Journal of Pharmaceutics & Pharmacology
Download PDF
Case Report
Use of Intravenous Acetaminophen to Reduce Opioid Use in Patients Undergoing Bariatric Surgery at a Community Teaching Hospital
C. EeJay Enekwa1*, Teresa I. Pounds2, Annesha Lovett 3, Pamela M. Moye3, Larry Hobson4, Titus Duncan4 and Maurice Gilbert5
- 1Cartersville Medical Center, 960 Joe Frank Harris Pkwy SE, Cartersville, GA 30120, USA2Atlanta Medical Center, 303 Parkway Dr NE, Atlanta, GA 30312, USA3Mercer University College of Pharmacy, 3001 Mercer University Drive Atlanta, GA 30341-4155, USA4Peachtree Surgical and Bariatrics 315 Boulevard NE, Ste 332, Atlanta, GA 30312, USA5Northlake Anesthesia Professionals, 303 Parkway Dr NE Suite 120, Atlanta GA 30312, USA
- Wininger SJ, Miller H, Minkowitz HS, Royal MA, Ang RY, et al. (2010) A randomized, double-blind, placebo-controlled multicenter, repeat-dose study of two intravenous acetaminophen dosing regimens for the treatment of pain after abdominal laparascopic surgery. Clin Ther 32: 2348-2369.
- Sinatra RS, Jahr JS, Reynolds LW, Viscusi ER, Groudine SB, et al. (2005) Efficacy and Safety of Single and Repeated Administration of 1 gram Intravenous Acetaminophen Injection (Paracetamol) for Pain Management after Major Orthopedic Surgery. Anesthesiology 102: 822-831.
- The Joint Commission. Sentinel Event Alert #49: Safe Use of Opioids in Hospitals.
- Macario A, Royal MA (2011) A Literature Review of Randomized Clinical Trials of Intravenous Acetaminophen (paracetamol) for acute postoperative pain. Pain Prac 11: 290-296.
- McNicol ED, Tzortzopoulou A, Cepeda MS, Francia MB, Farhat T, et al. (2011) Single-dose intravenous paracetamol or propacetamol for prevention or treatment of postoperative pain: a systematic review and meta-analysis. Br J Anaesth 106: 764-775.
- Mattia C, Coluzzi F (2009) What anesthesiologists should know about paracetamol (acetaminophen). Minerva Anesthiol 75: 644-653.
- O’neill T, Allam J (2010) Anaesthetic Considerations and Management of the Obese Patient Presenting for Bariatric Surgery. Current Anaesthesia and Critical Care 21: 16-23.
- Bankhead C (2012) Regimen Lowers Opioid Use After Bariatric Surgery.
- Aston G (2012) Smart Pain Management Makes Good Business Sense. Hosp Health Netw 86: 38-40, 49-50, 1.
*Address for Correspondence: C. EeJay Enekwa, Cartersville Medical Center, 960 Joe Frank Harris Pkwy SE Cartersville, GA 30120, USA, 615-584-5587; E-mail: eejayenekwa@yahoo.com
Citation: Enekwa CE, Pounds TI, Lovett A, Moye PM, Hobson L, et al. Use of Intravenous Acetaminophen to Reduce Opioid Use in Patients Undergoing Bariatric Surgery at a Community Teaching Hospital. J Pharmaceu Pharmacol. 2014;2(2): 3.
Copyright © 2014 Enekwa CE, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Pharmaceutics & Pharmacology | ISSN: 2327-204X | Volume: 2, Issue: 2
Submission: 30 June 2014 | Accepted: 22 September 2014 | Published: 26 September 2014
Abstract
Purpose: The use of intravenous (IV) acetaminophen has been evaluated in several clinical trials and systematic reviews and has been shown to be an effective pain medication that can reduce the need for opioids. Recently, the Pharmacy and Therapeutics (P&T) committee at Atlanta Medical Center (AMC) approved an extension of the use of IV acetaminophen from one dose intra-operatively to four doses over 24 hours for 30 patients. The objective of this study was to compare the use of IV acetaminophen dosed at 1 g every 6 hours, to the previous use of 1 g for one dose at AMC in patients undergoing bariatric surgery.Methods: Patients were divided into two groups; control group consisting of patients who received one dose of IV acetaminophen in the operating room (OR) and the intervention group consisting of patients who received four doses of IV acetaminophen over a 24 hour period. The primary endpoint was the total amount of opioids required by patients over 24 hours measured in morphine equivalents. The secondary endpoints were the adverse effects and average pain scores.
Results: The final sample consisted of 30 patients in each group. The total amount of opioids used by the intervention group was 28.3% lower than that of the control group. The average amount of opioids required by patients in the intervention group was 13.08 mg compared to 18.23 mg in the control group (p = 0.15). The only adverse event experienced within the groups was nausea/vomiting (p = 0.1). The average pain score reported by patients in the intervention group was 4.58 compared to 6.12 in the control group (p = 0.04).
Conclusion: Although not powered to show statistical significance between groups, IV acetaminophen is associated with a reduction in opioid use, and improved pain scores over a 24 hour period. Adequately powered studies are needed to determine the long term benefits of acute opioid reduction.
Keywords
IV acetaminophen; Analgesia; Surgery; OpioidsIntroduction
Opioids are the mainstay of treatment in patients with moderatesevere pain, however; they are associated with nausea, vomiting, constipation, sedation and respiratory depression [1,2]. It is necessary to consider other treatment options for pain so as to reduce Opioid consumption and minimize adverse effects [1,3]. The non-opioid analgesics available for post-operative use in patients are limited especially when the oral route for administration is not an option. The intravenous (IV) NSAIDs on the market include ketorolac and ibuprofen which are associated with bleeding and renal toxicity.The use of IV acetaminophen has been evaluated in several clinical trials and systematic reviews and has been compared to oral acetaminophen, NSAIDs, a pro-drug formulation of IV acetaminophen and placebo. These studies have shown that IV acetaminophen is an effective pain medication that can reduce the need for Opioids [1,4,5]. IV acetaminophen is currently approved in the United States for the management of mild to moderate pain, moderate to severe pain in conjunction with opioid analgesics and fever reduction. This formulation has a faster onset of action and therapeutic plasma concentrations are achieved within 20 minutes [6].
Atlanta Medical Center (AMC) recently added IV acetaminophen to its formulary but restricted its use to one dose in the operation room (OR) or in the post anesthesia care unit (PACU). Obesity is associated with an increased incidence of obstructive sleep apnea (OSA). Patients undergoing bariatric surgery who have OSA are sensitive to the depressant effects of Opioids [7]. Opioid reduction in this patient population has been shown in a small retrospective study evaluating the use of IV acetaminophen and comparing patients who received opioids to patients who received IV acetaminophen. A 37% reduction in opioid use was shown between groups [8]. In September 2012, the Pharmacy and Therapeutics (P&T) committee at AMC approved an extension of the use of IV acetaminophen from one dose intra-operatively to four doses over 24 hours for 30 patients undergoing bariatric surgery. In this study, patients who received 1 gram of IV acetaminophen in the OR were compared to patients who received IV acetaminophen dosed at 1 gram every 6 hours.
Methods
Study designIn this retrospective study, 60 bariatric surgery patients were divided into two groups: control and intervention. The control group included patients who received 1 gram of IV acetaminophen for one dose while the intervention group consisted of patients who received 1 ram every 6 hours over a 24 hour period. The research protocol was approved by the Institutional Review Board at AMC.
Study population
The patients included in the study were at least 18 years of age and underwent one of the following bariatric surgery procedures: laparascopic gastric bypass or laparascopic gastric sleeve at AMC. Patients were excluded if they were less than 18 years of age, pregnant, underwent a non-bariatric surgical procedure, allergic to opioids or acetaminophen, and had elevated liver enzymes at baseline or a history of alcohol abuse.
Outcomes
The primary outcome was the total amount of opioids used by both groups over a 24 hour period. The secondary outcomes were adverse events experienced by patients in both groups and pain severity assessed by pain scales. Patients were determined to have experienced any of the following side effects: nausea/vomiting, constipation and respiratory depression if it was noted in the progress note section of the charts or they received medications used to treat or reverse side effects. Pain was measured by numerical pain scales ranging from 0-10 depicting increasing pain severity.
Statistical analysis
All demographic information was examined using descriptive statistics (i.e. mean and standard deviation). Inferential statistics were used to examine differences between the control and intervention group. Specifically, the average pain score and average morphine equivalents were compared using the independent samples test while the adverse effects were compared using chi square test. A p-value of 0.05 or less was considered statistically significant.
Results
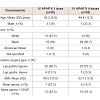
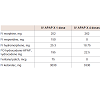
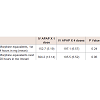
From April 1, 2012 to April 30, 2013, a total of 60 patients who underwent a bariatric surgery procedure were classified according to the number of doses of 1 gram of IV acetaminophen they received (Table 1). Every patient in the intervention group had written orders of IV acetaminophen 1 gram every 6 hours for 24 hours. One patient in the intervention group, however, was noted to have only received 3 doses of IV acetaminophen. All patients in both groups had orders for IV ketorolac 30 mg every 6 hours; either scheduled or as needed; except for one patient in the control group. The intervention group received 300 mg extra ketorolac than the control group (Table 2).
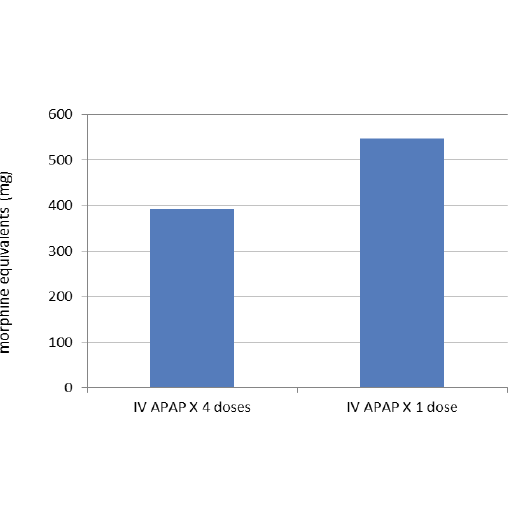
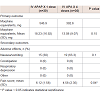
There was a 28.3% reduction in the total amount of morphine equivalents used by the patients in the intervention group compared to the control group (Figure 1). The average amount of morphine equivalents used by patients in the intervention group was 18.23 mg versus 13.08 mg in the control group (p = 0.15) (Table 3). All 60 patients had a length of stay in the post anesthesia care unit (PACU) after their procedure ranging from 2 to 6 hours before they were transferred to a medical/surgical floor. The average amount of morphine equivalents required by patients in the intervention group within the first four hours of the initial APAP dose was 6.57 mg versus 5.19 mg in the control group (p = 0.24). Over the next 20 hours, the average amount of morphine equivalents required was 6.52 mg and 13.14 mg in the intervention and control groups respectively (Table 4).
The adverse events experienced by patients in both groups were limited to nausea/vomiting which was seen in 19 patients in the intervention group compared to 15 patients in the control group (p= 0.1). The mean pain scores reported by patients in the intervention group was 4.58 versus 6.12 in the control group (p = 0.04) (Table 3).
Discussion
In this small, retrospective study, it was observed that the use of scheduled IV APAP can potentially reduce the amount of opioids required to control pain in patients undergoing bariatric surgery. The use of IV APAP was also associated with improved pain scores and a comparable side effect profile. Although no statistically significant difference was seen in average opioid consumption, it was observed that patients received more opioids while they were in the PACU and were in the PACU for 4 hours on average. The authors decided to break down the difference in opioid requirements between groups by classifying the patients based on the first four hours, and then the subsequent 20 hours. There is a clear trend toward significance in the amount of opioids consumed between groups when accounting for the time spent after the PACU stay. The authors also considered patients with sleep apnea; whether or not they required use of CPAP at home. This was done to determine whether there was any relationship between respiratory depression with opioids and sleep apnea. It can be inferred that there is no relationship because there were no cases of respiratory depression observed among the patients included in the study.Some limitations of the study include small sample size and lack of calculated power. Another limitation was the retrospective study design for which lack of information or poor record keeping was difficult to control. The results of this study may not be applicable to patients undergoing a surgical procedure associated with a more severe level of pain. The short window for the study may not have been sufficient to observe certain opioid adverse effects. The use of opioid reduction and pain scores as endpoints has been criticized because patients have varying levels of tolerance to opioids and a reduction in the amount of opioids used may not necessarily mean patient safety has been improved; and pain ratings are subjective [9]. It is essential to note that regardless of level of opioid tolerance, any patient may be at risk for opioid related side effects and it is best to minimize its use. The authors did not conduct a cost analysis for this project; however, studies show that the use of IV APAP will accrue a larger cost over time compared to its oral counterpart or no IV APAP at all.
In conclusion, in patients undergoing bariatric surgical procedures, IV APAP does not significantly reduce the amount of opioids required for pain control in the first 24 hours but improves patient pain scores. Adequately powered and prospective studies are needed to establish the long term benefits of acute opioid reduction.