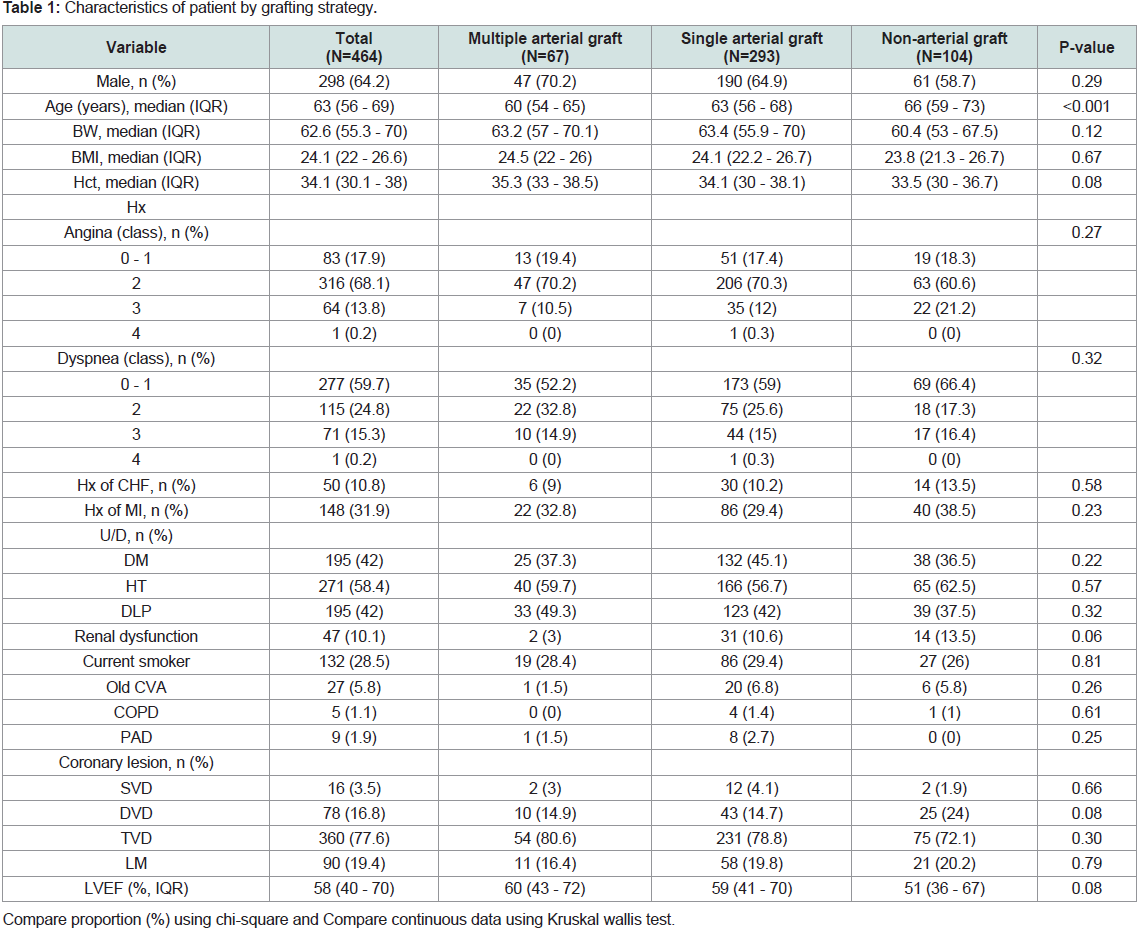
There were 464 patients who met the inclusion criteria. Their
preoperative demographic data were demonstrated in Table 1.
Patients were classified as multiple arterial graft group (MAG) if they
were grafted with two or more arterial conduits, single arterial graft
group (SAG) if they were grafted with one arterial conduit and nonarterial
graft group (NAG) if no arterial conduit was used.
Stata version 15.1 (Stata Corp., College Station, Texas), was
used for analysis. Continuous variables are expressed as median
(interquartile range: IQR) and percentage for categorical variables.
Differences in continuous and categorical variables between three
groups were assessed using a Kruskal Wallis test and Chi-square
test or fisher exact test, respectively. The survival rate and incidence
of MACCEs were calculated by Kaplan Meier and log rank test for comparison between groups. The Cox regression was used to
determine the factors associated with mortality and incidence of
MACCEs. Multivariate models were developed by adjusting for
covariates with p < 0.1 in univariate models to determine risk factors
associated with mortality and using stepwise backward LR for
incidence of MACCEs. All P-values reported are two-sided. Statistical
significance was defined as P < 0.05.
Results
There were 67 (14.4%) patients in MAG, 293 (63.1%) patients in
SAG and 104 (22.5%) patients in NAG with male predominant in
each group but not statistically significant between groups (P = 0.29).
The median age of population is 63 years (IQR 56-69) with 60 years
(IQR 54-65) in MAG, 63 years (IQR 56-68) in SAG and 66 years (IQR
59-73) in NAG (P < 0.001). Most patients (381 in 464, 82.1%) have
trouble with angina symptoms predominantly class II CCS (82.9%).
198 patients (42.7%) have a history of hospitalization with congestive
heart failure or acute coronary syndrome. Most patients have triple
vessel disease (360 in 464, 77.6%). Median preoperative LVEF is 58%
(IQR 40-70) (Table 1).
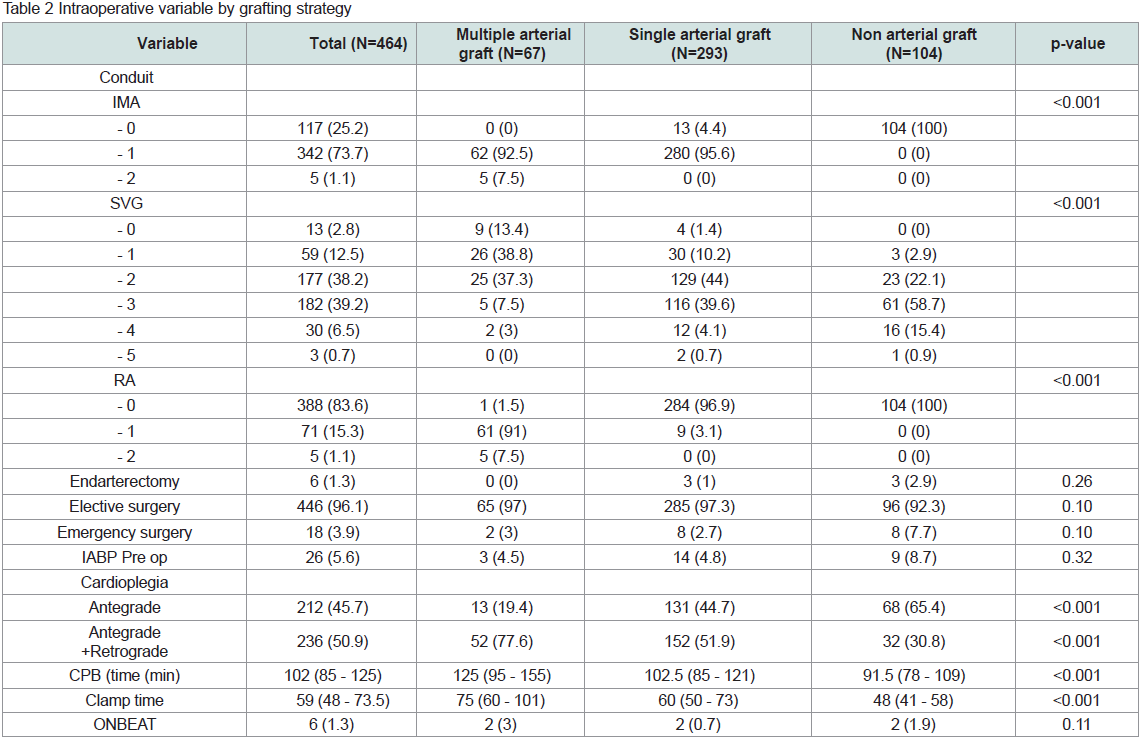
Intraoperative data were listed in Table 2. In MAG, left internal
thoracic artery (LITA) grafted to left anterior descending artery
(LAD) was used in all 67 patients with 5 patients (1.1%) underwent
bilateral internal thoracic artery (BITA) grafting. Radial artery (RA)
was used in 76 patients (16.4%). Bilateral radial artery was used in
4 patients with 1 patient underwent bilateral radial artery grafted
to three coronary targets (left radial artery grafted to two obtuse
marginal arteries sequentially and right radial artery grafted to
posterior descending artery). No gastroepiploic artery was used in
any patient. In SAG, 280 patients (95.6%) underwent LITA grafted to
LAD. Coronary endarterectomy was done in 6 patients (1.3%) with 3
patients in SAG and 3 patients in NAG. There were 18 patients (3.9%)
who underwent emergency operation and 26 patients (5.6%) needed
a preoperative intra-aortic balloon pump (IABP). Median CPB time
was 102 minutes (IQR 85 - 125) with 125 minutes (IQR 95 - 155) in
MAG, 102.5 minutes (IQR 85 - 121) in SAG and 91.5 minutes (IQR
78 - 109) in NAG (P < 0.001). Median aortic cross-clamp time was 59
minutes (IQR 48 - 73.5) with 75 minutes (IQR 60 - 101) in MAG, 60
minutes (IQR 50 - 73) in SAG and 48 minutes (IQR 41 - 58) in NAG
(P < 0.001).
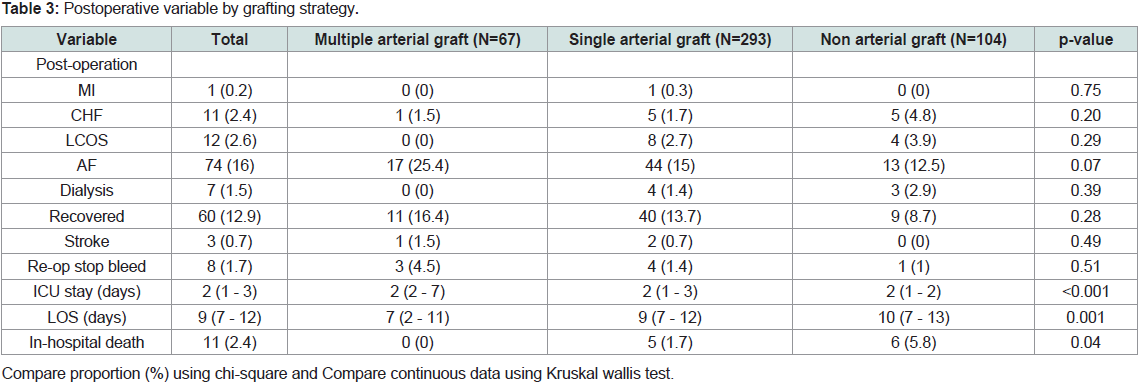
Postoperative myocardial infarction occurred in one patient
(0.2%) in SAG, the coronary angiography showed stenosis at
anastomosis of LITA to LAD and the patient underwent anastomosis
revision successfully. CHF and low cardiac output syndrome (LCOS)
occurred in 23 patients (5%). Postoperative atrial fibrillation (AF)
occurred in 74 patients (16%). There was renal dysfunction in 67 patients (14.4%) which 89% recovered before discharge. In-hospital
mortality occurred in 11 patients (2.4%) (Table 3).
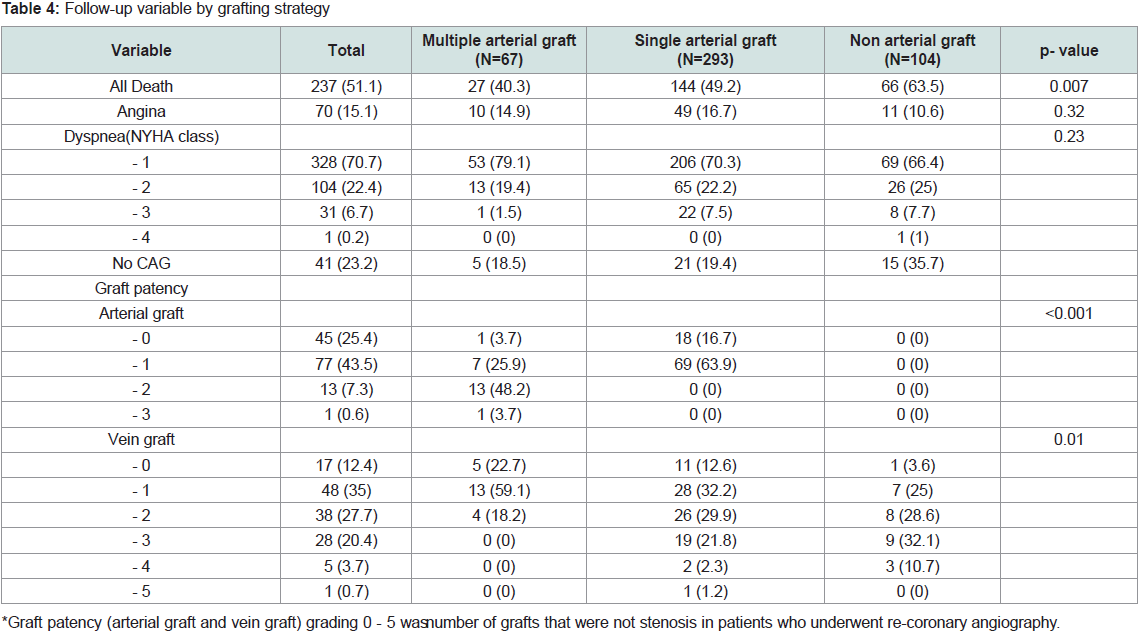
During 20-year follow-up, mortality occurred in 237 patients
(51.1%) with 27 patients (40.3%) in MAG, 144 patients (49.2%) in
SAG and 66 patients (63.5%) in NAG (P < 0.007) (Table 4).
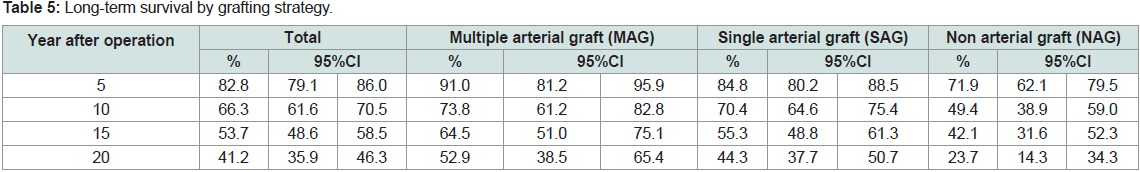
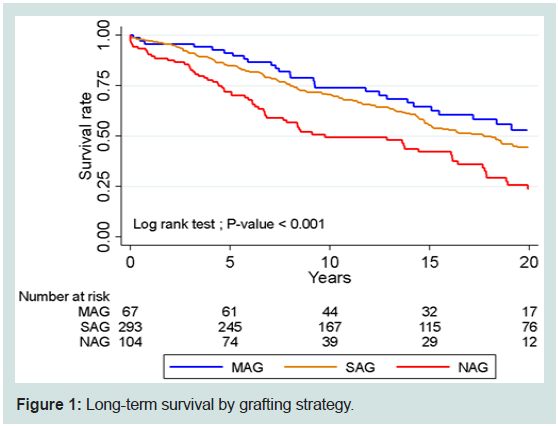
In MAG, survival at 5,10, 15, 20 years were 91%, 73.8%, 64.5%
and 52.9%, respectively. Survival at 5, 10, 15, 20 years were 84.8%,
70.4%, 55.3% and 44.3%, respectively in SAG. In NAG, survival at
5, 10, 15, 20 years were 71.9%, 49.4%, 42.1% and 23.7%, respectively
(Table 5, Figure 1).
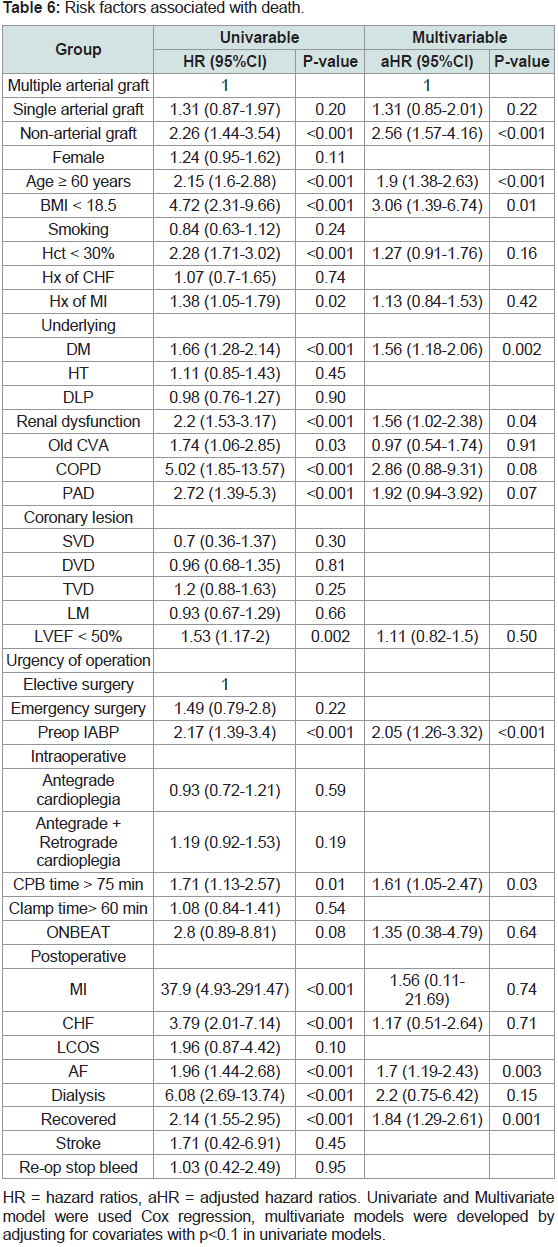
In univariate analysis, risk factors associated with death were
non-arterial graft (HR = 2.26; 95% CI 1.44 - 3.54, P < 0.001), age
60 years (HR = 2.15; 95% CI 1.6 - 2.88, P < 0.001), BMI < 18.5 kg/m2
(HR = 4.72; 95% CI 2.31 - 9.66, P < 0.001), Hematocrit < 30% (HR =
2.28; 95% CI 1.71 - 3.02, P < 0.001), history of MI (HR = 1.38; 95%
CI 1.05 - 1.79, P = 0.02), diabetes mellitus (HR = 1.66; 95% CI 1.28 -
2.14, P < 0.001), renal dysfunction (HR = 2.2; 95% CI 1.53 - 3.17, P <
0.001), old CVA (HR = 1.74; 95% CI 1.06 - 2.85, P = 0.03), COPD (HR
= 5.02; 95% CI 1.85 - 13.57, P < 0.001), PAD (HR = 2.72; 95% CI 1.39
- 5.3, P < 0.001), LVEF < 50% (HR = 1.53; 95% CI 1.17 - 2, P = 0.002),
preoperative IABP (HR = 2.17; 95% CI 1.39 - 3.4, P < 0.001), CPB
time > 75 min (HR = 1.71; 95% CI 1.13 - 2.57, P = 0.01), postoperative
MI (HR = 37.9; 95% CI 4.93 - 291.47, P < 0.001), postoperative CHF
(HR = 3.79; 95% CI 2.01 - 7.14, P < 0.001), postoperative AF (HR =
1.96; 95% CI 1.44 - 2.68, P < 0.001), postoperative renal dysfunction
(HR = 2.14; 95% CI 1.55 - 2.95, P < 0.001). Route of cardioplegia including antegrade or antergrade combined with retrograde were
not statistically significant risk factors associated with death. After
multivariate analysis, the risk factors associated with death were nonarterial
graft (HR = 2.56; 95% CI 1.57 - 4.16, P < 0.001), age 60
years (HR = 1.9; 95% CI 1.38 - 2.63, P < 0.001), BMI < 18.5 kg/m2
(HR = 3.06; 95% CI 1.39 - 6.74, P = 0.01), diabetes mellitus (HR =
1.56; 95% CI 1.18 - 2.06, P = 0.002), renal dysfunction (HR = 1.56;
95% CI 1.02 - 2.38, P = 0.04), preoperative IABP (HR = 2.05; 95% CI 1.26 - 3.32, P < 0.001), CPB time (HR = 1.61; 95% CI 1.05 - 2.47, P
= 0.03), postoperative AF (HR = 1.7; 95% CI 1.19 - 2.43, P = 0.003),
postoperative renal dysfunction (HR = 1.84; 95% CI 1.29 - 2.61, P =
0.001) (Table 6).
Discussion
Since the invention of CABG in the 1960s, a number of studies
have proved us that CABG improves survival of patients with
coronary artery disease. Most contemporary evidence showed a
trend toward better results with arterial conduit, especially total
arterial revascularization. An internal thoracic artery, especially
left, grafted to LAD has been a standard configuration to improve
patient’s survival. Also, radial artery is a recommended conduit
utilized to graft the second most important non-LAD coronary target
[8]. The guideline of coronary artery bypass grafting also recommend
multiple arterial grafting especially in younger patients as the conduit patency is compatible with patients’ life expectancy [9]. Despite
having more benefit in straightforward cases, arterial conduits have
some drawbacks in emergency situation and in patients with poor
LV function since arterial spasm may hinder the conduits from
providing immediate coronary revascularization. Also, there are
some challenges when grafting arterial conduits on non-critical
stenotic coronary targets because of the competitive flow [10]. On
the other hand, saphenous vein grafts have low propensity for spasm
and can provide immediate coronary flow. Besides, in patients with
severe co morbidities and limited life expectancy, saphenous vein
grafts offer a simpler procedure and a shorter operative time. Most of
this knowledge derived from western centers where most of the study
population is Caucasian. Whether the smaller stature and smaller
vessels, especially arteries, of Asians impede the benefit of arterial
graft over vein graft is one of the motivations of our study [11]. The
purpose of this study was to determine the long-term outcome up to
twenty years of multiple arterial grafting, single arterial grafting and
non-arterial grafting.
In our study, the median age of population is 63 years with male
predominate, the most common coronary pathology is triple vessels
disease and mean LVEF is around 50% which is comparable to other
studies [4,7,12,13]. The survival at 5, 10, 15 and 20 years of MAG in our
data is 91%, 73.8%, 64.5% and 52.9%, in SAG is 84.8%, 70.4%, 55.3%,
44.3% and in NAG is 71.9%, 49.4%, 42.1% and 23.7%, respectively.
These may be implied that the more arterial graft, the more survival
benefit. Nevertheless, we did not compare multiple arterial grafts in
subgroup of two, three or more arterial graft due to small number of
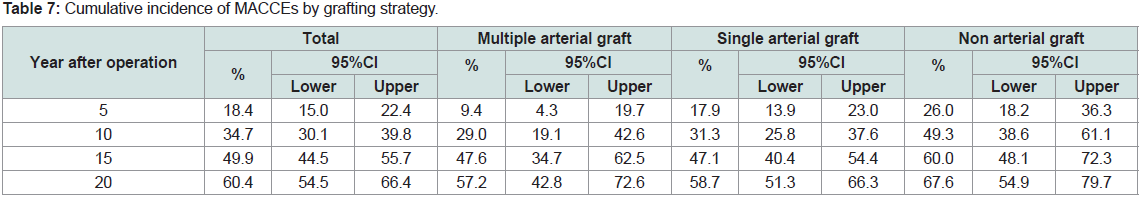
patients in each subgroup. The cumulative incidence of MACCEs at
5, 10, 15 and 20 years in our cohort is 9.4%, 29%, 47.6% and 57.2%
in MAG, 17.9%, 31.3%, 47.1% and 58.7% in SAG and 26%, 49.3%,
60% and 67.6% in NAG, respectively. These may suggest the benefit
of second arterial graft, mostly radial artery, in the first 10 years after
operation and the benefit of LITA grafted to LAD that last up to 20
years after operation. Rocha and colleagues reported the survival at 5,
8 years of MAG to be 91.3%, 83.6% and 89.3%, 80.3% in SAG which
are comparable with our study [5]. They also reported the cumulative
incidence of MACCEs at 5, 8 years to be 17.5%, 27.4% in MAG and
21.4%, 32.5% in SAG which is more than ours. The reason of fewer
incidences of MACCEs at 5 years of our study may be due to less
BMI and less incidence of PAD in our population. The survival and
MACCEs in the report of Parasca and colleagues are also on par with
Rocha’s [12]. Although there was a trend toward more satisfactory
survival outcome of MAG than SAG in our study, this was not
account to statistically significant as shown in both univariate and
multivariate analysis. This may be due to not large enough sample
size or not long enough follow-up as Kaplan-Meier graphs of MAG
and SAG are slowly apart from each other as the time goes by. In
our study, most of the second arterial conduit is radial artery. When
compared to data from RAPCO trial (RAPCO-SV) which reported 10
years survival of RA group to be 72.6% [14], 10 years survival of MAG
in our study is 73.8% corresponding to that of RAPCO. The objection
is that the mean age of population in RAPCO-SV is 72.6 years which
is older than ours. On the other hand, in RAPCO-RITA (mean age of
RA arm is 59.2 years), the 10 years survival of RA arm is reported to
be 90.9% which is better than ours. These may be explained by much
fewer diabetic patients (11% vs 37.3%) in RA arm in RAPCO-RITA
and smaller RA size of Asians as our concern in the first place [11]. In both univariate and multivariate analysis of our study also showed
diabetes to be risk factor of death. From our intraoperative data,
combined antegrade and retrograde cardioplegia delivery technique
was used more in MAG than SAG and NAG. We believed that these
were due to surgeon preference. CPB time and aortic cross clamp
time were also longest in MAG. All of these factors did not account
for death or MACCEs in multivariate analysis except CPB time which
was a risk factor for death but not MACCEs.
There were some limitations of our study. First, it was a
retrospective cross-sectional analysis which may be confounded by
selection bias. Second, the study population was quite small when
compared to the other previous cohort [4,5,12,13]. Third, the operative
outcomes may be partly related to operative techniques which have
been fine-tuned over time. Finally, the conduit selected for bypass
may be biased by coronary target and patients’ comorbidities such as
patients with severe comorbidities, limited life expectancy and poor
coronary target may be grafted by saphenous vein.
Conclusion
Multiple arterial grafting is associated with better twenty-year
survival compared with single arterial grafting and non-arterial
grafting. The cumulative incidence of MACCEs is also higher in
patients who underwent CABG with single arterial grafting and nonarterial
grafting.