Journal of Toxins
Download PDF
Case Report
*Address for Correspondence: Lu-Qing Wei, Department of Respiratory and Critical Care Medicine of Pingjing Hospital, Affiliated Hospital of Logistic University of Chinese People’s Armed Police Force, 220#, Cheng-Lin Road, Tianjin, 300162, China, Tel: +86-022-60578941; Fax: +86-022-60578671; E-mail: sunlaingys@sina.com
Citation: Sun L, Li G, Zhang Y, Dong H, Wei L. What Should We Do After Acute Organophosphorus Pesticide Poisoning During Pregnancy?. J Toxins.2015;2(2): 3
Copyright © 2015 Sun L, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Toxins | ISSN: 2328-1723 | Volume: 2, Issue: 2
Submission: 13 August, 2015 | Accepted: 23 November, 2015 | Published: 27 November, 2015
Facing these diverse outcomes, it is difficult to draw any final and firm conclusion from these studies. However, what should we do after AOPP during pregnancy? Perhaps the best way is to establish an international register (e.g. through WHO or Poison Center/ Organisation) in which all exposures (accidental and intentional) can be recorded. And long-term follow-up of neonates of human are required to find out whether a healthy baby can be delivered after AOPP during pregnancy. This will allow a more detailed and complete database from which advice can be retrieved.
What Should We Do After Acute Organophosphorus Pesticide Poisoning During Pregnancy?
Liang Sun1, Guo-qiang Li1,Yu-hua Zhang1, Huajiang Dong2 and Lu-qing Wei1*
- 1Department of Respiratory and Critical Care Medicine of Pingjing Hospital, Affiliated Hospital of Logistic University of Chinese People’s Armed Police Force, 220#, Cheng-Lin Road, Tianjin, 300162, China
- 2Logistic University of Chinese People’s Armed Police Force, 1#, Hui ZHi Huan Road, Tianjin, 300309, China
*Address for Correspondence: Lu-Qing Wei, Department of Respiratory and Critical Care Medicine of Pingjing Hospital, Affiliated Hospital of Logistic University of Chinese People’s Armed Police Force, 220#, Cheng-Lin Road, Tianjin, 300162, China, Tel: +86-022-60578941; Fax: +86-022-60578671; E-mail: sunlaingys@sina.com
Citation: Sun L, Li G, Zhang Y, Dong H, Wei L. What Should We Do After Acute Organophosphorus Pesticide Poisoning During Pregnancy?. J Toxins.2015;2(2): 3
Copyright © 2015 Sun L, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Toxins | ISSN: 2328-1723 | Volume: 2, Issue: 2
Submission: 13 August, 2015 | Accepted: 23 November, 2015 | Published: 27 November, 2015
Abstract
A 25-year-old married primigravida was admitted to Pingjin Hospital after ingestion of dichlorvos, with suicidal intent. The initial serum dichlorvos level was 1.7 umol/L, with a reduction in cholinesterase activity of 29% in whole blood. Abdominal investigation revealed a soft abdomen with a pregnant uterus consistent with 9th week of gestation on echography and with a viable fetus. The patient was discharged from hospital with successful treatment of both mother and neonate after 10 days of treatment. However, we cannot confirm whether dichlorvos poisoning will affect the brain development of the fetus. Subsequently, she made an artificial abortion for fear of adverse fetal outcome four weeks later after intoxication.Keywords
Organophosphates poisoning; Fetal development; PregnancyIntroduction
Organophosphates (OPs) are widely used insecticides, but still presents a serious health threaten. According to a report by the World Health Organization (WHO), up to 3,000,000 people worldwide are affected by pesticide poisoning each year, with acute organophosphate pesticide poisoning (AOPP) being the most common type [1]. AOPP is fairly common in rural areas of China [2]. It is seen in almost all types of population affecting both male and female. Accordingly, it can occur in women of reproductive age, including those pregnant. However, exposure to OP in pregnancy poses problems for both mother and fetus because of placental transfer of OP compounds [3].Treatment of OPs poisoning in pregnancy and the potential developmental effects of OPs exposures to the developing fetus and child has been studied for several decades. However, these issues still have not been adequately resolved and have no satisfactory answers. One of the important questions yet to be answered is whether a healthy baby can be delivered when pregnant women with AOPP managed successful without mother and fetal death. In this paper, we described one case of AOPP during pregnancy with successful treatment of both mother and neonate. However, the mother made an artificial abortion four weeks later after intoxication because not sure whether dichlorvos poisoning will affect the brain development of the fetus.
Case Report
A 25-year-old married primigravida was admitted to the Pingjin Hospital, Affiliated Hospital of Logistics university of Chinese people’s armed police force, 5 h after ingestion of dichlorvos, with suicidal intent. The initial serum dichlorvos level was 1.7 umol/L, with a reduction in cholinesterase activity of 29% in whole blood. Quantitative analysis of the initial serum dichlorvos level was conducted in the hospital laboratory by a gas chromatography method [4]. Clinical examination revealed a fully conscious patient, well-oriented and with mild salivation. Abdominal investigation revealed a soft abdomen with a pregnant uterus consistent with 9th week of gestation on echography and with a viable foetus. Fetal heart rate was monitored and showed no significant abnormality. Treatment included activated charcoal hemoperfusion therapy, gastric lavage, Penehyclidine hydrochloride (PHC) and pralidoxime chloride. The regimen of injection of PHC as follows: 4 mg of PHC was given intramuscular as a first dose, then 2 mg of PHC was given intramuscular every 8 h until muscarinic symptoms were relieved. It was continued until the tracheo-bronchial tree was cleared of the secretions and most secretions were dried. Then the dose was adjusted to maintain this effect until the cholinesterase activity of the whole blood increased 65%. When the first 2 intravenous injections of 1.0 g of pralidoxime chloride are not satisfactory, continuous infusion at rates up to 1 g per hour. After 5 days of treatment, the cholinesterase activity of the whole blood increased 100%. Then she was transported to the maternity ward to continue treatment. The patient was discharged from hospital with good general condition after 10 days of treatment, the fetal heart rate also showed normal. Before discharging from hospital, she wants to know that whether the fetal growth could be affected by the OP poisoning and whether a healthy baby can be delivered? However, facing these problems, we can’t give him a firm answer. Then, she made an artificial abortion for fear of adverse fetal outcome four weeks later after intoxication. However, the patient refused to check for the post-abortion fetus, we could not get any medical information of the fetus.Discussions
Whether a healthy baby can be delivered when pregnant women with AOPP managed successful without mother and fetal death is still a matter of debate. The key determinant of the answer is whether prenatal OP exposure can affect fetal development. Epidemiologic studies in humans on the subject have shown conflicting results [5-8]. However, these conflicting results are about the effect of low OP exposure upon birth weight, length and head circumference of the infants.OPs are well-known acute neurotoxicants, which inhibit acetylcholinesterase, resulting in the buildup of acetylcholine in neuronal junctions [9]. Ecologic studies have implicated a link between pesticide exposure and impaired neurodevelopment [10,11]. Developmental neurotoxicity studies have also been shown that prenatal exposure to OP pesticides may be associated with an increased risk of pervasive developmental disorders, delays in cognitive development and attentional deficits [12-14]. These developmental neurotoxicity also associated with the level of OP pesticide which prenatal and early childhood exposure to [15]. These studies suggest that prenatal exposure to OPs may disrupt brain development in the developing nervous system.Furthermore, numerous studies were conducted in animals to evaluate the potential effect of OPs exposures, including on neurologic development. Experiments indicate that young animals being more sensitive to the effects of OPs exposure [16,17]. Therefore, animals’ in utero experiencing OPs exposure may decrease balance [18], increase righting reflex time and poorer cliff avoidance [19].
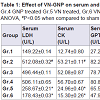
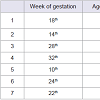
However, reviewed human of literature suggests that the majority of the pregnant women, who survived the acute phase of AOPP, had an uneventful pregnancy and had a good fetal outcome. Table 1 summarizes the study characteristics of case reports [20-26]; Table 2 summarizes the study characteristics of K. Adhikari [27]. As can be seen from these clinical data, the poisoning cases occurred in different stage of pregnancy and the majority of the women who survived the acute phase of poisoning had an uneventful pregnancy and had a good fetal outcome. With all the clinical data available up to now, it looks like that AOPP did not change the course of pregnancy nor did it damage the fetus. However, the study population was small and the severity of most poisoning cases is unclear. Especially in some cases, the types and classes of OPs are unclear. Furthermore, the instruments used to assess the outcomes of neonates are just Apgar score and weight, long-term follow-up of neonates was also lacking in all study population.
Facing these diverse outcomes, it is difficult to draw any final and firm conclusion from these studies. However, what should we do after AOPP during pregnancy? Perhaps the best way is to establish an international register (e.g. through WHO or Poison Center/ Organisation) in which all exposures (accidental and intentional) can be recorded. And long-term follow-up of neonates of human are required to find out whether a healthy baby can be delivered after AOPP during pregnancy. This will allow a more detailed and complete database from which advice can be retrieved.
Ethical Statement
The patient was given written information and a verbal explanation concerning the study prior to obtaining the written informed consent for his participation. Prior to commencement of the study, the patient was fully informed and signed an informed consent document.References
- Cavaliere MJ, Puga FR, Calore EE, Calore NM, Pelegrino JR, et al. (1998) Protective effect of pralidoxime on muscle fiber necrosis induced by organophosphate compounds. J Toxicol Clin Toxicol 36: 295-300.
- Zhang L, Hao L, Zhang X, Chen J, Wang Q, et al. (2015) Pidemiological analysis of pesticide poisoning in hangzhou during 2006-2013. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 33: 38-40.
- Bradman A, Barr DB, Claus Henn BG, Drumheller T, Curry C, et al. (2003) Measurement of pesticides and other toxicants in amniotic fluid as a potential biomarker of prenatal exposure: a validation study. Environ Health Perspect 111: 1779-1782.
- Rodziewicz L, Moniuszko-Jakoniuk J (1986) Determining methyl parathion level in the blood serum using a gas chromatography method. Rocz Panstw Zakl Hig 37: 430-433.
- Whyatt RM, Rauh V, Barr DB, Camann DE, Andrews HF, et al. (2004) Prenatal insecticide exposures and birth weight and length among an urban minority cohort. Environ Health Perspect 112: 1125-1132.
- Eskenazi B, Harley K, Bradman A, Weltzien E, Jewell NP, et al. (2004) Association of in utero organophosphate pesticide exposure and fetal growth and length of gestation in an agricultural population. Environ Health Perspect 112: 1116-1124.
- Harley KG, Huen K, Aguilar Schall R, Holland NT, Bradman A, et al. (2011) Association of organophosphate pesticide exposure and paraoxonase with birth outcome in Mexican-American women. PLoS One 6: e23923.
- Barr DB, Ananth CV, Yan X, Lashley S, Smulian JC, et al. (2010) Pesticide concentrations in maternal and umbilical cord sera and their relation to birth outcomes in a population of pregnant women and newborns in New Jersey. Sci Total Environ 408: 790-795.
- Ahlbom J, Fredriksson A, Eriksson P (1995) Exposure to an organophosphate (DFP) during a defined period in neonatal life induces permanent changes in brain muscarinic receptors and behaviour in adult mice. Brain Res 677: 13-19.
- Young JG, Eskenazi B, Gladstone EA, Bradman A, Pedersen L, et al. (2005) Association between in utero organophosphate pesticide exposure and abnormal reflexes in neonates. Neurotoxicology 26: 199-209.
- Kofman O, Berger A, Massarwa A, Friedman A, Jaffar AA (2006) Motor inhibition and learning impairments in school-aged children following exposure to organophosphate pesticides in infancy. Pediatr Res 60: 88-92.
- Ruckart PZ, Kakolewski K, Bove FJ, Kaye WE (2004) Long-term neurobehavioral health effects of methyl parathion exposure in children in Mississippi and Ohio. Environ Health Perspect 112: 46-51.
- Rohlman DS, Arcury TA, Quandt SA, Lasarev M, Rothlein J, et al. (2005) Neurobehavioral performance in preschool children from agricultural and non-agricultural communities in Oregon and North Carolina. Neurotoxicology 26: 589-598.
- Grandjean P, Harari R, Barr DB, Debes F (2006) Pesticide exposure and stunting as independent predictors of neurobehavioral deficits in Ecuadorian school children. Pediatrics 117: e546-556.
- Eaton DL, Daroff RB, Autrup H, Bridges J, Buffler P, et al. (2008) Review of the toxicology of chlorpyrifos with an emphasis on human exposure and neurodevelopment. Crit Rev Toxicol 38 Suppl 2: 1-125.
- Pope CN, Liu J (1997) Age-related differences in susceptibility to organophosphorus pesticides. Environ Toxicol Pharmacol 4: 309-314.
- Vidair CA (2004) Age dependence of organophosphate and carbamate neurotoxicity in the postnatal rat: extrapolation to the human. Toxicol Appl Pharmacol 196: 287-302.
- Muto MA, Lobelle F Jr, Bidanset JH, Wurpel JN (1992) Embryotoxicity and neurotoxicity in rats associated with prenatal exposure to DURSBAN. Vet Hum Toxicol 34: 498-501.
- Chanda SM, Pope CN (1996) Neurochemical and neurobehavioral effects of repeated gestational exposure to chlorpyrifos in maternal and developing rats. Pharmacol Biochem Behav 53: 771-776.
- Solomon GM, Moodley J (2007) Acute chlorpyrifos poisoning in pregnancy: a case report. Clini Toxicol (Phila) 45: 416-419.
- Karalliedde L, Senanayake N, Ariaratnam A (1998) Acute organophosphorus insecticide poisoning during pregnancy. Hum Toxicol 7: 363-364
- Weis OF, Müller FO, Lyell H, Badenhorst CH, van Niekerk P (1983) Materno-fetal cholinesterase inhibitor poisoning. Anesth Analg 62: 233-235.
- Kamha AA, Al Omary IY, Zalabany HA, Hanssens Y, Adheir FS (2005) Organophosphate poisoning in pregnancy: a case report. Basic Clin Pharmacol Toxicol 96: 397-398.
- Sebe A, Satar S, Alpay R, Kozaci N, Hilal A (2005) Organophosphate poisoning associated with fetal death: a case study. Mt Sinai J Med 72: 354-356.
- Jajoo M, Saxena S, Pandey M (2010) Transplacentally acquired organophosphorus poisoning in a newborn: case report. Ann Trop Paediatr 30: 137-139.
- Carrington da Costa RB, Maul ER, Pimentel J, Gonçalves JS, Rebelo A, et al. (1982) A case of acute poisoning by methyl demeton in a female 5 months pregnant. Arch Toxicol Suppl 5: 202-204.
- Adhikari K, Ghosh A, Alauddin MD, Moitra A, Datta AK (2011) Organophosphate poisoning in pregnancy. J Obstet Gynaecol 31: 290-292.