Journal of Pediatrics & Child Care
Download PDF
Case Report
*Address for Correspondence: Aye Aye Myint, Department of Pediatrics, Mandalay Children Hospital, University of Medicine Mandalay, Ayeyeik Mon Complex, Bayint Naung, Hlaing township, Yangon, Myanmar, Tel: (095) 01681517; E-mail: aye441@gmail.com
Citation: Kyawswamyint, Myint AA, Moe H, Win K, Mon O. The Effectiveness of 2 Years of First Line Antiretroviral Therapy among HIV-Infected Children at an Integrated HIV-Care Clinic in Myanmar. J Pediatrics Child Care. 2015;1(1): 6.
Copyright © 2015 Myint et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Pediatrics & Child Care | ISSN: 2380-0534 | Volume: 1, Issue: 1
Submission: 11 March 2015 | Accepted: 30 May 2015 | Published: 06 June 2015
Reviewed & Approved by: Dr. Thyyar M. Ravindranath, Assistant Professor of Pediatrics, Columbia University Medical Center, USA
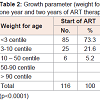
Growth parameter (weight for age) of HIV-infected children at the start, one year and two years of ART is presented in Table 2. At the start of ART, among 116 cases, growth parameter of 85 cases (73.3%) were < 3rdcentile, 25 cases (21.6%) were between 3rd and 10th centile, 6 cases (5.2%) were between 10th and 50th centile and there were no cases between 50th and 90th centile and > 90th centile.
At one year of ART, among 101 cases, 27 cases (26.7%) were < 3rd centile, 54 cases (53.5%) were between 3rd and 10th centile, 18 cases (17.8%) were between 10th and 50th centile, 2 patients (2%) were between 50th and 90th centile and there were no cases > 90th centile.
At one year of ART, among 101 cases, 2 (2%) cases had < 9 g/dl, 16 (15.8%) between 9 and 9.9 g/dl, 27 (26.7%) between 10 and 10.9 g/dl and 56 (55.5%) patients had > 11 g/dl.At two years of ART, out of 95 cases, 4 (4.2%) cases had hemoglobin status of < 9 g/dl, another 4 (4.2%) cases between 9 and 9.9 g/dl, 13 (13.7%) cases between 10 and 10.9 g/dl and 74 (77.9%) cases had > 11 g/dl.
The Effectiveness of 2 Years of First Line Antiretroviral Therapy among HIV-Infected Children at an Integrated HIV-Care Clinic in Myanmar
Kyawswamyint1, Aye Aye Myint1*, Hla Moe2, Khaingkhaing Win1 and Ohnmar Mon1
- 1Department of Pediatrics, Mandalay Children Hospital, Myanmar
- 2Department of Preventive and Social Medicine, University of Medicine, Mandalay
*Address for Correspondence: Aye Aye Myint, Department of Pediatrics, Mandalay Children Hospital, University of Medicine Mandalay, Ayeyeik Mon Complex, Bayint Naung, Hlaing township, Yangon, Myanmar, Tel: (095) 01681517; E-mail: aye441@gmail.com
Citation: Kyawswamyint, Myint AA, Moe H, Win K, Mon O. The Effectiveness of 2 Years of First Line Antiretroviral Therapy among HIV-Infected Children at an Integrated HIV-Care Clinic in Myanmar. J Pediatrics Child Care. 2015;1(1): 6.
Copyright © 2015 Myint et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Pediatrics & Child Care | ISSN: 2380-0534 | Volume: 1, Issue: 1
Submission: 11 March 2015 | Accepted: 30 May 2015 | Published: 06 June 2015
Reviewed & Approved by: Dr. Thyyar M. Ravindranath, Assistant Professor of Pediatrics, Columbia University Medical Center, USA
Abstract
Objective: To study the effectiveness of 2 years first line antiretroviral therapy on weight for age, haemoglobin, CD4 count among HIV infected children at integrated HIV-care clinic, Mandalay Children hospital (MCH).Method: This study was prospective cohort study performed on a total of 116 HIV infected children who started Anti Retroviral Therapy (ART) from 1st January to 31st December of 2010. At the start of the study, ART treatment has been established for one to two years. The follow up period was up to one year. Weights, weight for age, haemoglobin and CD4 counts were obtained from the medical records of individual patient at the start of ART and also at one year of ART for some children. Data were also recorded at 2 years of ART therapy. During every visit, each case of death, defaulter and regular follow-up and loss to followup cases were recorded. The reviews of medical records of patients at follow-up visits were done. Then, two years survival was calculated.
Results: Out of 116 cases, 85 (73.28%) patients were < 3rdcentile weight for age at ART initiation. After 1 year of ART, 74 (73.27%) cases were > 3rd centile and 88 (92.63%) cases were > 3rd centile after 2 years of ART. The median increase in weight at 1 year of ART was 3 kg (p=<0.001), and at 2 years was 7 kg (p =<0.001). At the start of ART 31.90% children had < 9 g/dl hemoglobin, but 1.98% and 4.21% of cases were <9 g/dl hemoglobin at 1 year and 2 years of ART. The medianhaemoglobin increased from 9.6 g/dl at the start to 11 g/dl at 1 year (p =<0.001), and 11.5 g/dl at 2 years of ART (p =<0.001). The medianCD4 count increased from 210 cells/µL at the start to 694 cells/µL at 1 year (p =<0.001) and 930 cells/µL at 2 years of ART (p =<0.001). Among116 patients, 95 (81.90%) had regular follow-up visits, 12 (10.34%) were lost for follow-up, 9 (7.8%) deaths were noted and cumulative survivalprobability at two years of ART was 0.82.
Conclusion: Good survival, positive effect on growth, hemoglobin status and CD4 count can be sustained after two years of first line ART among HIV infected children in resource-constrained settings. Low CD4 count and low haemoglobin status at the start of ART could have considerable impact on growth and other associated infections such as tuberculosis, viral hepatitis, and chronic diarrhea.
Abbreviations
ART: Antiretroviral Therapy; HIV: Human Immunodeficiency Virus; IHC: Integrated HIV-Care Clinic; CD: Cluster Designation; MCH: Mandalay Children’s Hospital; MGH: Mandalay General HospitalIntroduction
The history of HIV dates back to early 1981s. The first case of pediatric HIV was described in 1982 and the causative agent, HIV, was first isolated in 1983 [1,2]. Since the onset of pandemic in the early 1980s, HIV infection has become a global health problem. Every day, nearly 1200 children under 15 years of age are newly infected with HIV. Unfortunately, more than 90% of the two million of HIV infected children worldwide live in developing countries [3,4].The challenges of managing HIV positive children are particularly complex. Children need life-long ART. In South- East Asia access to HIV treatment covered 47% of those in need in 2011 [5].
The population of Myanmar in 2010-11 was estimated at 59.78 million. Among them, 29.44% are children under 14 years of age which amounts to substantial amount of the total population [6]. It is estimated that around 238,000 adults and children are living with HIV in 2009. Incidence is estimated at well above 10,000 new infections per year [7]. The government of Myanmar has initiated ART program since 2005. HIV prevalence among general population and pregnant women is below 1%, National AIDS Program linked to public health hospitals, which provide specialized clinical services such as ART provision, and hospital based prevention of mother to child transmission since 2005 [8]. In Mandalay, Integrated HIV-Care Clinic was started in 2005 at MCH and provides comprehensive care for HIV-infected children. The clinic provided ART to 62, 74 and 126 children with HIV in 2008, 2009 and 2010 respectively.
World Health Organization (WHO, 2010) has recommended non-nucleotide reverse transcriptase inhibitor (NNRTI) based regimens for resource-limited countries [3]. ART has been shown to be effective in suppressing viral replication and decreased HIV associated mortality and morbidity while promoting growth. Moreover, this therapy leads to immune reconstitution which can be shown by an increase in CD4 cells [9].
Few studies have evaluated the impact of HAART on survival, weight gain, height and CD4 counts. In Cambodia, Raguenaud et al. based on retrospective cohort study done on 1168 HIV-positive children 10].
Yotebieng et al. has shown that a cohort of 1394 HIV infected children treated with ART between April 2004 and March 2008 in Johannesburg, South Africa showed increase in CD4% in the first 6 months of ART was the best predictor of poor subsequent ART outcomes. They mentioned that in areas with limited access to CD4%, weight gain post-ART was a good alternative to CD4% [11].
In India, Banerjee et al. based on 5 years cohort study of 180 children with vertically HIV infected children had mentioned that survival rates of children improved which correlated with an increase in CD4 cell count concurrent with the expanded use of ART. ART had a positive effect on growth in HIV-1-infected children. Nutrition supplementation improved the health of children in both the no-ART and ART groups [12].
However, there is little information on these factors in Asia, especially government-sponsored ART program. Therefore, the objective of this article was to study the effectiveness (Weight for age, Haemoglobin and CD4 count) of 2 years first line antiretroviral therapy among HIV-infected children at integrated HIV-care clinic at the Government Hospital of Mandalay Children’s hospital.
Methods
Type of studyThis study was prospective cohort study. The study protocol was approved by Institutional Review Board of the University of Medicine, Mandalay and by the Ethical Committee of the University of Medicine, Mandalay. The study period was from 1st January 2010 to 31st December 2012.
Study population
The study population included Children (0-12 years of age) who started ART at IHC clinic, MCH from 1st January to 31st December in 2010. All children who started ART in 2010, regardless of duration of ART, deaths and defaulters were counted in the survival analysis of the study.
Study design
At IHC clinic, every Monday, the clinic visit of study population was recorded and the study was explained to them. One hundred and sixteen children who received ART in 2010 were studied. Clinical history, physical examinations were done and measured child’s weight was plotted on NCHS to get weight for age of an individual child. CD4 testing, complete blood count of each patient at the time of initiation of ART and at one year of ART were recorded by using the pre-structured forms. Then comparison of treatment responses by means of weight for age, haemoglobin level and CD4 count among 0, 1 and 2 years of ART treatment were done.Weight was measured to the nearest 0.1 kg by beam type weighing machine in children older than two years and by baby scale weighing machine in children younger than two years. The weighing machine was standardized before measuring and zeroing of the machine was carried out before each measurement. Children were subjected to CD4 count at follow up in IHC clinic. CD4 counts as well as hemoglobin measurements were performed in the laboratory of MGH.Death, defaulter, regular follow-up, or loss to follow-up cases was recorded. If needed, active tracing of death or defaulter was done by social workers and one of the researchers. The review of medical records of patients at follow-up visits were also done. Two year survival was calculated.
Statistical analysis
Data was collected by using pre-structured forms and from medical records of patients. Following data collection and prior to data entry, missing data was checked. The data entry was done by using Microsoft Excel 2007. All statistical analyses were conducted using R software [13]. We used frequency distributions for descriptive statistics and Pearson’s Chi-square and Fisher’s exact test for categorical data as well as paired t-test for continuous data to show significant differences. Kaplan -Meier analysis was used for survival at two years. We also performed linear mixed effect analysis for each of weight, haemoglobin and CD4 count by using R and lme4 [14]. For fixed effects, we included year of ART, age and gender into the model. For random effects, we had intercepts for subjects. P-values were obtained by likelihood ratio tests of the full model against the null model.
Treatment and follow up
ART was started in patients after a minimum of three counseling sessions. Zidovudine, lamivudine and nevirapine were used as first line ART treatment and abacavir, didanosine and lopinavir were used as second line therapy. As per WHO clinical guidelines on HIV/AIDS in infants and children (WHO, 2010) patients in WHO stage 3 or 4 are initiated on ART and also started on sulfamethoxazole/trimethoprim prophylaxis. In the study, 92% of study population took prophylaxis during the study period. In general follow up visits were every three months during which blood and CD4 counts were monitored. Support was provided to caregivers and children by specially trained counselors. Active tracing was done by social workers and a researcher.
Inclusion criteria
Children who started ART from 1st January to 31st December of 2010.
Exclusion criteria
1. HIV infected children who started ART outside of the defined enrollment period.
2. Children whose parents or guardian refused consent.
3. Children with lost or incomplete medical records during study period.
Operational definition Defaulters: Children who failed to come to IHC clinic and take ART according to scheduled visits for three months or more from the last known contact date at the clinic.
Loss to follow-up: Children who do not attend IHC clinic at recommended follow-up schedules, and not found at their residence on active tracing. Their status of life or death was unknown.
Transferred-out cases: Children who are transferred out of the adult IHC clinic after attaining 13 years of age.
Results
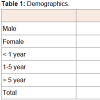
Among 116 cases of HIV infected children on antiretroviral therapy for two years, 2 cases (1.72%) were < 1 year, 47 cases (40.5%) were 1-5 years and 67 cases (57.8%) were > 5 years. 59 cases (50.9%) were males and 57 cases (49.14%) were females (Table 1). Of 116 HIV-infected children on ART for 2 years, 95 (81.9%) children attended the clinic regularly and 12 (10.3%) patients were lost for follow-up. There were 9 (7.8%) deaths and no defaulters.Growth parameter (weight for age) of HIV-infected children at the start, one year and two years of ART is presented in Table 2. At the start of ART, among 116 cases, growth parameter of 85 cases (73.3%) were < 3rdcentile, 25 cases (21.6%) were between 3rd and 10th centile, 6 cases (5.2%) were between 10th and 50th centile and there were no cases between 50th and 90th centile and > 90th centile.
At one year of ART, among 101 cases, 27 cases (26.7%) were < 3rd centile, 54 cases (53.5%) were between 3rd and 10th centile, 18 cases (17.8%) were between 10th and 50th centile, 2 patients (2%) were between 50th and 90th centile and there were no cases > 90th centile.
At 2 years of ART, out of 95 cases, 7 cases (7.4%) were < 3rd centile, 41 cases (43.2%) were between 3rd and 10th centile, 38 cases (40%) were between 10th and 50th centile, 9 cases (9.5%) were between 50th and 90th centile and there were no cases > 90th centile.
After one year of ART, 27 cases (26.7%) were still less than 3rd centile and 7 cases (7.4%) were also still less than 3rd centile weight for age after two years of ART. These patients without improvement in growth were analyzed for possible associated factors that may be responsible for growth failure.
Out of these 27 patients with growth failure, 14 cases (>50%) were found to have low CD4 count (<200 cell/µL) at initiation of ART and 6 cases had low initial haemoglobin. Therefore, growth improvement after ART therapy may depend on initial CD4 count and haemoglobin status. Therefore patients with low CD4 and low haemoglobin counts at the initiation of ART therapy may be at risk for growth failure despite treatment initiation with ART. In addition, out of 27 patients,10 patients were found to be afflicted with pulmonary TB during ART treatment, 2 patients had chronic diarrhea, 2 patients were infected with hepatitis B , 1 patient had cerebral palsy of unknown cause. 2 patients were switched from 1st line ART to 2nd line ART and 1 patientneeded blood transfusion following AZT induced anemia. In these 27 patients, 13 patients had very low CD4 count (<100 cells/µL) and 7 patients had low CD4 count (100-200 cell/µL) at the start of ART. The growth failures after one year of ART were associated with coinfectionslike pulmonary TB, hepatitis B and chronic diarrhea as well as underlying disease such as cerebral palsy. Treatment failure from first line drugs may be due to one of the underlying causes of growth failure among the study population.After one year of ART, there were 74 cases (73.3%) without growth failure. Among them, 60 cases (81.1%) showed >350 CD4 counts and 40 patients (54.1%) had >500 CD4 counts. Although there were improvements in CD4 count after one year of ART in children without growth failure, 10% of patients still had CD4 counts <200.
Figure 1 demonstrates haemoglobin status of HIV-infected children at the start, one and two years of ART. At the start of ART, out of 116 cases, haemoglobin status of 37 (31.9%) cases were < 9 g/dl, 26 (22.4%) cases had haemoglobin status between 9 and 9.9 g/dl, 43 (37.1%) between 10 and 10.9 g/dl and 10 (8.7%) had > 11 g/dl.
At one year of ART, among 101 cases, 2 (2%) cases had < 9 g/dl, 16 (15.8%) between 9 and 9.9 g/dl, 27 (26.7%) between 10 and 10.9 g/dl and 56 (55.5%) patients had > 11 g/dl.At two years of ART, out of 95 cases, 4 (4.2%) cases had hemoglobin status of < 9 g/dl, another 4 (4.2%) cases between 9 and 9.9 g/dl, 13 (13.7%) cases between 10 and 10.9 g/dl and 74 (77.9%) cases had > 11 g/dl.
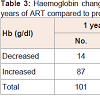
According to Table 3, compared to at the time of initiation of ART, 87 (86.1%) cases showed increased haemoglobin status at 1 year of ART and 91 (95.8%) cases at 2 years of ART. 14 (13.9%) cases had decreased haemoglobin level at 1 year of ART and 4 (4.2%) cases at 2 years of ART compared to at the start of ART.
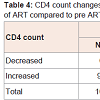
Table 4 demonstrates CD4 count changes of HIV-infected children at one year and two years of ART compared to pre ART. Compared to at the initiation of ART, there were increased level of CD4 counts in 95 (94.1%) cases at 1 year of ART and 91 (95.8%) cases at 2 years of ART. There were decreased level in 6 (5.9%) cases at 1 year and 4 (4.2%) cases at 2 year of ART.
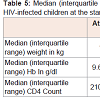
Median weight, haemoglobin and CD4 count of HIV-infected children at the start, one year and two years of ART are presented in Table 5. The median increase in weight at 1 year of ART was 3 kg (P <0.001). The median increase in weight at 2 years of ART was 7 kg (P <0.001). The median increase in haemoglobin level at 1 year of ART was 1.4 g/dl (P <0.001). The median increase in haemoglobin level at 2 years of ART was 1.9 g/dl (P <0.001). The median increase in CD4 count at 1 year of ART was 484 cells/μl (P <0.001). The median increase in CD4 count at 2 years of ART was 720 cells/μ (P <0.001).
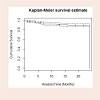
By using Kaplan-Meier survival estimate curve, cumulative survival at two years was 0.82 (82%) (Figure 2). Mean survival time was 20.9 months (95% CI 19.6 to 22.2). Among 116 cases at IHC clinic in MCH, 95 (81.9%) regular follow up cases, 12 (10.3%) loss to follow up cases, 9 (7.8%) death cases were noted. In our study, among 9 death cases, 6 patients died before completing one year of ART and 3 patients after one year of ART.
Discussion
In our study, out of 116 cases, 85 (73.3%) patients were < 3rd centile weight for age at ART initiation. This meant that almost all infected children were underweight at the start of ART.The median increases in weight at 12 months, at 24 months were 3 kg and 7 kg respectively. The weights at 12 months were greater than the baseline value in 93.2% of the children. In India, study by Rajasekaran et al. mentioned that the median increase in weight at 24 months was greater than the baseline value in 100% of the patient [15].
Anaemia a common complication of pediatric HIV infection has been associated with disease progression and death [16]. At the start of ART, most children (31.9%) had < 9 g/dl haemoglobin, but 2% and 4.2% of cases had < 9 g/dl haemoglobin at 1 year and 2 years following treatment with ART respectively. At the same time, very small proportion of children (8.6%) had > 11 g/dl haemoglobin at the start of ART, but 55.5% and 77.9% of patients had > 11 g/dl haemoglobin at 1 and 2 years of ART respectively. A great improvement in haemoglobin status was noted after 1 and 2 years of ART therapy compared to at the start of ART. After analysis of RDW and MCV values in anemic patients (Hb<9 g/dl) at initiation of ART, one year and two years after ART therapy, 70% of anemic children showed decreased MCV and increased RDW indicating that the cause of anemia was nutritional, whereas in 25% of patients anemiawas related to non-nutritional causes such as RVI itself, and other opportunistic infections or drug related secondary to zidovudine orsulfamethoxazole/trimethoprim.
Haemoglobin status improvement was comparable to other studies in developing countries. In India, hemoglobin at 12 months of ART therapy was greater than the baseline value in 86.6% of the children and the haemoglobin at 24 months of ART was greater than the baseline value in 92.9% of the children [15].
In our study, haemoglobin status at 1 year and 2 years of ART was greater than the baseline value (at the start of ART) in 86.1% and 95.8% respectively. Some patients (13.9% of patients at 1 year and 4.2% of patients at 2 years of ART), were found have lower haemoglobin value compared to at the start of ART.
World health organization (WHO) has recommended nonnucleotide reverse transcriptase inhibitor (NNRTI) based regimens for resource–limited countries. Although Zidovudine cause anemia, NNRTI based regimens are feasible and effective in our setting.
Regarding the hemoglobin status of study population, the limitations of this study is that blood transfusion or hospitalization status for anemia was not noted in our records. Anemia may relate to drug therapy as this center (IHC of MCH) used Zidovudine in first line ART treatment in 80% of patients. Incidence of Zidovudine related anaemia is limited. Kumarasamy et al. mentioned that anemia was diagnosed in 4.5% of South Indian children with Zidovudine [17]. In a Chinese study, there were no reports of anemia [18].
The median CD4 counts of HIV-infected children was 210 cells/μl (IQR 117.5-325) at the start of ART, 694 cells/μl (IQR 397-950) at 1 year of and 930 cells/μl (IQR 620-1116) at 2 years of ART. The median gain in CD4 cell count at 1 year of ART was 484 cells/μl and 720 cells/μl at 2 years of ART.
In a Cambodia study, median CD4 gain was 704 cells/μl at 24 months and 737 cells/μl at 36 months [19]. The median CD4% increased from 6% at the start of ART to 21.7% at 12 months and 24.6% at 24 months respectively [20].
The CD4 at 12 months was greater than baseline value in 95.2% of the patients, and CD4 counts at 24 months was greater than baseline value in 95.2% of the patients [15]. In this study, compared to CD4 counts at the start of ART, there were positive change in CD4 counts in 94.1% and 95.8% of patients at one year and two years of ART respectively. Decreased counts occurred in 5.9% and 4.2% of patients at 1 and 2 years of ART compared to at the start of ART.
The mortality rate markedly increased just after initiation of ART (within one year after ART initiation) than after one year of ART. All deaths were related to low CD4 counts and growth failure at the start of ART. However, 2 of 9 patients showed low haemoglobin (<9 g %) atthe start of ART. Severe anemia, growth failure and low CD4 counts before ART might predict early mortality in HIV infected children.
In India, among 295 children on ART, 260 (88%) of children were still alive and being treated, 24 (8%) were known to have died, and the remaining children were lost for follow up over 30 month period [15]. In Lesotho, the third highest HIV prevalence in the world, their outcome is highly satisfactory, with 89.4% remaining in care at 12 months and 87.5% at 24 months of ART [21]. In Cambodia, among the 670 children who started ART, 37 (5.5%) had died, 13 (2.0%) patients were lost for follow up over 3 year period. The survival probability was 0.93 and 0.91 at 24 and 36 months after ART [19]. In this study, survival probability after 2 years of ART was 0.82 (82%).
Our study has a number of limitations. The sample size in this study was small because five years ago only a small number of patients received ART treatment. However, the number of patients receiving ART treatment has substantially increased since then. Another limitation of our study is that we have limited data recorded in medical record on haemoglobin status of our patients especially regarding transfusion history or needing hospitalization for anaemia.
Conclusion
In a government children hospital of upper Myanmar, children infected with HIV, ART had a positive effect on growth, hemoglobin status, CD4 counts and survival. These improvements were better the longer the patients were on ART therapy. Some children with growth failure during one year of ART treatment were found to have low CD4 counts and anemia at the start of ART and also were co infected with either TB, viral hepatitis B or had chronic diarrhea. The underlying disease such as cerebral palsy was also one of the causes of growth failure. The treatment failure to first line ART could be due to the one of the above reasons.In our study a high rate of regular follow-up, low rate of loss to follow-up and good 2 years survival probability 0.82 (82%) were observed. Mortality rate was increased soon after initiation of ART than after one year therapy.
Acknowledgements
We thank all of the people involved in this study including Dr. Tin Maung Han, dean of the University of Medicine Mandalay and Dr. Hla Moe for his expert opinion on statistical analysis of the data. We would like to thank the patients, caregivers and their families for their participation to this study.References
- Mark C (2010) An HIV time line-The history of HIV.
- Caroline F, Diana G (2008) HIV infection. In: N Mclntosh, P Helms, R Smyth, S Logan (Eds). Forfar and Arneil’s textbook of pediatrics, (7th edn), Churchill Livingstone, London, 1259-1274.
- World Health Organization (2006) Antiretroviral therapy of HIV infection in infants and children in resource-limited settings: towards universal access. Recommendation for a public health approach. Geneva, Switzerland 1-83.
- UNAIDS (2008) 2008 Report on the global AIDS epidemic. Executive summary.
- UNAIDS (2012) Regional fact sheet 2012: Asia and the Pacific.
- Department of Health (2012) Health in Myanmar. Ministry of health, Union of Myanmar.
- (2010) UNGASS Country progress report, Myanmar, National AIDS programme.
- NAP (2015) National AIDS program, Department of Health. Overview of national ART program.
- Kabue MM, Kekitiinwa A, Maganda A, Risser JM, Chan W, et al. (2008) Growth in HIV-infected children receiving antiretroviral therapy at a pediatric infectious diseases clinic in Uganda. AIDS Patient Care STDS 22: 245-251.
- Raquenaud ME, Isaakidis P, Zachariah R, Te V, Soeung S, et al. (2009) Excellent outcomes among HIV+ children on ART, but unacceptably high pre-ART mortality and losses to follow-up: a cohort study from Cambodia. BMC Pediatr 9: 54.
- Yotebieng M, Van RA, Moultrie H, Meyers T (2010) Six-month gain in weight, height, and CD4 predict subsequent antiretroviral treatment responses in HIV-infected South African children. AIDS 24: 139-146.
- Banerjee T, Pensi T, Banerjee D, Grover G (2010) Impact of HAART on survival, weight gain and resting energy expenditure in HIV-1-infected children in India. Ann Trop Paediatr 30: 27-37.
- R Development Core Team (2012) R: a language and environment for statistical computing. R foundation for statistical computing, Vienna, Austria.
- Bates D, Maechler M, Bolker B (2012) lme4: linear mixed-effects models using S4 classes.
- Rajasekaran S, Jeyaseelan L, Ravichandran N, Gomathi C, Thara F, et al. (2009) Efficacy of antiretroviral therapy program in children in India: prognostic factors and survival analysis. J Trop Pediatr 55: 225-232.
- Janssen N, Ndirangu J, Newell ML, Bland RM (2010) Successful paediatric HIV treatment in rural primary care in Africa. Arch Dis Child 95: 414-421.
- Kumarasamy N, Venkatesh KK, Cecelia AJ, Devaleenal B, Lai AR, et al. (2008) Spectrum of adverse events after generic HAART in southern Indian HIV-infected patients. AIDS Patient Care STDS 22: 337-344.
- Bunupuradah T, Aurpibul L, Ananworanich J, Puthanakit T (2009) The effectiveness of highly active anti retroviral therapy among HIV- infected children in Asian countries, Asian Biomed 3: 89-100.
- Isaakidis P, Raguenaud ME, Te V, Akao K, Kumer V, et al. (2010) High survival and treatment success sustained after two and three years of first-line ART for children in Cambodia. J Int AIDS Soc 13: 11.
- Parakh A, Dubey AP, Kumar A, Maheshwari A, Saxena R (2009) Efficacy of first-line, WHO recommended generic HAART regimens in Indian children. Kathmandu Univ Med J (KUMJ) 7: 220-225.
- Cohen R, Lynch S, Bygrave H, Eggers E, Vlahakis N, et al. (2009) Antiretroviral treatment outcomes from a nurse-driven, community-supported HIV/AIDS treatment programme in rural Lesotho: observational cohort assessment at two years. J Int AIDS Soc 12: 23.