Journal of Urology & Nephrology
Download PDF
Research Article
Comparison of Endoscopic Injection of Vantris and Gil-Vernet surgery in the Treatment of Primary Vesicoureteral Reflux (VUR)
Rashed FK, Roshandel MR*, Aghaei Badr T and Motlagh RS
Department of Urology, Tabriz University of Medical Sciences, Iran
*Address for Correspondence: Roshandel MR, Department of Urology, Imam Reza hospital, Tabriz
University of medical sciences, Golgasht Street, Tabriz, Iran; E-mail: roshandelmr@yahoo.com
Submission: 18 June, 2019
Accepted: 14 August, 2019
Published: 17 August, 2019
Copyright: © 2019 Rashed FK, et al. This is an open access article
distributed under the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited.
Abstract
Purpose: Vesicoureteral Reflux (VUR) is the most common urologic
condition in pediatric population, affecting almost 1% of children. The
present study aims to compare outcomes of an open surgical technique
(Gil-Vernet), an old-fashioned method still performed in some centers,
and the endoscopic correction using Vantris as a preferred less invasive
method in children with VUR.
Materials and methods: In this randomized clinical trial, a total of 61
children with VUR of grades I-IV underwent either open surgical repair
using the Gil-Vernet approach (30 patients, 50 renal refluxing units), or
endoscopic repair using Vantris as the bulking agent (31 patients, 49 renal
refluxing units). The change in VUR grade before and after operation was
compared between the two groups.
Results: The Vantris group comprised 5 males and 26 females with
the mean age of 6.15±2.26 years (range, 1-10) versus the Gil-Vernet that
included 9 males and 21 females with the mean age of 5.23±2.05 years
(range, 1-10) (p=0.20 and 0.21, respectively). The VUR grade decreased
significantly in both groups after operation (p<0.001), but despite a better
improvement in the Vantris patients the inter-group analysis missed a
statistically significant level in a marginal fashion (p=0.07). The rate of
improvement and full improvement was 98% and 81.6% in the Vantris
group vs. 94% and 86% in the Gil-Vernet group, respectively (p=0.62 and
0.56, respectively).
Conclusion: Although postoperative improvement in VUR grade
was better in the Vantris® group than that in the Gil-Vernet group, the
difference was not statistically significant. Both methods of treatment were
safe and with a high rate of success. Nevertheless, lesser manipulations
performed in Vantris® makes it favorable comparing with open Gil-Vernet
method.
Abbreviations
VUR: Vesico-Ureteral Reflux
Introduction
Vesicoureteral Reflux (VUR), the return of the urine from bladder
to the ureter, is an anatomic or functional abnormality[1]. The
treatment goal is to preserve renal function by reducing the risk of
infection and renal scarring[1,2]. But desirable treatment of VUR is
controversial. Open anti-reflux surgery is the treatment of choice for
severe cases [3]. Gil-Vernet Open surgery is an intravesicular surgical
procedure, in which the intramural length of ureter is increased
with medial advancement and increasing the muscle support [4].
This technique is performable in unilateral and bilateral cases [5],
is simple, and is associated with few complications [6]. It seems
that Gil-Vernet trigonoplasty is one of the open procedures, which
is less invasive, simple, has a high success rate, has the advantage
of feasibility of future ureteroscopy with less problems, and is also
performable on outpatient basis [5]. The advantages of endoscopic
methods include the feasibility to be performed on outpatient basis, short duration of the procedure, short hospital stay, low cost,
minimally invasiveness and lack of common complications of open
surgery [3]. Various substances have been proposed to be injected,
including Teflon, collagen, patient’s own fat (autologous), poly-dimethylene
silocan, silicon, chondrocytes and deflux (dextranomer/
hyaluronic acid solution). In the meantime, the best results have
been reported in Teflon injection, but because of the small size of the
particles and concerns about displacement and migration of particles
to the neighboring areas and other organs, such as lungs, brain, and
heart complications, its use has not been confirmed in children [7].
Polyacrylate-Polyalcohol Copolymer (PPC, Vantris) is the most
recent industrial biocompatible material from the acryl family that
is used to correct VUR [2]. The size of Vantris particles are at a
level, which allows local and remote migration and therefore do not
lose their stability, after injection, over time. It seems that Vantrisis
eligible as the most ideal material for these cases, but few studies have
addressed this issue [1]. This study aimed to compare the results of
Gil-Vernet surgical treatment and endoscopic method using Vantris
in patients with VUR.
Materials and Methods
In this clinical trial study, 61 children with a diagnosis of VUR
selected from consecutive children who attended a tertiary outpatient
urology referral center and divided by simple randomization into two
groups of Gil-Vernet open surgery or endoscopic surgery during 30
months and the results were compared.
Parents of all patients signed written informed consent. This
study was approved by the Ethics Committee of Tabriz University
of Medical Sciences. The clinical trial was submitted at the Iranian
Registry of Clinical trial (IRCT) by ID number: 2015022321211N1,
IRCT is under supervision of the World Health Organization
(WHO). Inclusion criteria included patients age between one and
ten years, having reflux grade II to IV, occurrence of symptomatic
urinary tract infection (such as fever, dysuria, failure to thrive,
poor nutrition or new renal scarring, in spite of previous antibiotic
treatment or bilateral reflux or drug intolerance or unwillingness
of parents and high grades (III - IV); and exclusion criteria include
dreflux grade I with no complication and V, history of surgery or
endoscopic procedures on bladder or ureter, anatomic urinary tract malformation, including obstruction or full duplicated pielocalicial
system, suspected or proven voiding dysfunction through clinical
findings, including abnormal neurological examination or intestinal
dysfunction or obstructive-stimulatory LUTS, confirmed by VCUG
or sonographic evidence of irregular bladder wall or diverticulum
or trabeculation, low bladder volume and neurogenic bladder. 61
patients (100 renal units) with Vesicoureteral reflux were included
based on pre-determined inclusion and exclusion criteria, after
proving their reflux and the disease grade by VCUG. After explaining
the study terms and conditions, the children were categorized into
one of the groups of Vantris endoscopic injection (Promedone,
Cordoba, Argentina) or Gil-Vernet open surgery. All operations
were done by a single attending pediatric urologist who was trained
with more than 10 years of performing experience for endoscopic
injection. In patients undergoing endoscopic injection (31 patients,
50 renalunits), the Vantris bulking material was sub mucosally
injected through the compact cystoscope with 6-French size and
23-gauge needles under the intramural ureter at 6 o’clock position of
the ureteral orifice (STING method). In patients with higher grades of
reflux and very loose ureteral orifice, it was injected inside the ureter. Volume of injection varied from 0.2 to about 2 cc, depending on the
patient. The patients were discharged the same day of surgery with
oral antibiotics for a week. Finally, follow-up was not feasible on one
renal unit because Left the trial after surgery and 49 renal units were
investigated in this group. In the Gil-Vernet antireflux surgery group
(30 patients, 50 renal units), patients underwent classic Gil-Vernet
antireflux surgery. In this technique, in cases of unilateral reflux, both
sides underwent surgery to prevent reflux in the opposite side due
to trigone instability. These patients were discharged after two days.
Patients had no Foley catheter after surgery and were discharged with
antibiotics for one week. All patients underwent ultrasonography two
weeks after surgery for hydronephrosis (as a complication). Three
months postoperatively, VCUG (voiding cysto-ureterography) was
performed to follow-up of reflux. The reporters of the VCUG images
were unaware of the type of the treatment. Treatment success was
defined as eliminating or reducing the severity of reflux.
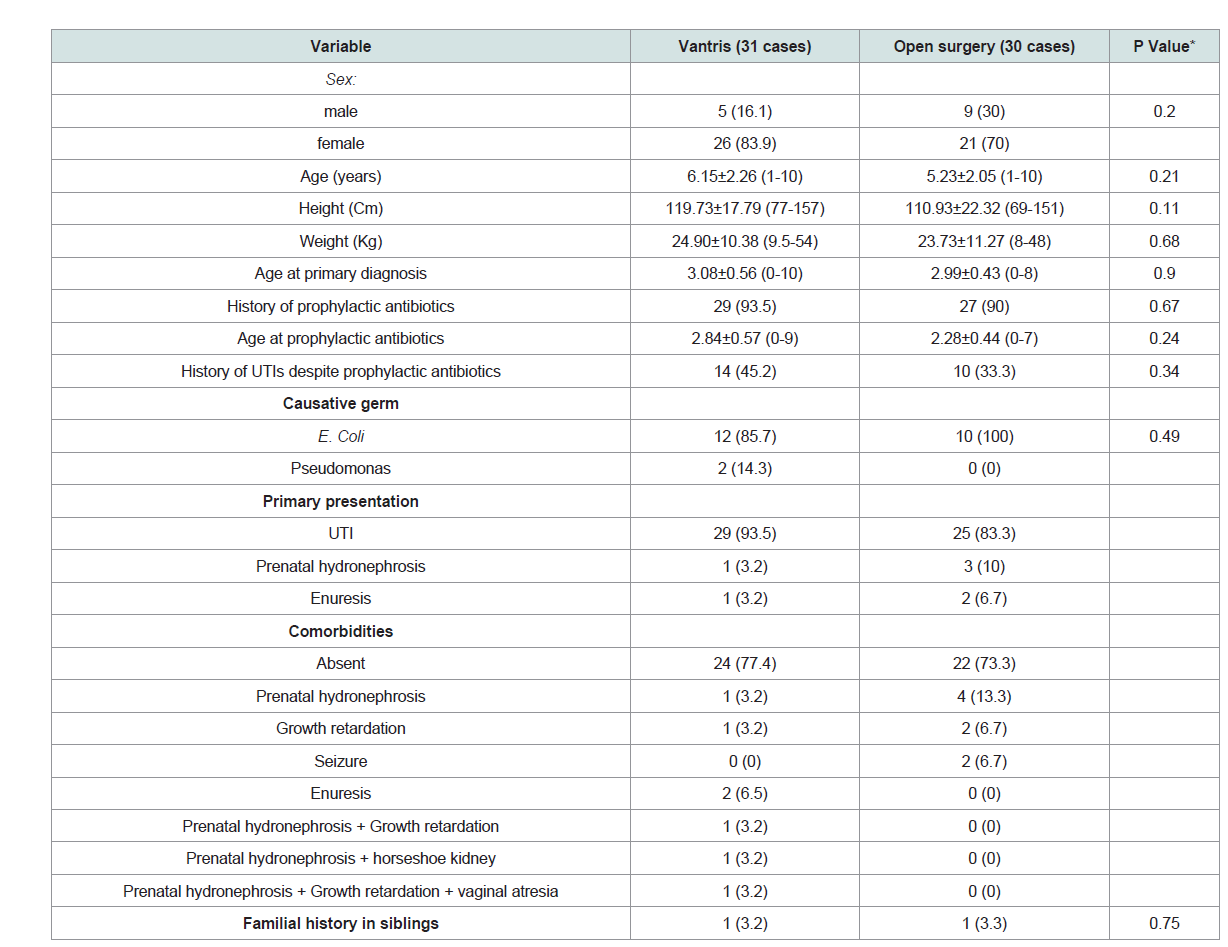
Table 1: Demographic characteristics and variables associated with patients’ history between Vantris and surgical group.
Statistical analysis:
The data was reported by mean±standard deviation, or standard
error (if necessary), and frequency (%). Statistical software SPSS™ (version 16) was used. Normal distribution of quantitative data
was confirmed by Kolmogorov-Smirnov test. To compare variables
between the two groups, t-test and for independent groups, chisquare
test or Fisher’s exact test (depending on conditions) were
used. Repeated measures test was used to assess between-group and
inter-group analysis to assess the changes in disease grade. P<0.05
was considered statistically significant.Results
Demographic characteristics and variables associated with history
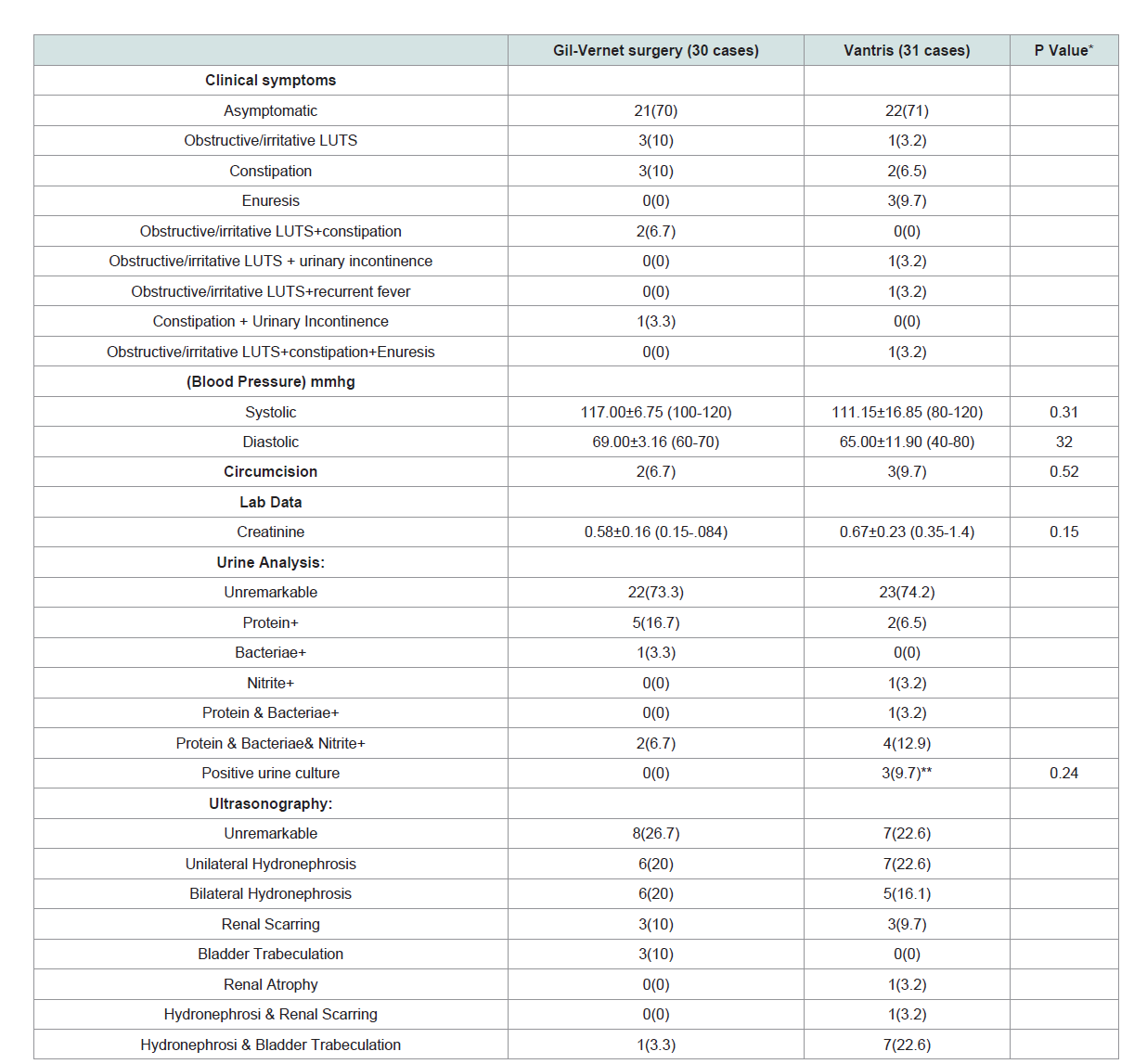
of patients in both groups are summarized in (Table 1). Accordingly, the two groups were similar. Clinical symptoms, laboratory
examination results of both groups are summarized in (Table 2 ).
In these cases, there was also no significant difference between the
two groups. It should be noted that neurologic examination revealed
no cases of mental retardation, impaired gait and spina bifida/
spinal dysraphism. In Vantris group, VUR was on the right in 5
cases (16.1%), on the left in 8 cases (25.8%), and bilateral in 18 cases
(58.1%). VUR in the surgical group was on the right in 6 patients
(20%), on the left in 4 cases (13.3%) and bilateral in 20 cases (66.7%)
and there was not a statistically significant difference in this respect
between the two groups (P=0.47). In Vantris group, the baseline VUR grade was II in one case, III in 24 cases, and IV in 24 cases andin the surgical group was I in 2 cases, II in 12 cases, III in 15 cases,
and IV in 21 cases. The post-surgical VUR grade was I in 3 cases,
and III in 4 cases. VUR grade significantly decreased in both groups
after treatment (P<0.001), however, a significant difference was not
observed between the two groups (P=0.07).
The mean duration of follow-up in Vantris group was 8.81±1.65
months (1 to 22) and in the surgical group was a 7.57±0.89 months (3
to 26). There was no statistically significant difference in this respect
between the two groups (P=0.47). Recovery and non-recovery after
treatment in the Vantris group, was 48 (98%) and 1 (2%), respectively,
and in the surgical group was 47 (96%) and 3 cases (4%). There was no
significant difference in this respect between the two groups (P=0.62).
Full recovery after treatment in the Vantris group was observed in 40
cases (81.6%) and in the surgical group, in 43 cases (86%). There was
no statistically significant difference in this respect between the two
groups (P=0.56). After treatment, VUR occurred in the opposite side
in the Vantris group in one case (3.2%) and in the surgical group in
two cases (6.7%). There was no significant difference in this respect
between the two groups (P=0.61). Symptomatic urinary tract infection
after treatment, during follow-up, occurred in the Vantris group in
one case (3.2%), while there were no cases in the surgical group. There
was no significant differences between the two groups (P=0.51).
Urine analysis or culture was positive after treatment of VUR, during
follow-up, in the Vantris group in two cases (6.5%), while there were
no cases in the surgical group. There was no significant differences
between the two groups (P=0.49). According to the ultrasonography
findings after treatment, during follow-up, in the Vantris group, 24
cases (77.4%) were normal, renal hydronephrosis was recorded in 4
cases (12.9%), renal stone, atrophy, and scar, each in 1 case (3.2%)
and in the surgical group 22 cases (75.9%) were normal, and renal
hydronephrosis occurred in 5 cases (17.2%), and renal scar in 2 cases
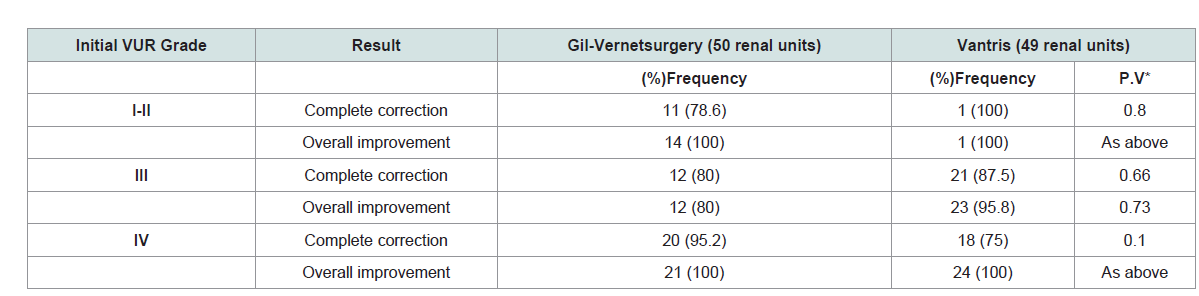
(6.9%). The results of treatment in two groups, based on the initial
severity of VUR, is summarized and compared in (Table 3 ). There
was no statistically significant difference between the two groups.
Two cases had severe hydronephrosis, one of those accompanied
by scarring. The remainder of hydronephrotic cases were of mild
hydronephrosis. For those with severe hydronephrosis, IVP was
done which revealed ureteral stenosis. The atrophic and stone cases
and the open surgery cases with scarring were free of considerable
hydronephrosis/obstruction.The two cases with severe persistent
hydronephrosis underwent extravesical ureteral reimplantation.
Discussion
In the current study, the success rate of endoscopic treatment of VUR after the first injection of Vantrisin patients with severity of
grade II to IV was investigated and the results were compared with
those treated with Gil-Vernet open surgery methods. Duration of
follow-up was, on average, 8 months in both groups. Accordingly,
complete remission and overall recovery was observed in 81.6% and
98% in the Vantris group and in 86% and 94% in the open surgery
group, respectively (no significant difference). Although the decrease
in the severity of disease was non-significant in the Vantris group, it
was at borderline more than other groups.
Vantris was introduced for the first time in 2008, as a bulking
material, in Argentina by Ormaechea and colleagues [8]. After that
some study is done with low included patients but in all of these overall
recovery were more than 80% to near 90% for one injection [9-12].
In a multicenter comprehensive study, carried out by Kocherov and
colleagues (2014), the results of endoscopic treatment of VUR using
Vantris were studied. In this study, a total of 611 pediatric patients were
studied at seven different centers. Follow-up duration ranged from 6
to 54 months and more than half of patients had VUR with grade III.
After the first treatment course, VUR was fully recovered in 93.8%
of patients. Finally, it was concluded that this treatment modality is
simple, safe and effective and can be used in all grades of VUR [13]. In
the study by Corbetta and colleagues (2015), the results of endoscopic
treatment using Vantris were evaluated in 81 children with VUR
(117 renal units). The overall recovery rate in this study was 92.3%.
Finally, it was concluded that this therapy has a high efficiency [14].
It has been pointed out in the conclusion of the study results that the
success rate (total or complete) ranged from 71% to 98.1% in similar
investigations; accordingly, the results of the present study is also
within this range and is in a high level. It should be noted that success
rate of endoscopic treatment of VUR using different bulking materials
have been reported at 70 to 80% [15-17]. In a study by Abdullaev et al.
(2013) on 4000 cases of VUR treated with endoscopic treatment using
a variety of bulking materials, it was concluded that the best material
is Vantrisin this regard [18]. Vantrisis a non-biodegradable synthetic
material; that is why it creates fibrotic capsule at the injection site that
leads to stability, continuity, and survival in place for a long time.
This material belongs to the Acrylics family, in which the polyacrylate
polyalcohol copolymer particles are floating in a physiologic carrier
solution. The high molecular weight of the material causes it to last for
a long time after injected in the place, through creating a mass status.
The used carrier contains 40% glycerol solution that is absorbed
by the reticular system after injection and is excreted through the
kidneys without being metabolized. Since Vantris contains anionic
particles with high surface electron negativity, it induces little cell response and fibrotic growth. Studies have shown that this material
is not mutagenic and toxic. In addition, histological examination
of the animal organs with this material has shown that it does not
cause particle migration. Thus, Vantrisis considered one of the best
bulking materials in endoscopic treatment of VUR [8]. However,
some studies have reported the major limitation of the endoscopic
treatment of VUR as its high degree of inefficiency in severe cases of
the disease [19]
Meanwhile, Dogan et al. (2015) found no significant relationship
between initial severity of the disease and the success rate of
endoscopic method, in their study [20]. In the present study, the
success rate of this treatment are reported separately, based on the
severity of VUR (Table 3).
Accordingly, the overall success rate was
high in all the investigated severities (100% in group I-II and IV, and
80% in group III). However, it is recommended that future studies
examine this treatment in severe cases with grade V with sufficient
sample size in each group. It should be noted that this study is the
first clinical comparing the results of using Vantris with the results
of Gil-Vernet open surgery. In all of other study there were not any
comparisons with gold standard. Gil-Vernet open surgical procedure
is considered an intravesical method, where medial ureter is displaced.
Among open surgical procedures, this method is very simple, and fast
and is associated with high success rates. Based on previous studies,
the success rate of this method is usually more than 90% and in some
cases 100% [21-23]. For example, in the study by Basiri et al. (2008)
in Iran, 96 patients with VUR (150 renal units) underwent Gil-Vernet
surgery with a recovery rate of 92% [24]. The study by Mirshemirani
et al. (2010) in Iran, also, investigated the results of Gil-Vernet open
procedures in 72 patients with VUR. The mean duration of follow-up
in this study was 48 months. Full recovery following this surgery was
reported 96.2%[5]. As evident, the results of our study are consistent
with previous studies regarding the efficiency of this procedure.
However, it should be noted that endoscopic treatment has more
advantages over open surgery. The benefits of endoscopic vs. surgical
methods include less complications, cost, and no scarring on the skin
surface. In addition, unlike open surgery, endoscopic procedures can
be done on outpatient basis and do not require hospitalization [18].
Conclusion
According to this study, the results of the endoscopic treatment
with Vantris in short follow-up period is similar to the open surgery
with Gil-Vernet technique. With respect to the superiorities of Vantris
over Gil-Vernet such as short hospital stay and an early recovery, we
recommend it for VURs with severities less than V.